
Did you know that the patella, commonly known as the kneecap, is the largest sesamoid bone in the human body? This seemingly small but mighty bone holds immense significance for our mobility and protection, serving as the anchor point for crucial tendons and ligaments.
Join us as we explore the intricate position and function of the patella in the human body. From its unique anatomy to the development variations and common conditions affecting it, we’ll uncover the secrets of this important bone. Discover where the patella is located within our bodies, how it contributes to knee extension, and how it protects the knee joint from friction and deeper structural damage. This is essential knowledge for understanding and addressing any potential issues related to the patella.
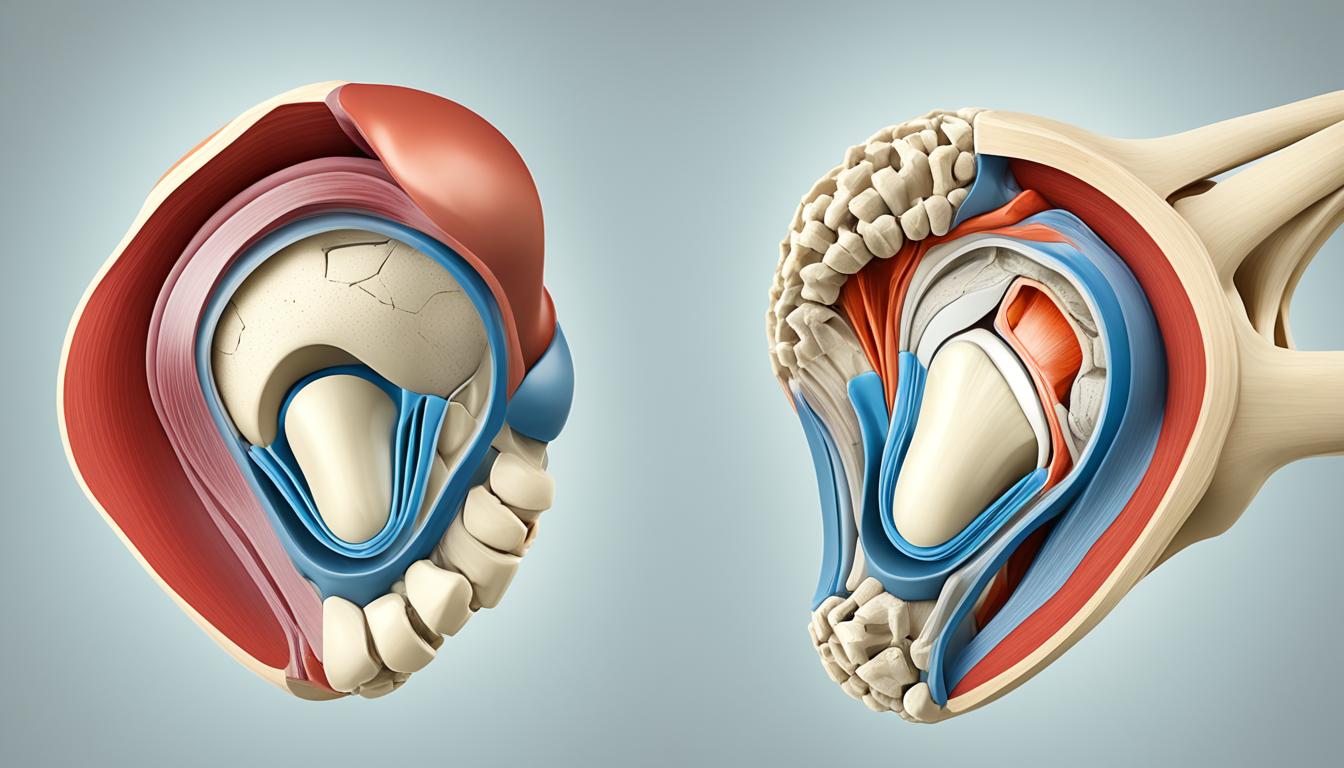
When it comes to the anatomy of the patella, this small yet significant bone is located deep to the fascia lata and the rectus femoris tendon, in the anterior region of the knee joint.
The patella, also known as the kneecap, has a triangular shape with a pointed apex that is attached to the patellar ligament. The upper third of the patella serves as the attachment point for the quadriceps tendon, while the vastus medialis and lateralis muscles insert on the medial and lateral borders, respectively.
The patella plays a crucial role in the function of the knee. One of its primary functions is to enhance the efficiency of the quadriceps muscle. The patella increases the moment arm, which allows for greater torque production during knee extension. This increased torque production leads to more efficient movement and improved force transmission.
In addition to enhancing muscle efficiency, the patella also helps in stabilizing the knee joint during physical activities such as walking, running, and jumping. It acts as a protective shield for the deeper structures in the knee joint, providing support and stability during various movements.
To help visualize the anatomy and function of the patella, refer to the table below:
| Anatomy of the Patella | Function of the Patella |
|---|---|
| – Located deep to the fascia lata and rectus femoris tendon – Triangular shape with a pointed apex – Attached to the patellar ligament – Quadriceps tendon attaches to the upper third | – Enhances efficiency of the quadriceps muscle – Increases the moment arm for greater torque production during knee extension – Stabilizes the knee joint during physical activities – Acts as a bony shield for deeper structures in the knee joint |
The development of the patella begins during childhood and continues into adulthood. It originates from a continuous band of fibrous connective tissue at the distal margin of the femur. Ossification, the process of bone formation, starts between the ages of 3 and 6 years and typically completes by adulthood.
Variations in the patella are not uncommon and can have an impact on its alignment and function. One such variation is a bipartite patella, where the patella is split into two parts due to the ossification of a second cartilaginous layer. Although bipartite patella is usually asymptomatic, it can sometimes cause pain or discomfort.
Another variation is patella alta, which refers to a high-riding patella. In this condition, the patella is positioned higher than normal within the quadriceps tendon. Patella baja, on the other hand, is characterized by a low-riding patella, where it sits lower than the usual position.
These variations in the patella’s structure can affect the alignment and function of the knee joint. It’s important to consider these variations when diagnosing and treating conditions related to the patella.
Did you know?
The term “patella” comes from the Latin word for “small pan” or “dish.” It was named after its round and flat shape, resembling a dish.
Several conditions and disorders can affect the patella, leading to knee pain and dysfunction. Patellar dislocation and patellar subluxation are common causes of knee pain, where the patella either fully dislocates or partially dislocates from its groove in the femur. When the patella dislocates, it moves out of its normal position, usually towards the outside of the knee. This can cause severe pain, swelling, and instability in the knee joint. Patellar subluxation, on the other hand, is a partial dislocation where the patella momentarily moves out of place but returns to its original position.
Osteoporosis, a condition characterized by decreased bone density and increased fracture risk, can also affect the patella. As the patella is a bone, it can be weakened by osteoporosis, making it more susceptible to fractures. Osteoporosis-related fractures in the patella can cause significant pain, swelling, and hinder normal knee function. It is important to note that osteoporosis is a systemic condition that affects multiple bones throughout the body, including the patella.
If you experience new symptoms in your knees, such as pain, swelling, grinding, or having trouble walking or moving, it is important to seek medical attention. A healthcare professional can properly diagnose and treat conditions affecting the patella, providing the necessary guidance and interventions for recovery and pain management.
| Condition | Symptoms | Treatment |
|---|---|---|
| Patellar Dislocation | Pain, swelling, instability in the knee | Immobilization, physical therapy, surgery in severe cases |
| Patellar Subluxation | Intermittent pain, feeling of patella shifting or slipping | Physical therapy, strengthening exercises, bracing |
| Osteoporosis-related Patella Fracture | Pain, swelling, limited mobility in the knee | Rest, immobilization, pain management, lifestyle modifications |
Please note that the above table provides a general overview and may not capture all possible conditions and treatments. A healthcare professional should be consulted for an accurate diagnosis and personalized treatment plan.
When it comes to assessing the function of the patella and diagnosing patellar conditions, healthcare providers rely on various tests and imaging techniques. These tests help in identifying the underlying cause of pain or dysfunction and guide appropriate treatment strategies.
The patella reflex test is a simple yet effective diagnostic tool used to evaluate the patellar reflex and the integrity of the nervous system. During the test, the healthcare provider taps the patellar tendon just below the patella, causing a reflexive contraction of the quadriceps muscle. Abnormal reflex responses can indicate nerve damage or other neurological issues.
In cases where a more detailed evaluation is required, imaging tests such as X-rays and magnetic resonance imaging (MRI) can provide valuable insights into the structure and condition of the patella. X-rays can help identify fractures, dislocations, or degenerative changes, while MRIs offer a more comprehensive view of soft tissue injuries, such as ligament tears or cartilage damage.
Treatment strategies for patellar conditions depend on the underlying cause and severity of the condition. Common treatment approaches include:
In more severe cases, such as patellar fractures, immobilization with a cast or brace may be necessary to facilitate proper healing. In some instances, surgical intervention might be required to realign the fractured bone segments or address other structural abnormalities.
Osteoporosis, a condition characterized by weakened bones, can increase the risk of fractures in the patella. Treatment for osteoporosis focuses on strengthening bones and reducing the risk of fractures. This may involve lifestyle modifications, such as regular weight-bearing exercises, adequate calcium and vitamin D intake, and lifestyle changes to reduce fall risks. In more severe cases, medications may be prescribed to optimize bone health and reduce the risk of fractures.
By implementing comprehensive treatment plans, healthcare providers aim to alleviate pain, improve function, and promote healing in individuals with patellar conditions. Regular monitoring, rehabilitation exercises, and patient education are essential components of successful treatment regimens.
The patella, located anterior to the knee joint in the human body, is a vital component for knee extension and stability. Its unique anatomical structure and function contribute to efficient movement and protection of the knee joint. Understanding the precise location and function of the patella is crucial for accurate diagnosis and effective treatment of conditions that affect it. Through proper medical evaluation and treatment, individuals experiencing patellar-related issues can find relief from pain and regain their mobility.
Whether it’s providing attachment points for tendons and ligaments, increasing the extension capacity of the quadriceps muscle, or acting as a bony shield for deeper knee joint structures, the patella plays a significant role. Its position in the body, anterior to the knee joint, facilitates optimal function and biomechanics during various activities.
By having a comprehensive understanding of the patella’s location and its contribution to knee function, healthcare providers can accurately diagnose and prescribe appropriate treatments for conditions such as patellar dislocation, subluxation, fractures, and complications related to osteoporosis. With timely and proper medical interventions, patients can experience significant improvements in their quality of life and regain their ability to engage in physical activities comfortably.
The patella, also known as the kneecap, is located in the anterior part of the knee joint, between the femur (thigh bone) and the tibia (shin bone).
The patella serves several important functions, including providing attachment points for the quadriceps tendon and the patellar ligament, increasing the extension capacity of the quadriceps muscle, protecting the quadriceps tendon from friction, and acting as a bony shield for deeper structures in the knee joint.
The patella develops from a continuous band of fibrous connective tissue at the distal margin of the femur. Ossification of the patella begins around the age of 3–6 years and typically completes by adulthood.
Common conditions that can affect the patella include patellar dislocation, patellar subluxation, and osteoporosis, which weakens the bones and increases the risk of fractures.
Patellar conditions can be diagnosed using imaging tests such as X-rays and MRIs. Treatments may include wearing braces or immobilizing devices, resting, physical therapy, and at-home treatments like icing and pain relievers. In cases of patellar fracture, immobilization and surgery may be required.
As a physical therapist with over 30 years of experience, I've helped countless patients identify…
Rheumatoid arthritis (RA) is a chronic autoimmune disease that follows a progressive course, typically worsening…
Discover how to alleviate Knee pain when vacuuming on carpet with our expert tips and…
Discover the best foam padding for carpet knee pain. We review top products to help…
We're analyzing Carpet vs. hard floor knee pressure to help you decide which flooring is…
Discover how Knee bursitis and carpet surfaces are connected in our Ultimate Guide. Learn the…