

Osteoporosis, often called the “silent disease,” is a condition characterized by decreased bone density and deterioration of bone tissue, leading to increased fragility and risk of fractures. The condition affects approximately 1 in 3 women and 1 in 5 men over the age of 50, making it a significant public health concern worldwide. The impact of osteoporosis extends beyond bone health – hip fractures, in particular, are associated with a 3-4 times greater risk of dying within 12 months compared to the general population of the same age.
Throughout our lives, our bones undergo a continuous process of remodeling, with old bone being removed (resorption) and new bone being formed. In healthy individuals, this process maintains a balance. However, in osteoporosis, bone resorption outpaces bone formation, resulting in a net loss of bone mass and structural deterioration.
The good news is that osteoporosis is both preventable and treatable. While conventional medical treatments play a crucial role in managing the disease, especially for those at high fracture risk, natural approaches can complement these treatments and provide additional benefits for bone health. This article explores the full spectrum of osteoporosis management, from medical interventions to evidence-based natural therapies that can help strengthen bones and reduce fracture risk.
By understanding both conventional treatments and natural approaches, individuals can work with their healthcare providers to develop a comprehensive strategy tailored to their specific needs and risk factors.

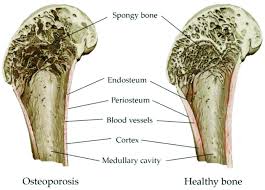
To effectively address osteoporosis, it’s important to understand the disease process and the factors that contribute to its development. At its core, osteoporosis occurs when the body loses too much bone, makes too little bone, or both. This results in weakened bones that can break from minor falls or, in serious cases, even from simple actions like sneezing or bumping into furniture.
Several risk factors contribute to the development of osteoporosis:
Osteoporosis is typically categorized as either primary or secondary. Primary osteoporosis is related to aging and hormonal changes, while secondary osteoporosis results from specific medical conditions or medications that affect bone metabolism.
Diagnosis typically involves dual-energy X-ray absorptiometry (DEXA scan), which measures bone mineral density (BMD). The results are presented as a T-score, comparing an individual’s bone density to that of a healthy 30-year-old of the same sex. A T-score of -1.0 or above is considered normal, while scores between -1.0 and -2.5 indicate osteopenia (low bone mass), and scores below -2.5 indicate osteoporosis.
The Fracture Risk Assessment Tool (FRAX) may also be used to predict the 10-year probability of a major osteoporotic fracture based on individual risk factors, with or without BMD measurements.
One of the challenges of osteoporosis is that it progresses silently, often without symptoms until a fracture occurs. This makes screening and preventive measures crucial, especially for those with known risk factors.
Modern medicine offers several effective treatments for osteoporosis, designed to reduce fracture risk by slowing bone loss, increasing bone formation, or both. Treatment recommendations typically consider factors such as age, sex, fracture history, bone density measurements, and overall fracture risk.
Bisphosphonates remain the most commonly prescribed first-line treatment for osteoporosis. These medications slow bone resorption by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone. The American College of Physicians (ACP) recommends bisphosphonates as the initial pharmacologic treatment for reducing fracture risk in postmenopausal women with osteoporosis.
Common bisphosphonates include:
These medications have been shown to reduce the risk of vertebral fractures by 40-70% and non-vertebral fractures, including hip fractures, by 20-40%. Side effects can include gastrointestinal issues with oral formulations and flu-like symptoms with intravenous formulations. Rare but serious side effects include osteonecrosis of the jaw and atypical femur fractures, particularly with long-term use.
When bisphosphonates are not appropriate or effective, several second-line treatments are available:
Denosumab (Prolia) is a RANK ligand inhibitor that blocks the development and activity of osteoclasts. Given as a subcutaneous injection every six months, it has been shown to reduce vertebral, non-vertebral, and hip fractures. Unlike bisphosphonates, denosumab does not accumulate in the bone, so its effects reverse quickly if treatment is stopped, potentially leading to rapid bone loss and increased fracture risk if not properly managed.
Selective Estrogen Receptor Modulators (SERMs) such as raloxifene (Evista) mimic estrogen’s beneficial effects on bone without some of the risks associated with estrogen. They can reduce vertebral fracture risk but have not been shown to reduce non-vertebral or hip fracture risk.
Hormone Replacement Therapy (HRT) was once widely used for osteoporosis prevention but is now primarily recommended for managing menopausal symptoms in women at high risk for osteoporosis, and only for the shortest duration possible due to potential risks of breast cancer, heart disease, and stroke.
For patients with severe osteoporosis or those who have experienced fractures despite other treatments, more potent options are available:
Anabolic Therapies stimulate bone formation rather than simply slowing bone loss. These include:
These medications can increase bone density more substantially than antiresorptive drugs, especially at the spine. However, they are typically reserved for those at very high fracture risk due to their cost, route of administration, and limited treatment duration.
The optimal duration of osteoporosis treatment continues to be studied. Many experts recommend reassessing after 3-5 years of bisphosphonate therapy, with consideration of a “drug holiday” for patients whose fracture risk has decreased. For high-risk patients, sequential therapy (starting with an anabolic agent followed by an antiresorptive) may provide optimal fracture protection.
Regular monitoring of bone mineral density and, in some cases, biochemical markers of bone turnover, can help assess treatment response and guide decisions about continuing or modifying therapy.
It’s important to remember that medication is just one component of osteoporosis management. All treatment approaches should be accompanied by adequate calcium and vitamin D intake, appropriate exercise, and measures to prevent falls.
Nutrition plays a fundamental role in both preventing and managing osteoporosis. While medications can effectively slow bone loss or stimulate bone formation, they cannot compensate for nutritional deficiencies that compromise bone health. A bone-healthy diet provides the essential building blocks needed for optimal bone remodeling and maintenance.
Calcium is the primary mineral found in bone, making adequate intake essential throughout life. The recommended daily intake varies by age and gender:
Dietary sources of calcium include:
While food sources are preferred, calcium supplements can help bridge dietary gaps. Two main types are available:
For optimal absorption, calcium supplements should be taken in doses of 500-600 mg or less at a time, spaced throughout the day. Taking them with meals can reduce the risk of kidney stones and improve absorption, particularly for calcium carbonate.
Vitamin D is crucial for calcium absorption and proper bone mineralization. Without adequate vitamin D, the body cannot effectively utilize calcium, regardless of intake. Current recommendations include:
Vitamin D sources include:
Many healthcare providers recommend checking vitamin D levels through a blood test (25-hydroxyvitamin D) to determine if supplementation is needed. Optimal levels are generally considered to be 30-60 ng/mL.
While calcium and vitamin D receive the most attention, other nutrients also contribute to bone health:
Certain dietary patterns may also impact bone health. The Mediterranean diet, rich in fruits, vegetables, whole grains, fish, olive oil, and nuts, has been associated with higher bone density and lower fracture risk.
Conversely, some dietary factors may negatively affect bone health:
Exercise is a powerful tool for building and maintaining bone strength. Unlike medication, which primarily works to slow bone loss, appropriate physical activity can actually stimulate bone formation, improve balance and coordination (reducing fall risk), and enhance overall functional capacity.
Bones respond to mechanical loading much like muscles respond to resistance – they adapt and strengthen. This phenomenon, known as Wolff’s Law, explains why weight-bearing activities and resistance training are particularly beneficial for bone health. When muscles pull on bones during these activities, they create stress that stimulates osteoblasts (bone-building cells) to lay down new bone tissue.
Different types of exercise affect bone health in different ways:
Weight-bearing exercises force you to work against gravity while staying upright. These activities are particularly effective for strengthening the bones of the hips, legs, and lower spine. They include:
A general recommendation is to engage in weight-bearing aerobic activities for 30 minutes on most days of the week.
Resistance or strength training involves working against resistance, whether from weights, bands, water, or body weight. These exercises target specific muscle groups and the bones they attach to. Effective resistance training for bone health includes:
Resistance training should be performed 2-3 times per week, targeting all major muscle groups. For bone health benefits, moderate intensity (8-12 repetitions with a weight that creates fatigue by the final repetition) is generally recommended.
While these exercises don’t directly build bone, they help prevent falls – a critical consideration for those with osteoporosis:
Balance exercises should be incorporated into daily routines, even if just for a few minutes each day.
For those already diagnosed with osteoporosis, exercise remains beneficial but requires certain precautions:
An ideal exercise program for bone health includes:
For those new to exercise or with health concerns, starting with a physical therapist or qualified fitness professional experienced in working with osteoporosis is recommended. They can design a program tailored to individual needs, limitations, and goals.
Remember that consistency is key – the bone benefits of exercise are lost when activity stops, so finding enjoyable activities that can be maintained long-term is essential for ongoing bone health.
Vitamin K has emerged as an important nutrient for bone health that often doesn’t receive the same attention as calcium and vitamin D. Research increasingly suggests that adequate vitamin K intake is essential for optimal bone metabolism and strength.
Vitamin K serves as a cofactor for the enzyme that activates osteocalcin, a protein that binds calcium to the bone matrix. Without sufficient vitamin K, osteocalcin remains inactive, leading to reduced bone mineralization and potentially increased fracture risk.
There are two main forms of vitamin K:
Studies have found that higher vitamin K intake is associated with higher bone mineral density and lower fracture risk. Low circulating levels of vitamin K have been linked to lower bone mass and increased fracture risk, particularly hip fractures.
The best food sources of vitamin K include:
The adequate intake (AI) for vitamin K is:
However, optimal amounts for bone health may be higher than these basic recommendations.
Research on vitamin K supplementation for osteoporosis has shown mixed results. Some studies, particularly those using vitamin K2 (MK-4 form) at doses of 45mg daily, have shown reduced fracture risk in Japanese populations. Other studies using different forms or lower doses have shown more modest or inconsistent effects.
When considering vitamin K supplementation:
While the evidence for vitamin K supplementation is promising, it’s not yet conclusive enough for most major medical organizations to recommend routine supplementation specifically for osteoporosis. Current approaches include:
For those interested in supplementation, consulting with a healthcare provider is essential, particularly for those on medications that might interact with vitamin K.
Magnesium is an essential mineral that plays multiple roles in bone health yet is often overlooked in discussions about osteoporosis prevention and treatment. Approximately 60% of the body’s magnesium is stored in bone tissue, highlighting its importance to skeletal structure.
Magnesium contributes to bone health through several mechanisms:
Research has found that magnesium deficiency is associated with reduced bone mineral density, altered bone and mineral metabolism, and increased fracture risk. One study found that 40% of women with osteoporosis or low bone density had low circulating magnesium levels.
The recommended dietary allowance (RDA) for magnesium is:
Excellent food sources of magnesium include:
Despite its abundance in whole foods, many people don’t consume enough magnesium due to dietary patterns high in processed foods, which typically contain little magnesium. Soil depletion of minerals may also reduce the magnesium content of foods compared to historical levels.
For those who cannot meet their magnesium needs through diet alone, supplements can be beneficial. Several forms are available, each with different properties:
When supplementing, it’s generally recommended to start with a lower dose and gradually increase to avoid digestive discomfort. Taking magnesium supplements with food can also improve tolerance.
While magnesium is generally safe, excessive intake from supplements (not food) can cause diarrhea, nausea, and abdominal cramping. In people with reduced kidney function, high doses of magnesium supplements can lead to magnesium toxicity, characterized by low blood pressure, confusion, and cardiac complications.
Those with kidney disease, heart problems, or on certain medications should consult their healthcare provider before supplementing with magnesium.
While more research is needed on the specific effects of magnesium supplementation on fracture risk, ensuring adequate magnesium intake is a sensible strategy for supporting bone health. The greatest benefits are likely to be seen in those who are magnesium deficient.
Current recommendations include:
The dramatic increase in osteoporosis risk that follows menopause highlights the crucial role of estrogen in maintaining bone health. As estrogen levels decline, bone resorption accelerates, often leading to significant bone loss in the first 5-7 years after menopause. This connection between estrogen and bone health has led researchers to investigate plant compounds with estrogen-like properties, known as phytoestrogens, as potential natural therapies for osteoporosis.
Isoflavones are a class of phytoestrogens – plant compounds that have a structure similar to human estrogen and can bind to estrogen receptors in the body, though their effects are typically much weaker than those of human estrogen. The most well-studied isoflavones include:
These compounds are found primarily in soybeans and soy products, but also in smaller amounts in other legumes such as chickpeas, lentils, and beans.
Isoflavones may support bone health through several mechanisms:
Research on soy isoflavones for bone health has shown promising but mixed results:
A meta-analysis of 19 studies in postmenopausal women found that soy isoflavone supplementation significantly increased bone mineral density by 54% and reduced bone resorption markers by 23% compared to baseline values. The most significant benefits were seen in studies lasting at least one year and using higher doses (80-90 mg of isoflavones daily).
However, not all studies have shown positive results, and the effects may vary based on factors such as:
The richest food sources of isoflavones include:
The isoflavone content varies widely among soy foods, with whole and minimally processed soy foods generally providing higher amounts than highly processed soy ingredients.
For those considering isoflavone supplements for bone health:
While moderate consumption of dietary soy is generally considered safe for most people, questions have been raised about the long-term safety of isolated isoflavone supplements, particularly for women with a history of hormone-sensitive conditions such as breast cancer.
Current evidence does not indicate that moderate soy consumption increases breast cancer risk, and some studies suggest it may even be protective. However, the effects of high-dose isoflavone supplements taken for extended periods are less well understood.
Potential side effects of isoflavone supplements may include:
Given the current evidence:
As research continues, our understanding of the optimal use of isoflavones for bone health will likely evolve.
Beyond nutrition and targeted supplements, several lifestyle modifications can significantly impact bone health and fracture risk. These changes, while sometimes overlooked, can be powerful components of a comprehensive approach to osteoporosis prevention and management.
Smoking has multiple detrimental effects on bone health:
Studies have consistently shown that smokers have lower bone density and higher fracture risk compared to non-smokers. The longer one smokes, the greater the impact on bone health.
The good news is that quitting smoking can help slow the rate of bone loss, though it may not fully reverse existing damage. Former smokers gradually see their fracture risk decrease after quitting, though it may take years to approach the risk level of people who never smoked.
Resources for quitting smoking include nicotine replacement therapies, prescription medications, counseling programs, and support groups. Healthcare providers can help develop a personalized smoking cessation plan.
Excessive alcohol consumption negatively impacts bone health through multiple mechanisms:
Moderate alcohol consumption (up to one drink daily for women and up to two drinks daily for men) has not been clearly associated with increased osteoporosis risk. However, heavy drinking significantly increases the risk of bone loss and fractures.
For those who drink heavily, reducing alcohol consumption or abstaining completely can help preserve bone mass and reduce fracture risk. Support is available through healthcare providers, counseling, and programs like Alcoholics Anonymous.
For those with osteoporosis, preventing falls is crucial for avoiding fractures. Comprehensive fall prevention includes:
Home Safety Modifications:
Personal Safety Measures:
Health Management:
Emerging research suggests that chronic stress may contribute to bone loss through several mechanisms:
Effective stress management techniques include:
Incorporating stress reduction into daily routines can support overall health, including bone health.
Maintaining a healthy weight is important for bone health:
Achieving and maintaining a healthy weight through nutritious eating and regular physical activity supports optimal bone health and reduces fracture risk.
The most effective approach to osteoporosis prevention and treatment often combines conventional medical treatments with natural therapies. This integrated strategy addresses the condition from multiple angles, potentially providing more comprehensive protection against bone loss and fractures than either approach alone.
An optimal osteoporosis management plan typically includes:
The optimal combination of treatments varies based on individual factors:
Effective osteoporosis management requires collaboration with healthcare providers, potentially including:
Open communication about all therapies being used, including supplements and exercise programs, is essential to avoid potential interactions and ensure complementary rather than conflicting approaches.
Some natural therapies may interact with osteoporosis medications or other treatments:
Discussing all supplements with healthcare providers helps minimize the risk of adverse interactions.
Regular assessment helps determine whether the treatment plan is working:
Based on these assessments, the treatment plan can be adjusted to optimize outcomes.
Osteoporosis is a complex condition that requires a multifaceted approach to prevention and treatment. While conventional medical treatments play a crucial role, especially for those at high fracture risk, natural therapies can significantly complement these approaches and provide additional benefits for bone health.
The six natural therapies discussed – nutrition, exercise, vitamin K, magnesium, soy isoflavones, and lifestyle modifications – each address different aspects of bone health. When combined appropriately and personalized to individual needs, they create a comprehensive strategy that supports both bone quantity (density) and quality (structure).
The most effective approach is typically one that integrates conventional and natural strategies based on individual risk factors, preferences, and needs. This may mean using medications for those at high fracture risk while simultaneously optimizing nutrition, incorporating appropriate exercise, and addressing lifestyle factors that affect bone health.
For those at lower risk, focusing primarily on natural approaches may be appropriate, with regular monitoring to ensure bone health is maintained. The key is early intervention – whether through natural or conventional means – as preventing bone loss is easier than reversing it once significant deterioration has occurred.
Working collaboratively with healthcare providers to develop and adjust your bone health strategy over time ensures that you receive the most appropriate combination of treatments for your specific situation. With this comprehensive approach, many individuals can maintain bone strength, reduce fracture risk, and continue to lead active, independent lives despite osteoporosis.
Find the perfect knee brace for your specific condition with our comprehensive Knee Brace Selection…
Experiencing outer knee pain? Learn the specific symptoms of a torn meniscus outside knee, how…
Relieve IT band pain with these proven Iliotibial Band Syndrome exercises with pictures. Learn step-by-step…
Learn about the causes, treatments, and prevention of knee pain behind knee when bending and…
Discover the best heating pad for knee arthritis with our comprehensive guide. Compare top-rated options…
Discover the causes of knee pain that comes and goes walking, learn to differentiate between…