Welcome to our comprehensive guide on knee osteoarthritis. In this article, we will provide you with in-depth knowledge about this whole joint disease, its causes, symptoms, and treatment options. Whether you are experiencing joint pain or simply want to learn more about the knee joint, we’ve got you covered.
Knee osteoarthritis is a common condition that affects the knee joint, resulting in joint pain, stiffness, and swelling. It primarily affects the elderly population but can also occur due to previous joint trauma or other underlying conditions such as rheumatoid arthritis. Understanding the complexities of knee osteoarthritis is crucial in managing the condition effectively.
In this article, we will explore the etiology and pathophysiology of knee osteoarthritis, including the factors that contribute to its development. We will discuss the clinical presentation of knee osteoarthritis, highlighting the common symptoms and physical examination findings. Additionally, we will delve into the risk factors associated with knee osteoarthritis and its prevalence among different demographics.
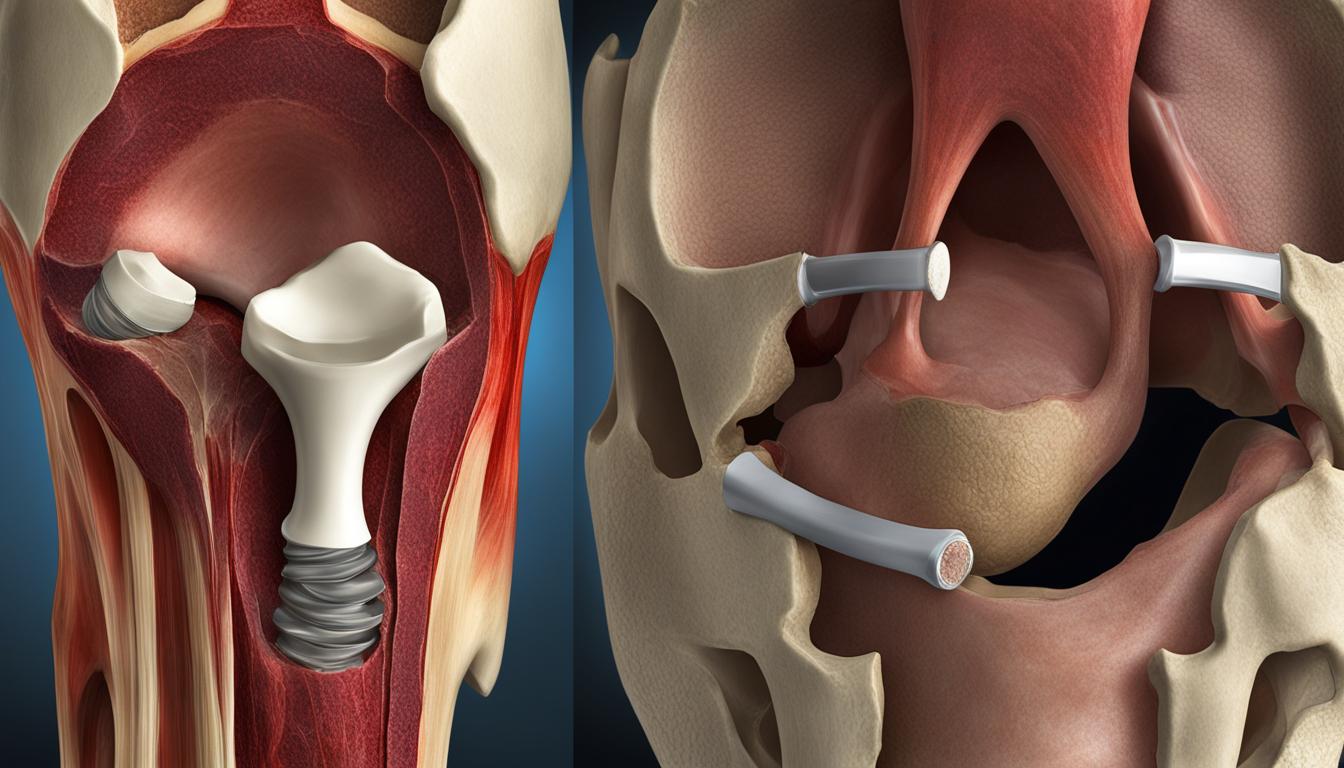
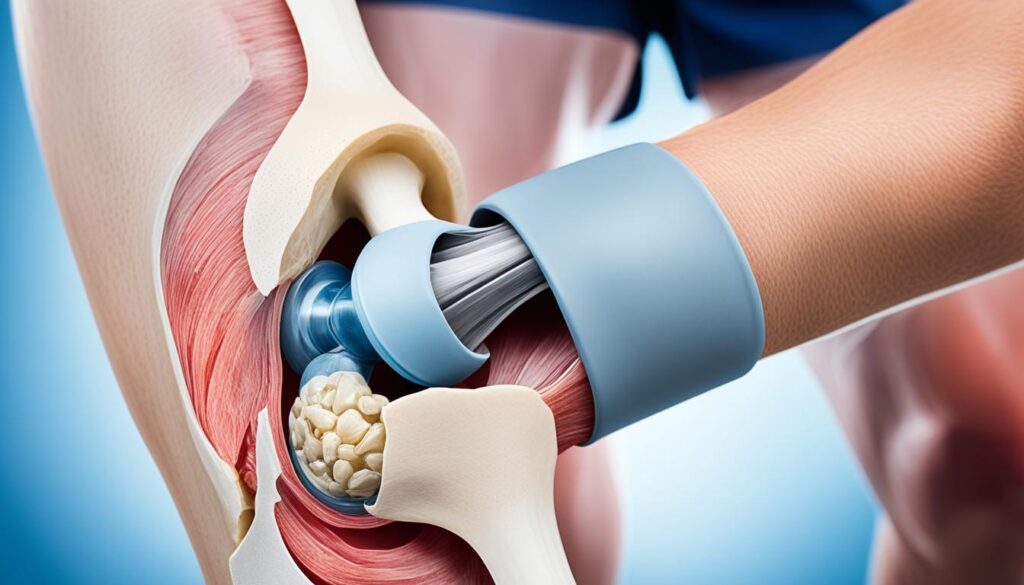
Finally, we will provide an overview of the various treatment options available for knee osteoarthritis. From conservative methods that focus on lifestyle modifications, physical therapy, and medications to surgical interventions such as arthroscopy or joint replacement, we will guide you through the possible strategies for managing knee osteoarthritis.
By the end of this article, we hope to equip you with the knowledge needed to understand knee osteoarthritis and make informed decisions about your joint health. So, let’s dive in and explore the fascinating world of knee osteoarthritis together!
Etiology of Knee Osteoarthritis
Knee osteoarthritis can be classified into primary and secondary based on its cause. Primary osteoarthritis refers to the degeneration of the articular cartilage without any known reason, often associated with aging and wear and tear. Secondary osteoarthritis, on the other hand, is caused by specific factors such as joint trauma, abnormal joint alignment, or other underlying conditions like rheumatoid arthritis.
Understanding the etiology of knee osteoarthritis is crucial for appropriate management and treatment. By identifying whether the osteoarthritis is primary or secondary, healthcare professionals can personalize the treatment approach and address the underlying factors contributing to the condition.
| Primary Osteoarthritis | Secondary Osteoarthritis |
|---|---|
| Osteoarthritis without any known cause | Caused by joint trauma, abnormal joint alignment, or underlying conditions like rheumatoid arthritis |
| Associated with natural aging and wear and tear | Triggered by specific factors other than natural aging |
| Gradual onset and progression | Can occur suddenly or progress rapidly depending on the underlying cause |
| Occurs in the absence of any identifiable risk factors | Often associated with identifiable risk factors or a history of joint trauma |
Identifying the etiology of knee osteoarthritis helps healthcare professionals tailor treatment plans that address the root cause of the condition, improving patient outcomes and quality of life.
Epidemiology of Knee Osteoarthritis
Knee osteoarthritis is a widespread condition with a significant impact on individuals and societies. Understanding the epidemiology of knee osteoarthritis is vital for healthcare professionals in providing appropriate care and identifying preventive measures. Let’s take a closer look at the prevalence, age distribution, and gender differences associated with knee osteoarthritis.
Prevalence:
Knee osteoarthritis affects a substantial portion of the population globally. Studies have shown that its prevalence is increasing due to various factors such as aging populations and the rising rates of obesity. According to the World Health Organization, knee osteoarthritis is one of the leading causes of disability worldwide.
Age Distribution:
The prevalence of knee osteoarthritis increases with age, with a higher incidence observed among older adults. While knee osteoarthritis can develop at any age, it becomes more common as people grow older. In fact, a significant percentage of individuals over the age of 60 experience symptomatic knee osteoarthritis, highlighting the importance of effective management strategies for this age group.
Gender Differences:
Knee osteoarthritis affects both men and women; however, there is a notable gender difference in its prevalence. Research studies have consistently shown that women are more likely to develop knee osteoarthritis compared to men. This gender disparity may be attributed to hormonal differences, genetic factors, and variations in joint anatomy and biomechanics.
To provide a comprehensive understanding of the epidemiology of knee osteoarthritis, let’s take a closer look at the affected joints and the relationship between radiographic evidence and clinical symptoms.
Pathophysiology of Knee Osteoarthritis
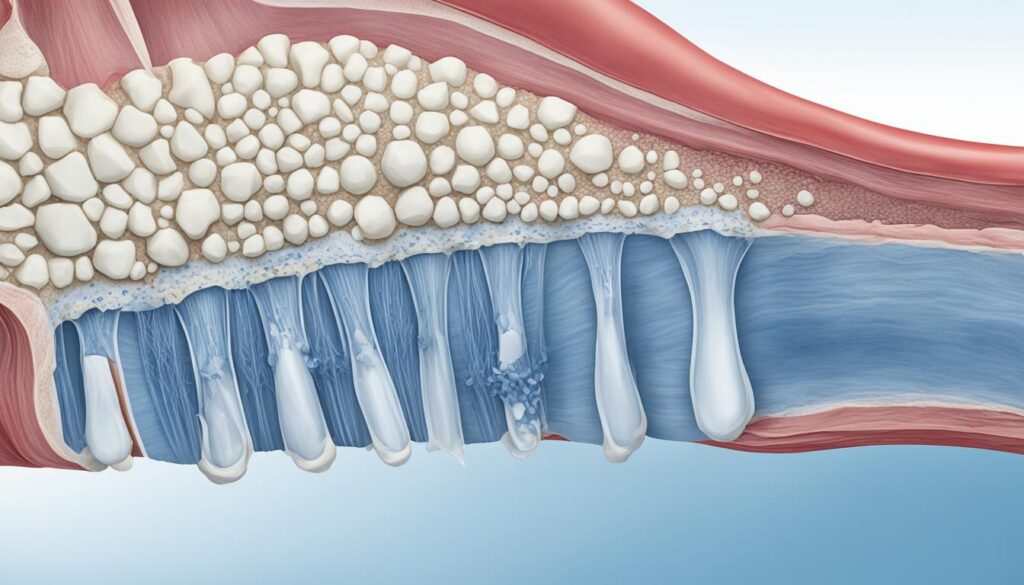
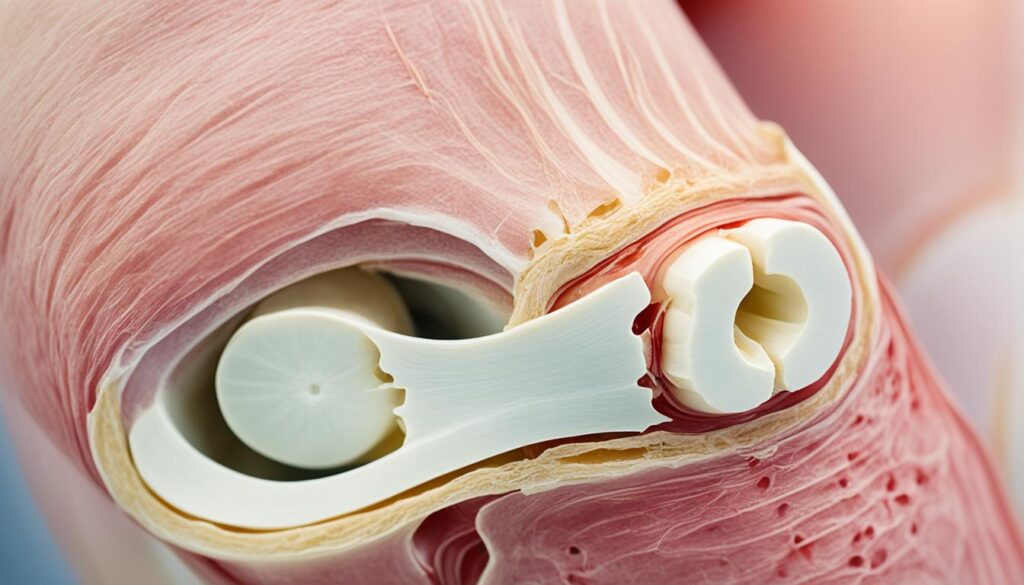
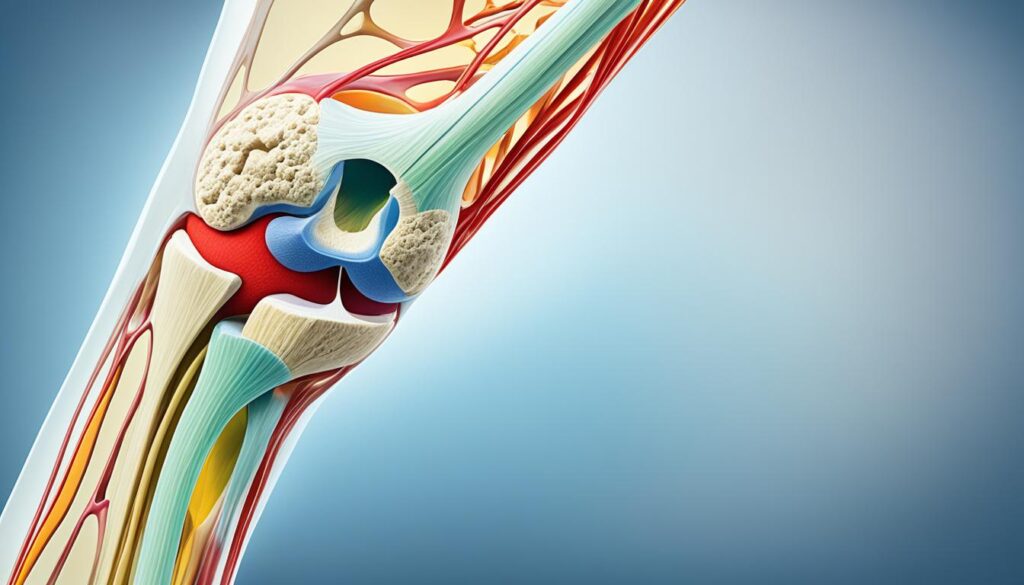
The pathophysiology of knee osteoarthritis involves the disruption of the articular cartilage within the knee joint. Articular cartilage is a specialized connective tissue that covers the ends of bones and allows for smooth joint movement. It is primarily composed of collagen, proteoglycans, and chondrocytes.
In knee osteoarthritis, there is an imbalance between cartilage degradation and synthesis, leading to the progressive loss of collagen and proteoglycans. Collagen provides structural support and strength to the cartilage, while proteoglycans help to retain water and maintain cartilage hydration. The gradual loss of these essential components in knee osteoarthritis disrupts the integrity and function of the articular cartilage.
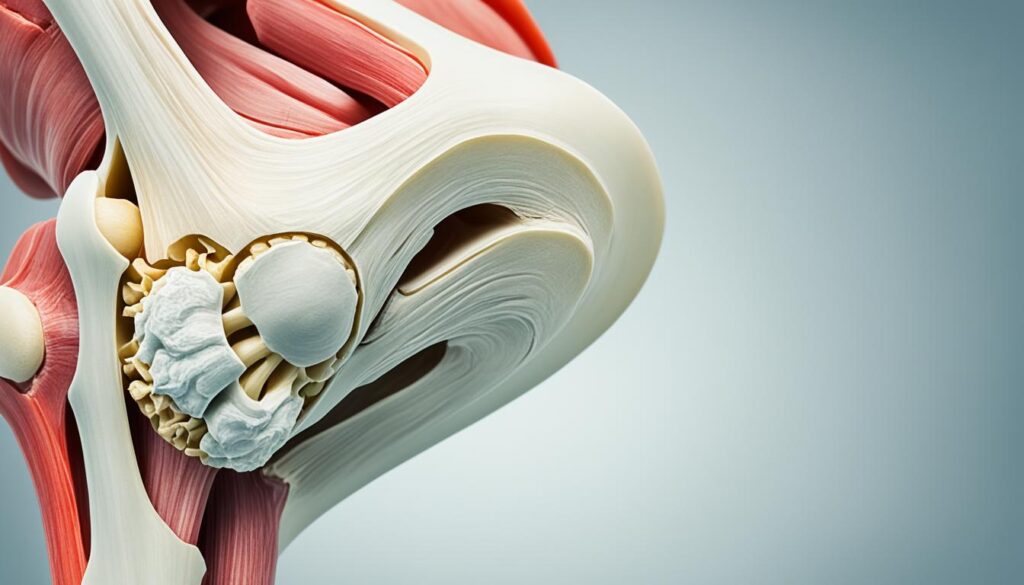
The degradation of collagen and proteoglycans in knee osteoarthritis results in the disorganization of the cartilage matrix, increased water content, and ultimately, erosion of the articular surface. This leads to the development of joint symptoms such as pain, stiffness, and reduced range of motion. Various enzymes, such as matrix metalloproteases, are implicated in the degradation of the cartilage in knee osteoarthritis.
The Role of Matrix Metalloproteases
Matrix metalloproteases (MMPs) are a group of enzymes that play a crucial role in the breakdown of extracellular matrix components, including collagen and proteoglycans. In knee osteoarthritis, the activity of MMPs becomes dysregulated, leading to excessive degradation of the articular cartilage. This imbalance between cartilage breakdown and repair mechanisms contributes to the progressive loss of joint function and the development of knee osteoarthritis symptoms.
“The disruption of articular cartilage in knee osteoarthritis involves an imbalance between cartilage degradation and synthesis, leading to the loss of collagen and proteoglycans. Various enzymes, such as matrix metalloproteases, play a role in cartilage degradation.”
Understanding the pathophysiology of knee osteoarthritis is essential for developing targeted therapeutic strategies that can slow down its progression, preserve joint function, and alleviate symptoms. By addressing the underlying mechanisms involved in cartilage degradation and promoting cartilage repair, it may be possible to improve the management of knee osteoarthritis and enhance the quality of life for individuals affected by this condition.
Clinical Presentation of Knee Osteoarthritis
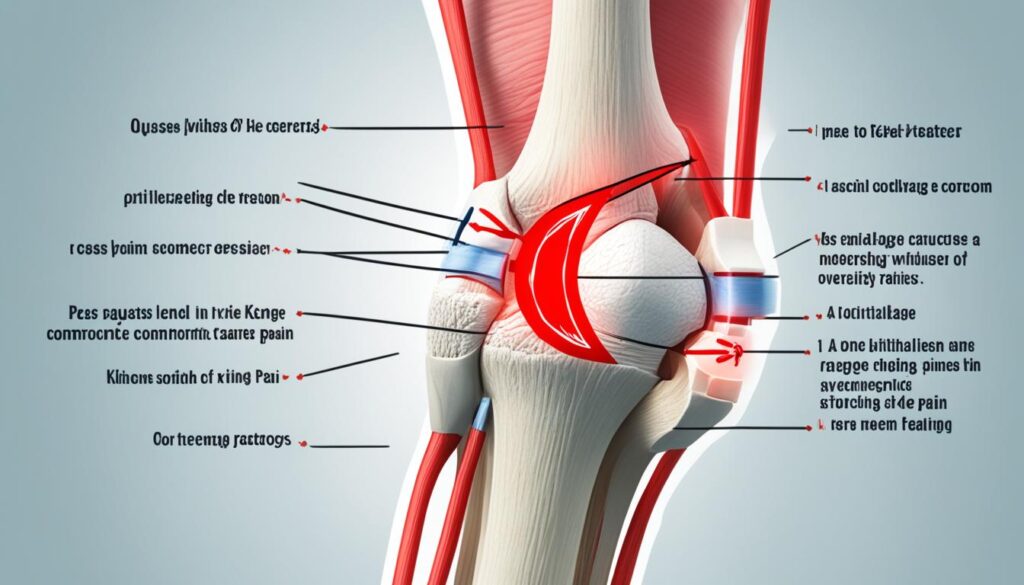
Knee osteoarthritis is characterized by several clinical symptoms that aid in its diagnosis and management. These symptoms include knee pain, stiffness, and swelling. The pain experienced by individuals with knee osteoarthritis is typically gradual in onset and worsens with activities such as walking, repetitive bending, and prolonged sitting. It is important to note that knee pain can vary in intensity, ranging from mild discomfort to severe, debilitating pain.
In addition to pain, stiffness is a common symptom of knee osteoarthritis. Individuals may experience difficulty in moving the knee joint, especially after periods of rest or inactivity. This stiffness may improve with movement and physical activity.
Swelling, also known as joint effusion, can occur in knee osteoarthritis. It is often characterized by localized swelling around the knee joint, which may be accompanied by redness and warmth. This swelling is primarily due to the accumulation of fluid within the joint space.
During a physical examination, healthcare professionals may assess various signs related to knee osteoarthritis. These can include periarticular erythema and swelling, indicating inflammation in the surrounding tissues. The examination may also reveal muscle atrophy, which is a result of reduced muscle strength and usage due to knee pain and limited mobility.
Furthermore, healthcare professionals may evaluate the alignment of the knee joint. Varus or valgus deformities, in which the knee joint deviates inward or outward, may be present in individuals with knee osteoarthritis.
Range of motion testing and palpation of the knee joint are significant components of the physical examination. These techniques help assess the flexibility, stability, and overall health of the knee joint.
Overall, a thorough understanding of the clinical presentation of knee osteoarthritis is essential in making an accurate diagnosis and developing an appropriate management plan. By recognizing and addressing the specific symptoms and signs associated with knee osteoarthritis, healthcare professionals can improve the quality of life for individuals with this condition.

Risk Factors and Prevalence of Knee Osteoarthritis
In order to understand the development and prevalence of knee osteoarthritis, it is important to consider the various risk factors associated with this condition. These risk factors include:
- Joint trauma
- Obesity
- Metabolic syndrome
- Genetic factors
- Age
Obesity, in particular, is a significant risk factor for knee osteoarthritis. The excess weight places increased mechanical stress on the knee joint, leading to accelerated wear and tear of the articular cartilage. Additionally, occupations that involve prolonged standing and repetitive knee bending can also contribute to the development of knee osteoarthritis.
Prevalence studies have consistently shown that knee osteoarthritis is more common in women and tends to increase with age. This may be attributed to hormonal differences and the cumulative effects of joint use over time.
To better address the risk factors and prevalence of knee osteoarthritis, preventive measures and targeted interventions play a crucial role. By understanding these factors, we can implement strategies to reduce the incidence and impact of this condition on individuals’ quality of life.
Key Takeaways:
- Risk factors for knee osteoarthritis include joint trauma, obesity, metabolic syndrome, genetic factors, and age.
- Obesity is a significant risk factor due to increased mechanical stress on the knee joint.
- Knee osteoarthritis is more common in women and tends to increase with age.
- Preventive measures and targeted interventions are essential to address these risk factors and reduce the incidence of knee osteoarthritis.
| Risk Factors | Prevalence |
|---|---|
| Joint trauma | – |
| Obesity | – |
| Metabolic syndrome | – |
| Genetic factors | – |
| Age | – |
Conclusion
In conclusion, effective management of knee osteoarthritis is crucial for maintaining joint health and improving the quality of life for individuals affected by this condition.
Conservative methods such as lifestyle modifications, physical therapy, and medications play a key role in the initial treatment of knee osteoarthritis. By implementing these strategies, individuals can reduce pain, improve joint flexibility, and slow down the progression of the disease.
However, in cases where conservative treatments fail to provide sufficient relief, surgical options such as arthroscopy or joint replacement may be considered. These surgical interventions aim to provide long-term pain relief and restore joint function.
By understanding the etiology, pathophysiology, clinical presentation, and risk factors of knee osteoarthritis, healthcare professionals can develop individualized treatment plans to effectively manage this condition. Through a collaborative approach, we can improve knee osteoarthritis management, promote joint health, and enhance the overall well-being of patients.
FAQ
What is knee osteoarthritis?
Knee osteoarthritis, also known as degenerative joint disease of the knee, is a common condition that results from the gradual loss of articular cartilage within the knee joint. It is a whole joint disease that primarily affects elderly individuals.
What are the symptoms of knee osteoarthritis?
Symptoms of knee osteoarthritis include gradual onset knee pain, stiffness, and swelling. The pain worsens with activity and repetitive bending and is often aggravated by prolonged sitting. The symptoms of knee osteoarthritis progress over time.
What are the treatment options for knee osteoarthritis?
Treatment options for knee osteoarthritis range from conservative methods to surgical interventions, depending on the severity of the condition. Conservative treatment may include lifestyle modifications, physical therapy, and medications. In cases where conservative treatment fails, surgical options such as arthroscopy or joint replacement may be considered.
What are the risk factors for knee osteoarthritis?
Risk factors for knee osteoarthritis include joint trauma, obesity, metabolic syndrome, genetic factors, and age. Obesity is a significant risk factor due to the increased mechanical stress placed on the knee joint. Occupations involving prolonged standing and repetitive knee bending also contribute to the development of knee osteoarthritis.
Who is at a higher risk of developing knee osteoarthritis?
Knee osteoarthritis is more common in women and tends to increase with age. The prevalence of knee osteoarthritis increases significantly among individuals over the age of 60. However, not all individuals with radiographic evidence of knee osteoarthritis experience symptoms.
What is the pathophysiology of knee osteoarthritis?
Knee osteoarthritis involves the disruption of the articular cartilage within the knee joint. There is an imbalance between cartilage degradation and synthesis, leading to the loss of collagen and proteoglycans. This results in the disorganization of cartilage and erosion of the articular surface.
How is knee osteoarthritis diagnosed?
Knee osteoarthritis is diagnosed based on clinical symptoms such as knee pain, stiffness, and swelling. Physical examination, including range of motion testing and palpation of the knee joint, is essential. Radiographic findings may also aid in the diagnosis, but they do not always correlate with clinical presentation.