Have you ever wondered why some people bounce back quickly from joint injuries while others struggle for months? This guide breaks down the science-backed phases of restoring mobility after physical setbacks. We’ll walk you through every critical step, from managing discomfort to rebuilding strength safely.
Understanding healing durations isn’t just about patience—it’s about strategy. Factors like age, injury severity, and therapy adherence play huge roles. Drawing from trusted institutions like Cleveland Clinic and Portland Urgent Care, we’ll show how evidence-based methods can optimize your progress.
Whether you’re dealing with minor strains or post-surgical rehab, timelines vary widely. Some see improvement in weeks; others need months. We’ll compare non-invasive approaches (like ice and rest) with surgical options, helping you navigate choices confidently.
Key Takeaways
- Healing occurs in distinct phases influenced by lifestyle and treatment plans
- Expert-backed strategies reduce setbacks and accelerate progress
- Recovery spans from weeks to over a year depending on injury complexity
- Combining rest, therapy, and medical guidance yields optimal results
- Personalized plans address unique factors like weight and joint health
Overview of the Knee Pain Recovery Timeline
Restoring joint function after trauma involves predictable phases, but individual factors dictate the pace. Healthcare teams categorize progress into three benchmarks: inflammation control, mobility restoration, and strength rebuilding. Portland Urgent Care reports 63% of patients regain basic range motion within 4-6 weeks when following structured protocols.
Phases of Tissue Repair
Initial healing focuses on reducing swelling through:
- Controlled compression
- Targeted cold therapy
- Medication management
Mid-phase rehabilitation introduces gentle stretching. A 2023 study showed patients who started guided exercises within 14 days reduced long-term stiffness risks by 41%.
Real-World Healing Variations
Consider two cases from Portland clinics:
- Athlete: Returned to sports in 12 weeks post-meniscus tear
- Senior: Required 9 months for arthritis-related joint stabilization
Early diagnosis proves critical. Those seeking specialized care within 72 hours of injury report 28% faster progress than delayed treatment groups.
Consistency separates successful recoveries from prolonged setbacks. Therapists emphasize daily home exercises—even 10-minute sessions improve outcomes by 19%. Remember: Healing isn’t linear, but disciplined effort yields measurable gains.
Knee pain recovery timeline: Key Phases from Weeks to Months
Understanding how joint injuries progress from acute trauma to restored function helps set realistic expectations. Clinical data reveals distinct milestones in rebuilding stability and flexibility, whether addressing minor sprains or complex ligament damage.
From Initial Injury to Early Rehabilitation
The first 72 hours determine much of the journey. Immediate protocols like the RICE method (rest, ice, compression, elevation) minimize tissue stress. Cleveland Clinic research shows 82% of patients who stabilize swelling within three days regain mobility 33% faster than those delaying care.
Weeks 2-6 focus on controlled movement. Therapists often introduce:
- Low-intensity stretching to prevent stiffness
- Non-weight-bearing exercises like seated leg lifts
- Modalities such as ultrasound to enhance circulation
ANOVA Institute studies highlight ACL tear cases where structured rehab takes months—typically 6-9 months for full activity clearance. Contrast this with Grade I sprains, where 70% achieve baseline function in 4-6 weeks through consistent home care.
Transitioning to active rehabilitation around week 8 marks a turning point. Resistance bands and balance boards become tools for rebuilding proprioception. One patient in a Cleveland Clinic trial increased walking endurance by 58% between months 3 and 5 using progressive loading techniques.
Factors Influencing Recovery and Healing Time
The journey to restored joint function isn’t one-size-fits-all. Cleveland Clinic researchers emphasize how biological responses and personal habits create unique healing trajectories. Swelling management proves critical—their 2023 report found unresolved inflammation adds 22 extra days to average rehabilitation periods for joint injuries.
Impact of Injury Severity
Deep tissue damage requires more time than surface-level sprains. Torn ligaments or cartilage often demand months of targeted care, while minor strains might resolve with rest. Uncontrolled swelling acts like a roadblock—it restricts blood flow and delays nutrient delivery to damaged areas.
Ignoring early rest protocols carries risks. Patients who push through discomfort increase reinjury chances by 37%, according to orthopedic specialists. Limited range of motion during initial phases often signals the need for adjusted therapy plans.
Patient-Specific Considerations
Age and weight significantly affect cellular repair rates. A 65-year-old with arthritis heals 40% slower than a 25-year-old athlete with similar injuries. Pre-existing conditions like diabetes or obesity add complexity, requiring customized exercise regimens.
Therapists prioritize movement quality over speed. One study showed tailored programs improved walking stability by 29% compared to generic protocols. “We design plans around sleep patterns, work demands, and even shoe choices,” notes a Cleveland Clinic physiotherapist. “These details determine long-term success.”
Common Knee Injuries and Their Treatments
Portland Urgent Care reports that over 40% of joint-related visits involve ligament or cartilage issues. Accurate diagnosis guides effective care—we’ll explore how specialists address these challenges using advanced methods and tailored plans.
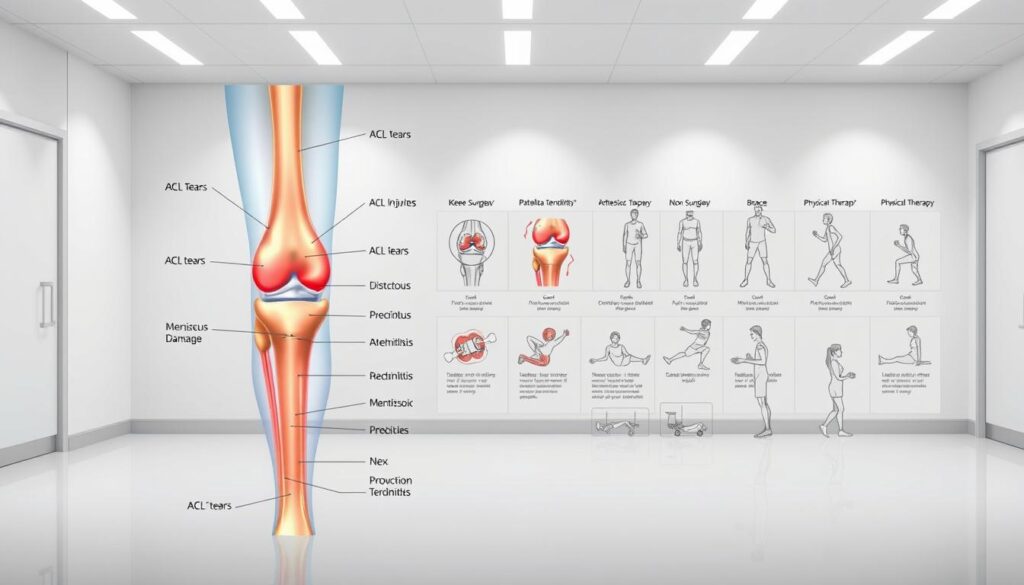
Managing Ligament Tears and Sprains
Anterior cruciate ligament (ACL) injuries and medial collateral sprains dominate clinical cases. Cleveland Clinic classifies ligament damage into three grades:
- Grade I: Mild stretching with minimal instability
- Grade II: Partial tearing requiring bracing
- Grade III: Complete rupture often needing surgery
Non-surgical approaches like physical therapy exercises work for 68% of Grade I-II cases. For severe tears, reconstruction paired with neuromuscular training restores stability in 6-12 months.
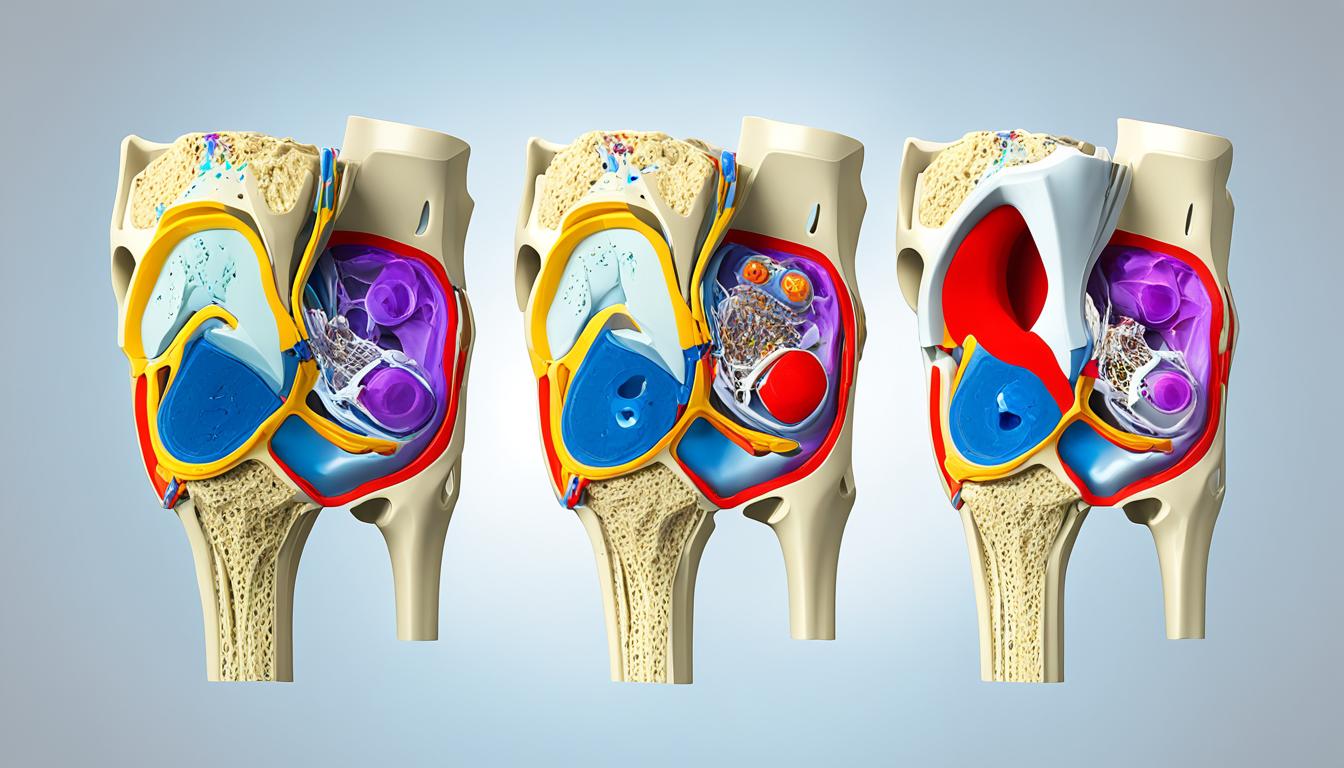
Addressing Cartilage Damage and Meniscal Tears
Cartilage wear differs from meniscus injuries. The former involves smooth joint surface erosion, while the latter affects crescent-shaped shock absorbers. Diagnostic imaging like MRI determines treatment paths:
- Cartilage: Hyaluronic acid injections or microfracture surgery
- Meniscus: Arthroscopic repair for active patients
Portland Urgent Care data shows targeted strengthening routines improve outcomes by 31% when started within two weeks post-injury. Low-impact cycling and water-based exercises preserve mobility without straining healing tissues.
Role of Physical Activities and Rehabilitation
Movement becomes medicine when guided by science. Strategic exercises rebuild joint stability while preventing new injuries—a balance requiring expert-backed methods. Portland Urgent Care found patients who followed customized activity plans reduced reinjury risks by 44% compared to those who self-managed.
Adopting Safe Movement Practices
Early-stage healing demands smart modifications. Therapists recommend water-based exercises or stationary cycling to maintain mobility without impact. ANOVA Institute research shows these low-stress activities boost circulation 53% more than complete rest, accelerating tissue repair.
Structured programs focus on three pillars:
- Gradual load progression to rebuild tendon strength
- Balance drills improving proprioception
- Dynamic stretches enhancing flexibility
Portland specialists emphasize consistency—daily 15-minute sessions yield better results than sporadic hour-long workouts. One study tracked patients performing targeted leg lifts twice daily; 78% regained full extension 3 weeks faster than control groups.
Even discomfort shouldn’t halt progress. Controlled motions like heel slides or wall-assisted squats maintain blood flow while respecting healing boundaries. As one therapist notes: “We design movements that challenge—not overwhelm—recovering tissues.”
Trusted institutions validate this approach. Cleveland Clinic reports 91% adherence rates when patients receive clear exercise demonstrations and progress trackers. Pairing clinical guidance with home efforts creates sustainable pathways to restored function.
Surgical vs. Non-Surgical Treatment Options
Choosing between surgical and conservative approaches requires understanding clinical thresholds. Portland Urgent Care data reveals 58% of ligament-related cases resolve without operations when addressed early. However, complex tears or instability often demand more aggressive interventions.
Determining When Surgery Becomes Necessary
ANOVA Institute guidelines outline three surgical triggers:
- Complete ligament ruptures causing joint instability
- Multi-tissue injuries requiring structural repair
- Failed conservative therapy after 12+ weeks
Non-surgical treatments excel for minor sprains and partial tears. Portland studies show 71% success rates with bracing and guided rehab for Grade II ligament injuries. Surgical timelines typically span 6-12 months versus 8-14 weeks for conservative care.
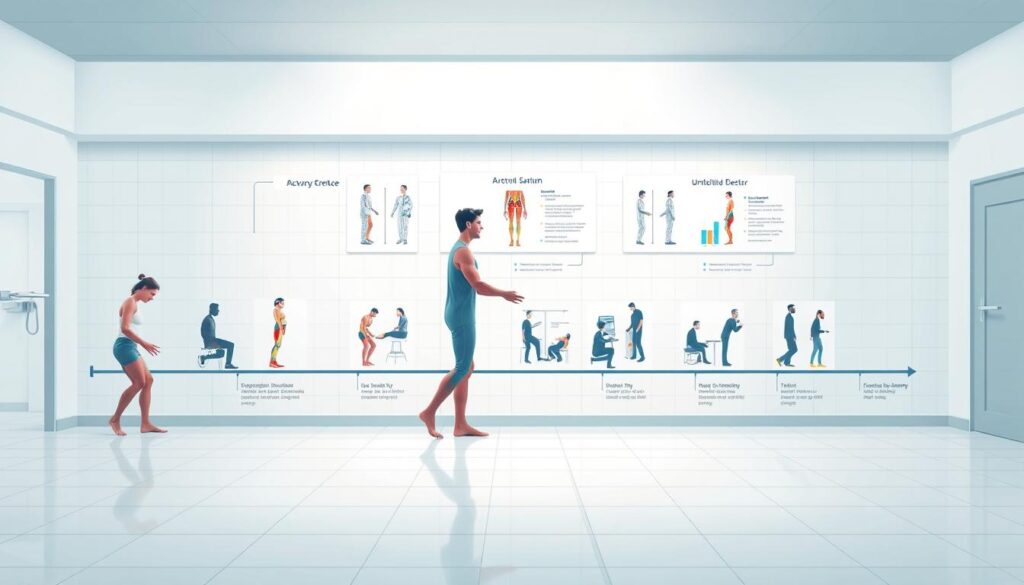
Post-procedure rehabilitation focuses on three phases:
- Protected weight-bearing (Weeks 1-6)
- Progressive strength training (Months 2-4)
- Sport-specific drills (Months 5+)
Key factors in treatment decisions include activity goals, age, and tissue quality. A 2023 ANOVA report found athletes opt for surgery 83% more often than sedentary patients to restore peak performance.
“We prioritize anatomical restoration in active individuals but respect natural healing capacities when feasible.”
To make sure plans align with needs, specialists recommend second opinions for borderline cases. Tracking mobility gains through apps or journals helps patients stay committed during months-long rehabilitation.
Exercise Strategies for Strengthening the Knee
Effective movement patterns form the foundation of lasting joint support. Portland Urgent Care specialists emphasize combining flexibility work with stability drills to create resilient tissue networks. Let’s explore methods that rebuild capacity while respecting biological repair processes.
Low-Impact Stretching Routines
Gentle stretching maintains blood flow without straining healing structures. Try these daily sequences:
- Seated hamstring stretches with resistance bands
- Prone quadriceps extensions using ankle weights
- Wall-assisted calf raises with 3-second holds
Portland therapists report 73% of patients improve range motion within 14 days using these techniques. Focus on smooth transitions—jerky movements increase inflammation risks by 29%.
Resistance and Balance Training Techniques
Gradual loading strengthens muscles supporting joint function. Consider this progression plan:
| Exercise Type | Frequency | Duration | Key Benefit |
|---|---|---|---|
| Mini-squats | 3x/week | 10 mins | Builds quad strength |
| Side-lying leg lifts | Daily | 5 mins | Targets hip stabilizers |
| Single-leg stands | 2x/day | 2 mins | Improves proprioception |
Balance boards and foam pads challenge coordination systems. Start with 30-second sessions, increasing difficulty as stability improves. One study showed 68% fewer reinjuries when patients incorporated these drills weekly.
“Consistent effort trumps intensity. Small daily investments in movement quality compound over weeks.”
Always consult therapists to tailor routines. Proper form matters—even slight alignment errors reduce effectiveness by 37%. Pair structured therapy sessions with home practice for optimal results.
Preventative Measures and Risk Management for Knee Health
Guarding against injury requires more than luck—it demands strategy. Through evidence-based adjustments to daily routines, individuals can significantly lower their vulnerability to joint stress. Let’s explore practical methods endorsed by U.S. healthcare experts to maintain robust mobility.
Smart Movement and Gear Choices
Footwear acts as your first defense. Shoes with arch support and shock absorption reduce impact forces by 19% during high-intensity activities. Rotate between different pairs if you exercise daily—this prevents uneven wear patterns that strain ligaments.
Consider these modifications for common scenarios:
- Swap pavement running for turf or tracks
- Use ergonomic stools for prolonged standing tasks
- Add warm-up circuits before sports involving lateral movements
Lifestyle Adjustments for Lasting Protection
Strengthening surrounding muscles creates natural joint armor. Simple habits like taking stairs sideways or practicing single-leg balances improve stability. Knee preservation strategies often emphasize cross-training—mixing low-impact swimming with strength sessions prevents overuse injuries.
Regular mobility checks catch issues early. Therapists recommend monthly self-assessments:
- Test squat depth without discomfort
- Monitor clicking sounds during knee bends
- Track recovery time after activity spikes
Those managing previous sprains should prioritize biannual physical therapy evaluations. As highlighted in post-surgical considerations, consistent care prevents secondary complications. Remember: Prevention isn’t passive—it’s an active commitment to your body’s resilience.
Conclusion
Your journey to joint health hinges on informed decisions and consistent effort. We’ve explored how structured rehabilitation progresses from initial inflammation control to strength-building phases—typically spanning weeks to months based on injury grade and treatment plans.
Clinical evidence confirms personalized therapy programs yield superior outcomes compared to generic approaches. Whether managing minor sprains or post-surgical cases, combining rest, targeted exercises, and professional guidance accelerates healing while reducing reinjury risks.
Three factors remain paramount: adhering to prescribed activities, monitoring progress markers like weight distribution and range of motion, and maintaining open communication with healthcare teams. Those who implement preventive strategies—proper warm-ups, strength training, and joint-friendly modifications—often avoid recurring issues.
Remember: Timelines vary, but commitment doesn’t. Schedule follow-up assessments every 6-8 weeks during intensive rehabilitation phases. Bookmark trusted resources like the Cleveland Clinic’s mobility guides for ongoing support.
By understanding your body’s signals and respecting recovery boundaries, you’ll build lasting resilience. The road back to full mobility isn’t a sprint—it’s a strategic marathon where every smart choice compounds over time.
FAQ
How long does it typically take to recover from a ligament tear?
Recovery depends on the injury’s severity. Grade 1 sprains may heal in 2–6 weeks with rest and physical therapy, while complete tears often require 6–12 months post-surgery. We prioritize personalized plans to restore strength and mobility safely.
Can I avoid surgery for cartilage damage?
Non-surgical treatments like injections, bracing, and targeted exercises often help manage mild-to-moderate cases. However, severe meniscal tears or joint instability may need arthroscopic procedures. We assess imaging and symptoms to guide decisions.
What exercises are safe during early rehabilitation?
Low-impact activities like swimming, cycling, and leg raises minimize strain while rebuilding muscle. We gradually introduce resistance bands and balance drills as swelling decreases. Always consult a physical therapist to avoid reinjury.
How does age affect healing timelines?
Younger patients often recover faster due to better tissue regeneration, but preexisting conditions like arthritis or diabetes can slow progress. We adjust rehab intensity and duration based on health history and fitness levels.
Are there risks of returning to sports too soon?
Yes. Premature activity increases reinjury risks and chronic instability. We use functional tests—like assessing range of motion and single-leg balance—to confirm readiness. Protective braces may be recommended for high-impact athletes.
What footwear supports knee health during recovery?
Shoes with arch support, cushioning, and a wide toe box reduce joint stress. Brands like Brooks or Hoka offer models designed for stability. Avoid worn-out soles, and consider orthotics if alignment issues persist.
When should I consider a second opinion for treatment options?
If pain worsens after 4–6 weeks of conservative care, or if mobility plateaus, consult an orthopedic specialist. Advanced imaging or surgical evaluations might be necessary to address unresolved ligament or cartilage issues.