Treating and Recovering from Knee Injuries
Introduction:
Knee injuries are an extremely common problem that can happen to athletes, weekend warriors, and even sedentary individuals. The knee joint is complex and vulnerable to various forms of trauma and overuse. Knee problems can develop at any age and affect day-to-day activities. This comprehensive guide covers the most prevalent knee injuries, their typical symptoms and diagnosis, all the treatment options available, as well as the rehabilitation process. Read on to learn how to identify knee issues, seek proper medical care, and safely return to activities after sustaining a knee injury.
Most Common Knee Injuries:
There are several injuries that frequently occur around the knee joint. These include sprains, strains, tears in ligaments or tendons, fractures, dislocations, and inflammatory conditions.
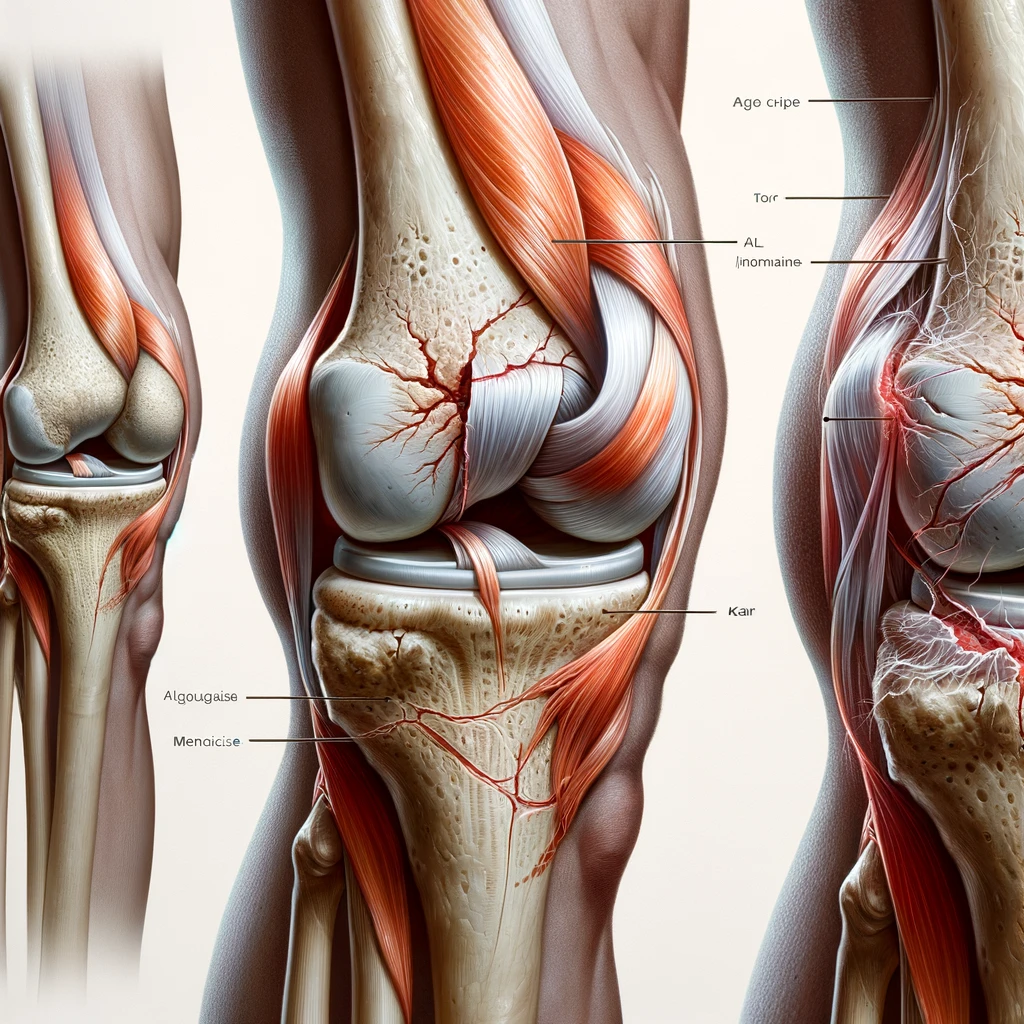
Knee sprains and strains involve overstretching or partial tears of the ligaments and tendons. The most commonly affected ligaments are the ACL, MCL, and LCL. Knee strains can happen to muscles like the quadriceps or hamstrings. These injuries cause pain, swelling, and instability in the knee.
More serious knee injuries involve complete tears of key ligaments like the anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL). Tears can also occur in shock-absorbing structures like the menisci cartilage or patellar tendon. Knee dislocations are when the knee cap slips out of position. Fractures around the knee may occur in the patella, tibia, or femur.
Inflammatory conditions like tendinitis, bursitis, and arthritis can develop over time with overuse or anatomical issues. Patellar tendinitis (jumper’s knee) involves irritation of the tendon below the kneecap. Bursitis affects the small fluid-filled sacs around the knee joint. Arthritis causes progressive cartilage damage and bone spur formation.
Causes and Risk Factors:
Knee injuries can result from sudden trauma or impact to the joint, like a sports tackle or fall. Twisting the knee forcefully can also damage ligaments. Prolonged overuse through repetitive motions, improper training, or imbalance in strength and flexibility increases injury risk. Some anatomical factors that predispose people include being bow-legged or knock-kneed, having flat feet, or a previous knee injury.
Signs and Symptoms:
– Pain – This may be focal or diffuse depending on the injury. Severe initial pain suggests serious trauma. Chronic, progressive pain indicates an overuse injury or degenerative arthritis.
– Swelling – Fluid accumulation indicates inflammation or bleeding inside the joint. Localized swelling affects specific structures.
– Instability – A feeling that the knee will buckle or give out. Significant instability points to ligament tears.
– Locking or catching – Impaired mobility suggesting loose cartilage or tears is blocking joint motion.
– Redness and warmth – The knee appears flushed and inflamed.
– Limited range of motion – The knee lacks full extension or flexion due to pain, swelling, or structural damage.
– Popping or crunching sounds – Results from cartilage and bone rubbing abnormally.
Diagnosis and Testing:
A physician gathers a medical history and performs a physical exam assessing knee range of motion, strength, alignment, swelling, and sites of pain. Imaging tests help evaluate soft tissue and bone structures. X-rays show fractures and arthritis. MRI scans visualize ligaments, tendons, and cartilage in detail. CT scans also assess bony anatomy. Joint fluid analysis under a microscope can identify inflammatory conditions. Assessing walking and alignment helps identify biomechanical issues.
Treatment Options:
– RICE – Rest, ice packs, compression, and elevating the knee reduces swelling and pain.
– Medications – Anti-inflammatories and targeted injections provide pain relief and reduce inflammation.
– Physical therapy – Exercises strengthen muscles, improve range of motion, and promote proprioception.
– Assistive devices – Braces, sleeves, crutches, or canes help immobilize and offload the knee.
– Surgery – Repairing torn ligaments or resurfacing damaged cartilage can restore function.
– Alternative medicine – Treatments like acupuncture, massage, cryotherapy, or prolotherapy may augment conventional care.
Rehabilitation and Recovery:
The initial rehab goals are to control pain and swelling while regaining passive knee mobility. Later, the focus shifts to building muscle strength, endurance, and stability. Sport-specific drills prepare the patient for returning to full activity. Recovery timelines vary based on the injury. Most knee issues require at least 4-6 weeks of rehab. Severe ligament tears may need 3-9 months. Patience during rehab is key to prevent re-injury.
Outlook and Prevention:
With appropriate treatment, most knee injuries can fully recover within 3-12 months depending on severity. However, some may lead to lasting issues like osteoarthritis later in life. Preventive measures include building muscular strength, proprioception, and flexibility through training. Use proper technique when exercising. Wear protective knee pads if necessary. Taping or bracing can also stabilize vulnerable knees during activities.
Conclusion:
Knee injuries are diverse, encompassing everything from minor sprains to severe fractures and ligament tears. Prompt diagnosis and treatment tailored to the specific injury leads to an optimal recovery. A well-structured rehabilitation program further helps restore knee mobility and strength. While knees are susceptible to injury, focusing on prevention and prompt care when problems arise allows most people to return to an active lifestyle.









