Artificial knee replacement is a common surgical procedure that aims to alleviate pain and improve mobility in individuals with knee joint degeneration. This article provides an in-depth understanding of the anatomy of the knee joint, the causes of knee degeneration, indications for knee replacement surgery, and the types of knee replacement procedures.
Key Takeaways
- Artificial knee replacement is a viable option for individuals experiencing significant pain and disability due to knee degeneration.
- Non-surgical treatments may fail to provide adequate relief for knee degeneration, leading to the consideration of knee replacement surgery.
- Osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis are common causes of knee degeneration that may necessitate knee replacement surgery.
- Total knee replacement, partial knee replacement, and revision knee replacement are the main types of knee replacement procedures.
- Understanding the anatomy and function of the knee joint is crucial in determining the appropriate course of action for knee degeneration.
The Anatomy of the Knee Joint

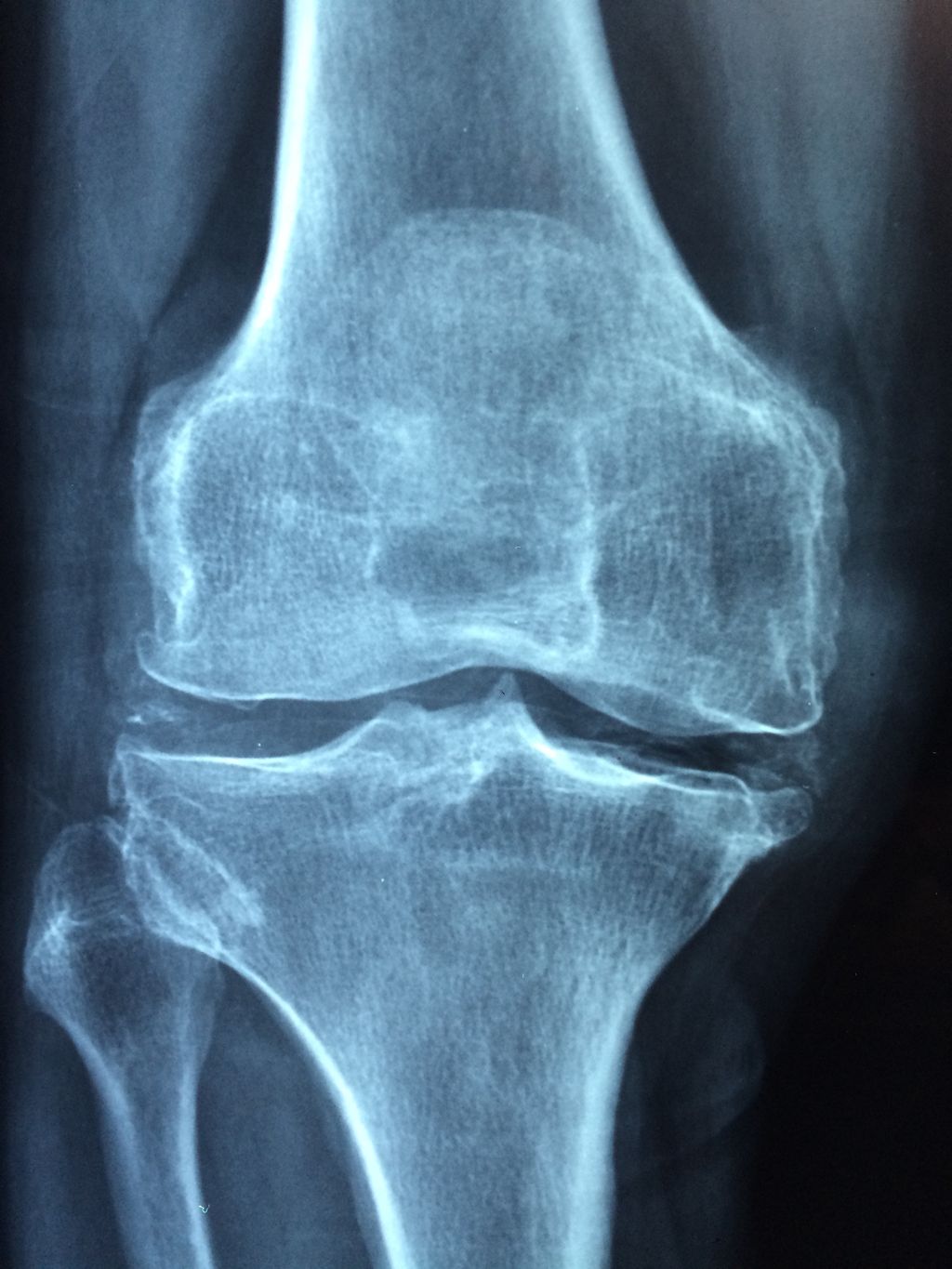
Structure of the Knee Joint
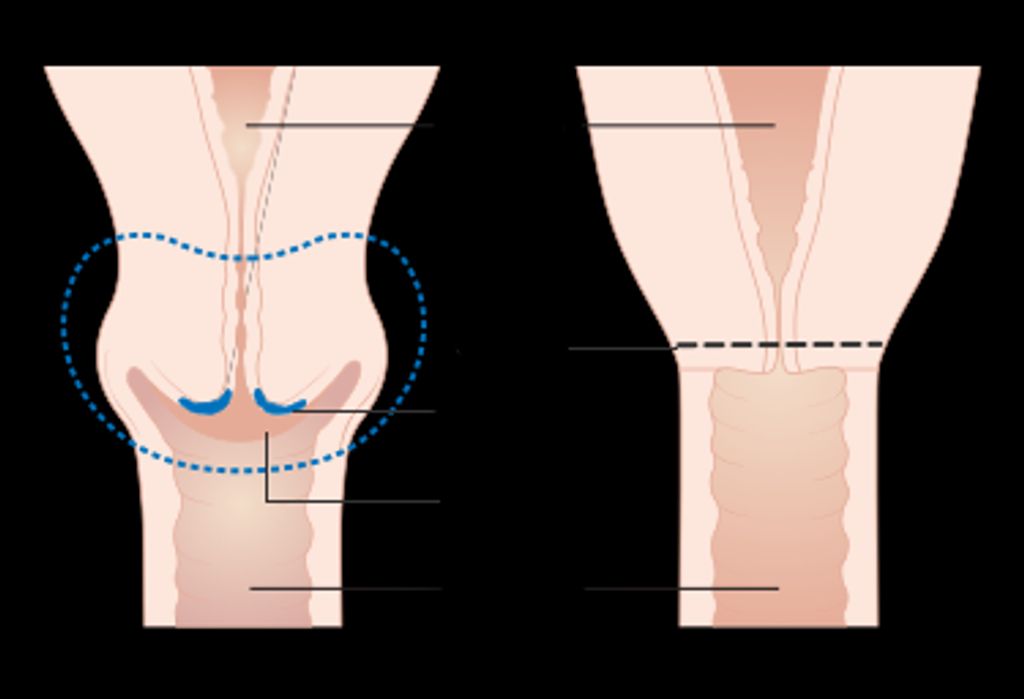
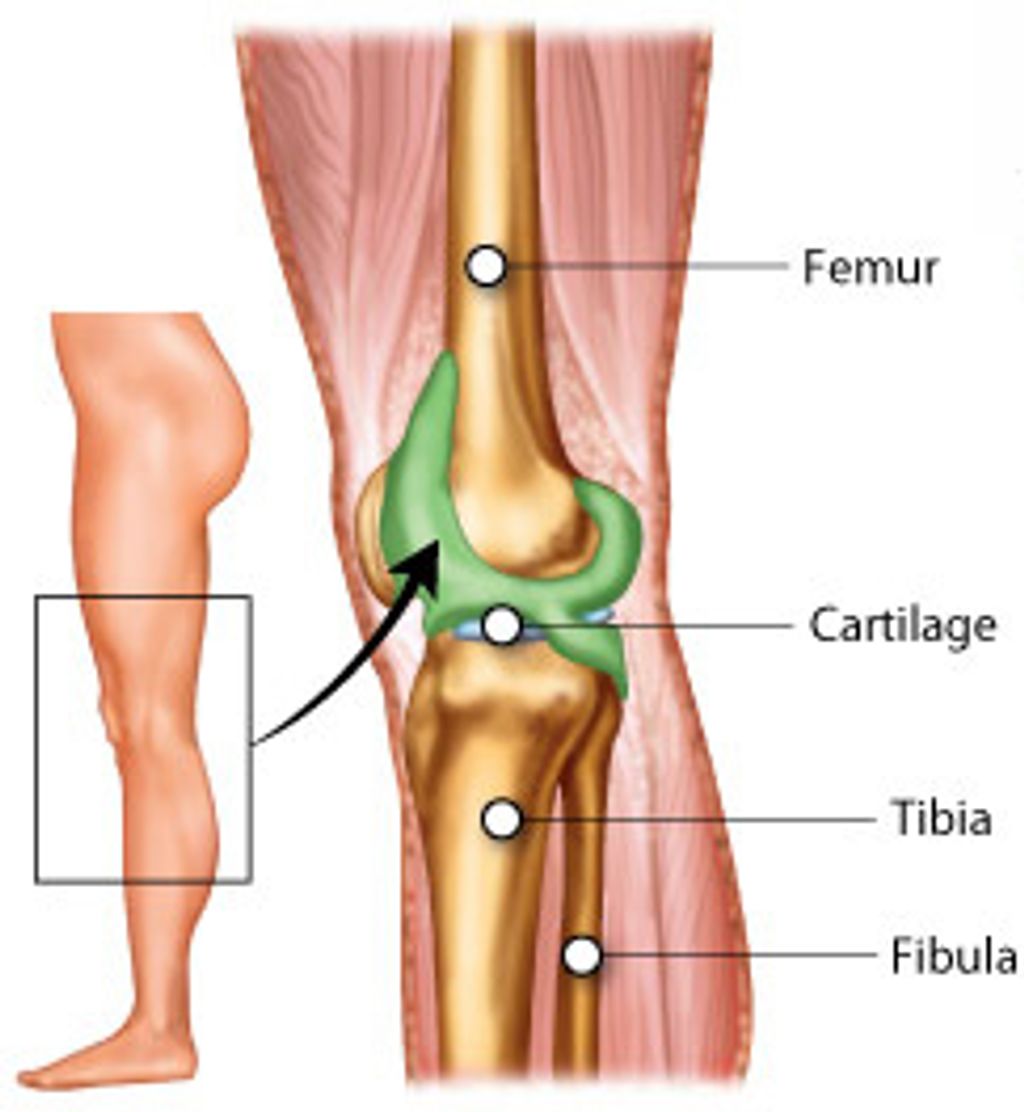
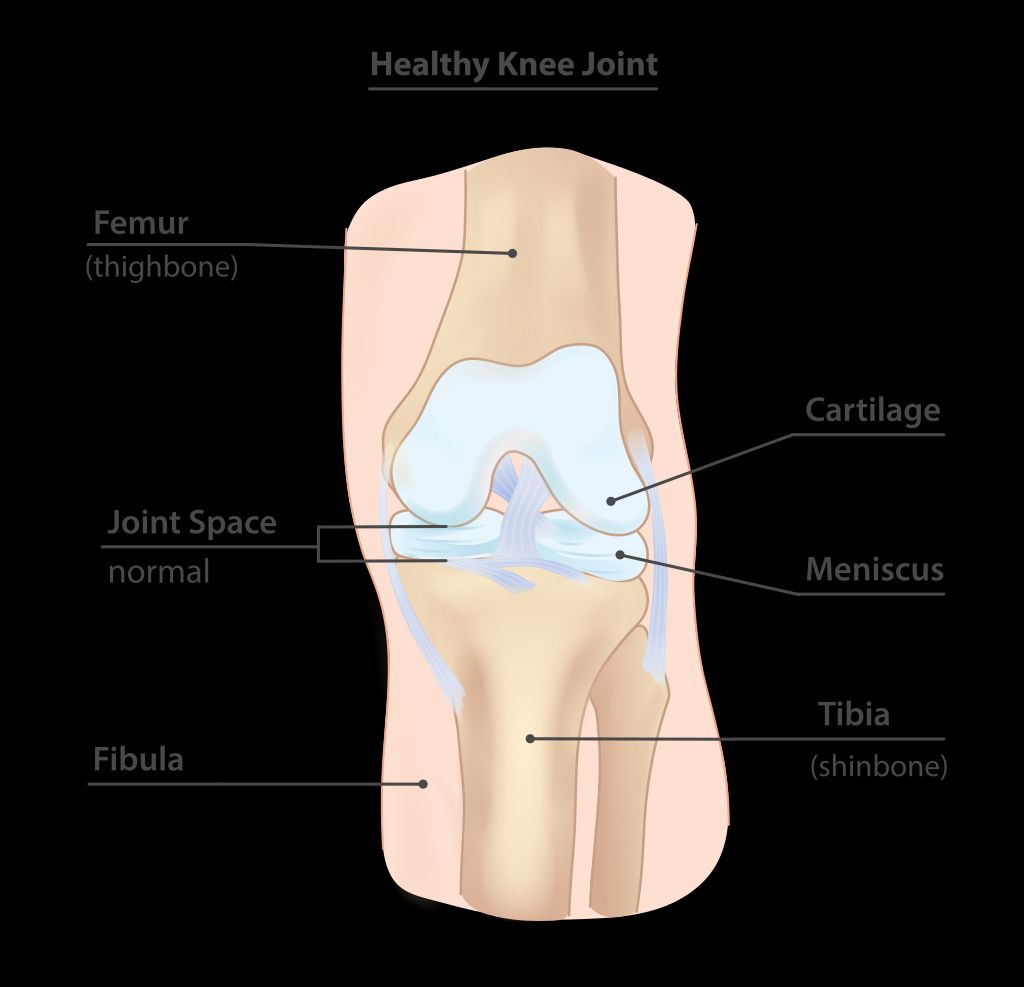
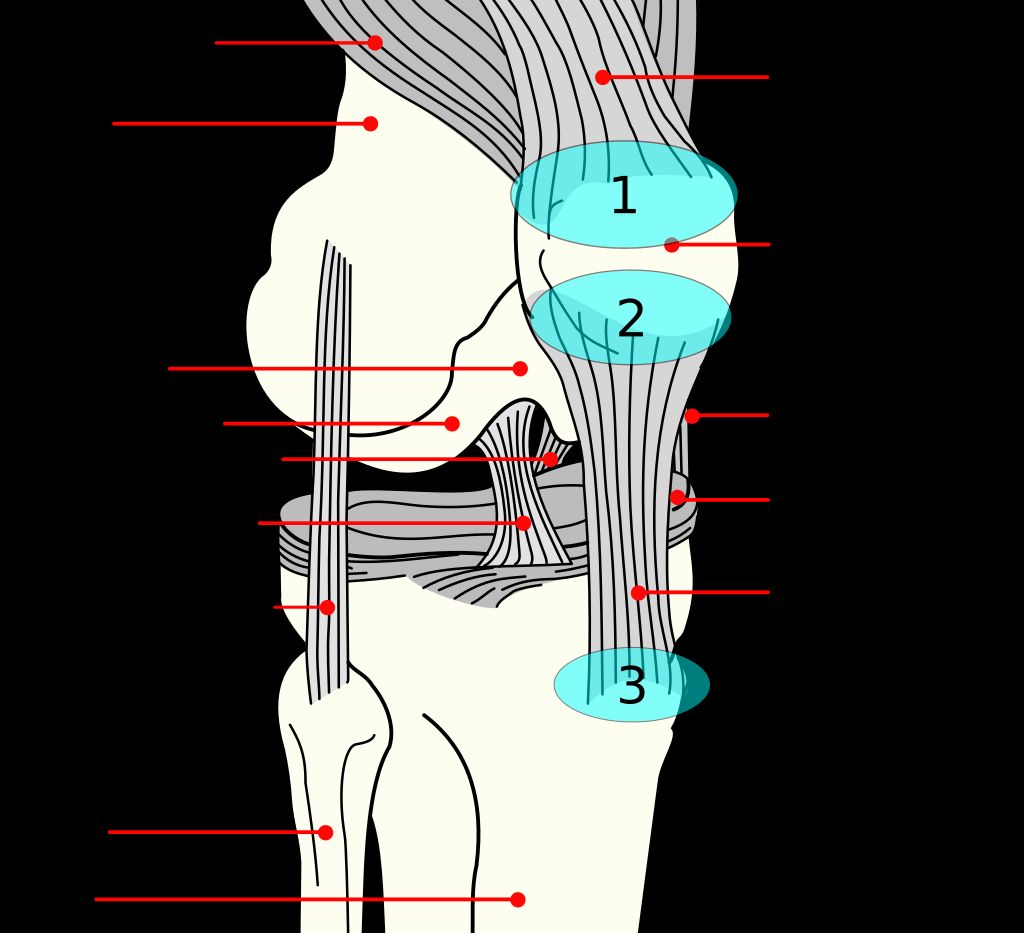
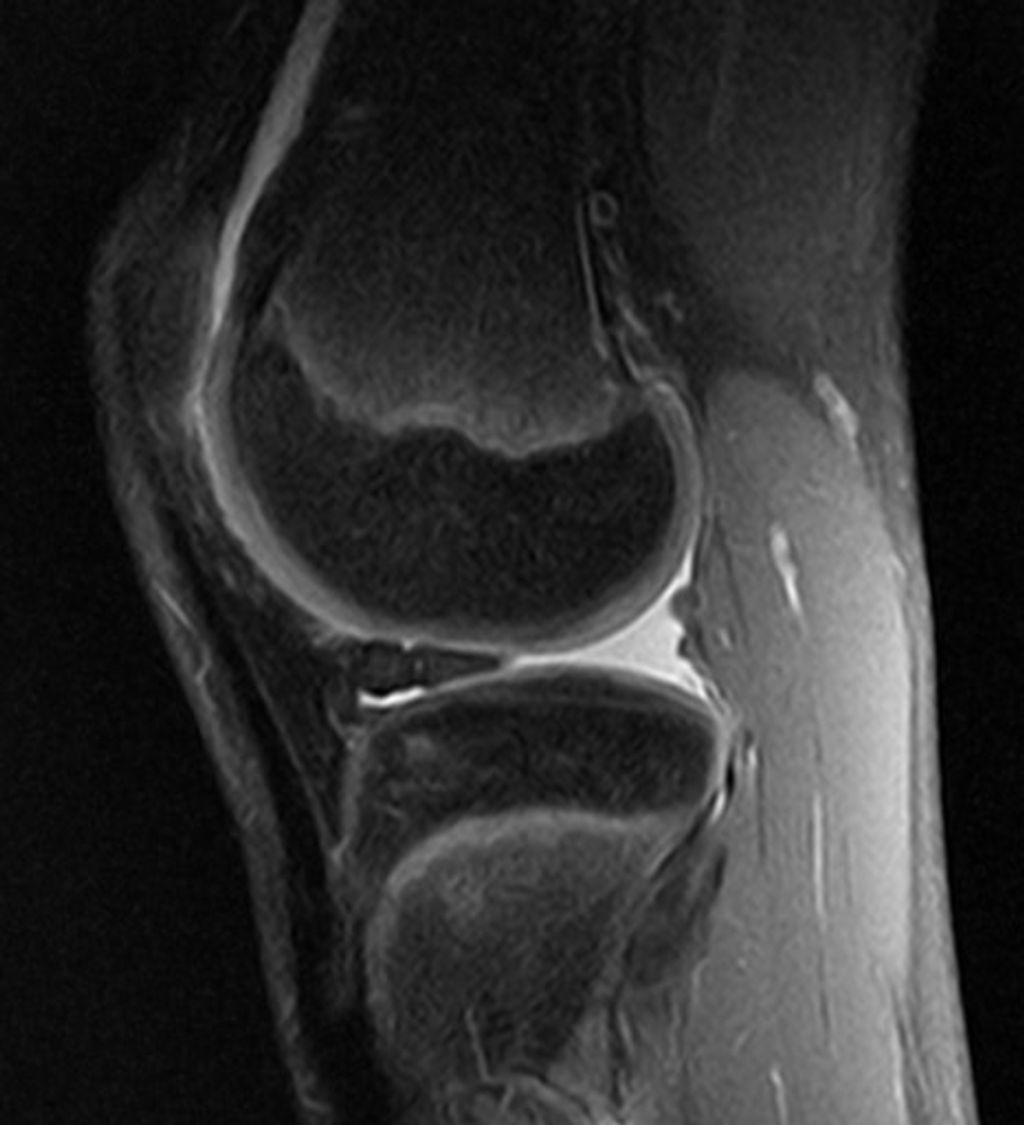
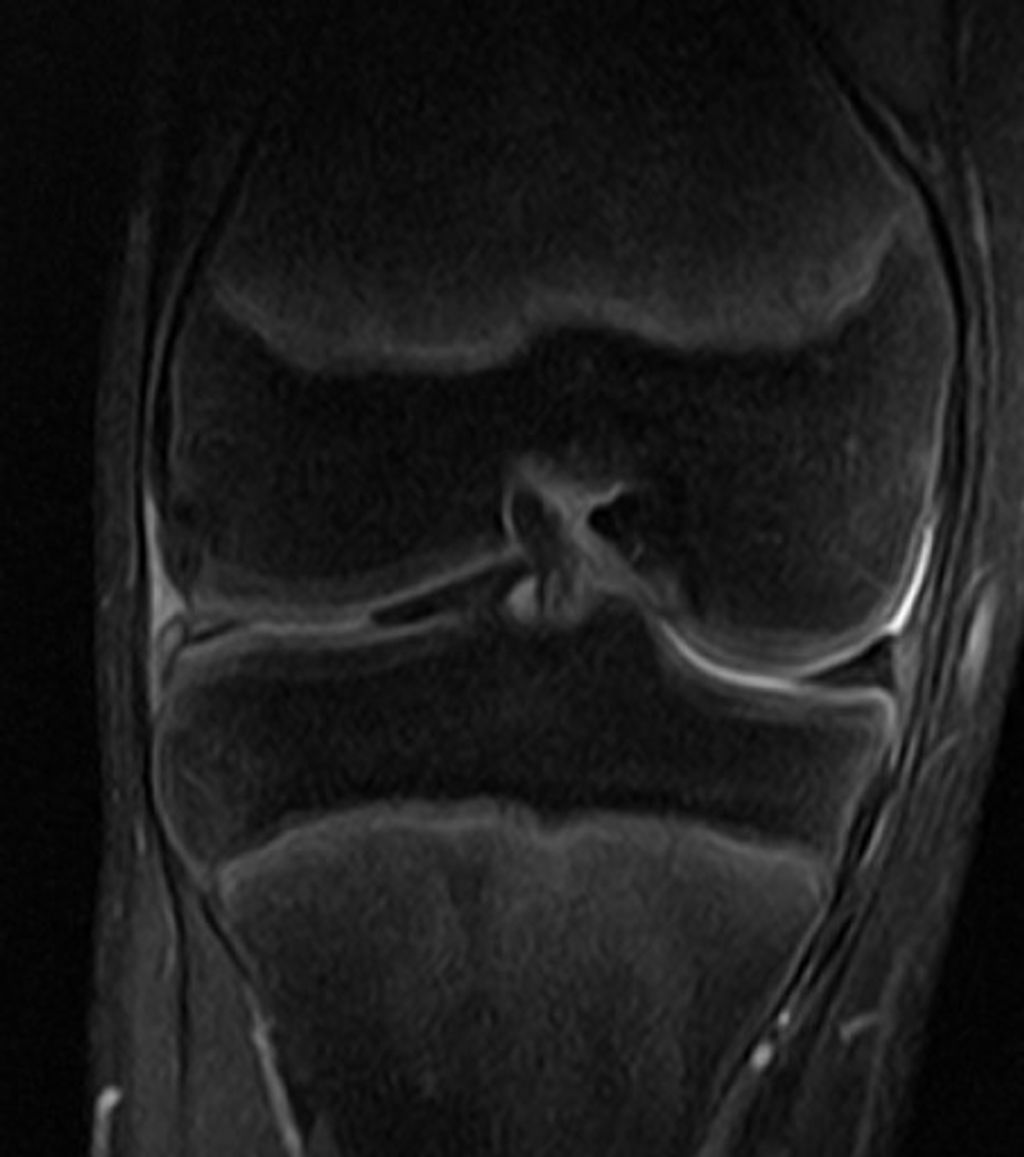
We must first understand the complex structure of the knee joint to appreciate the intricacies of an artificial knee replacement. The knee is a hinge joint, primarily involving two bones: the femur (thigh bone) and the tibia (shin bone). The patella (kneecap) also plays a crucial role, protecting the joint and facilitating movement.
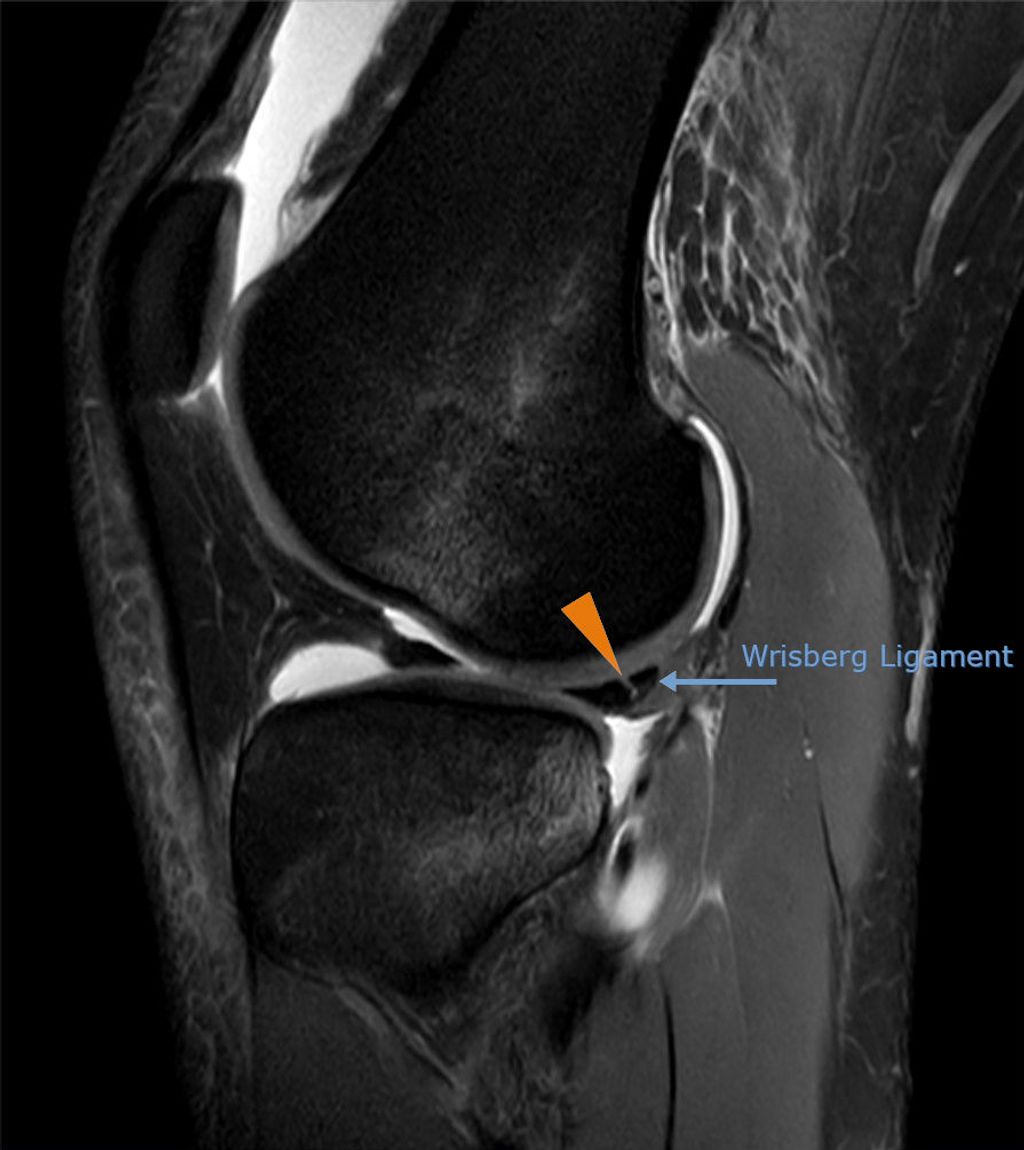
The knee joint is stabilized by a network of ligaments and tendons, with the meniscus acting as a cushion between the femur and tibia. This cartilaginous tissue is essential for absorbing shock and ensuring smooth movement. Surrounding the knee is the synovial membrane, which secretes fluid for lubrication.
Key Components of the Knee Joint:
- Femur (thigh bone)
- Tibia (shin bone)
- Patella (kneecap)
- Ligaments and tendons
- Meniscus
- Synovial membrane
Remember: Maintaining the health of each component is vital for knee joint function. Degeneration of any part can lead to pain and disability, potentially necessitating knee replacement surgery.
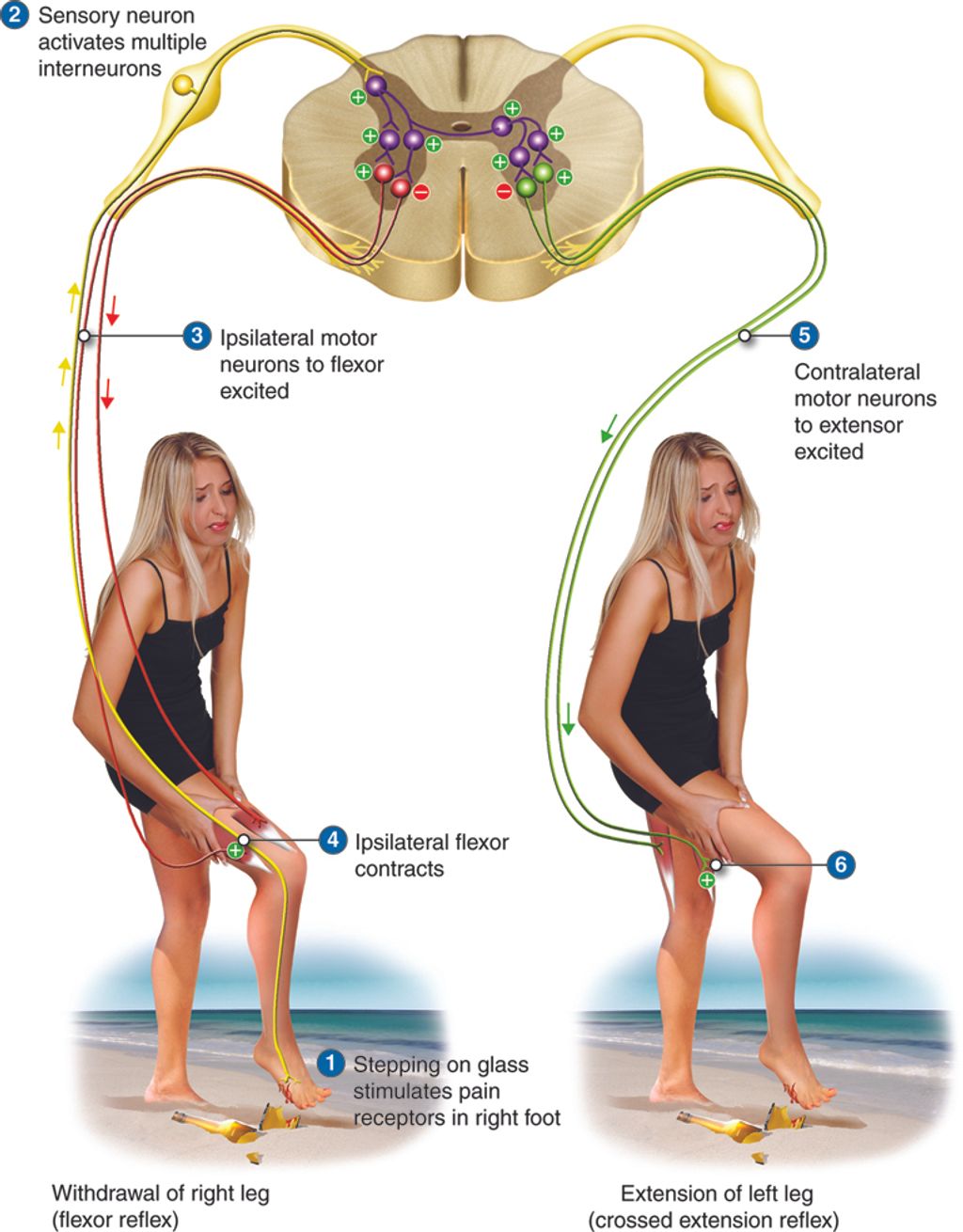
Function of the Knee Joint
The knee joint is a complex structure that allows flexion and extension of the lower leg. It also provides stability and support during weight-bearing activities. The joint is composed of three main components: the femur, the tibia, and the patella. These components work together to facilitate smooth movement and absorb shock. Additionally, the knee joint is surrounded by ligaments and tendons that provide further support and control movement. Understanding the function of the knee joint is crucial for comprehending the impact of degenerative conditions and the necessity for knee replacement surgery.
Causes of Knee Degeneration

Osteoarthritis
Osteoarthritis, a degenerative joint disease, is characterized by the breakdown of cartilage in the knee joint. It is the most common form of arthritis and often leads to pain, stiffness, and reduced mobility. In severe cases, osteoarthritis can significantly impact daily activities and quality of life.
- While the exact cause of osteoarthritis is not fully understood, it is believed to be influenced by a combination of genetic, metabolic, and mechanical factors.
- Risk factors for developing osteoarthritis include age, obesity, joint injuries, and repetitive stress on the knee joint.
It is important to maintain a healthy weight and engage in low-impact exercises to reduce the risk of osteoarthritis and alleviate its symptoms.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just the joints. It can damage a wide variety of body systems, including the skin, eyes, lungs, heart, and blood vessels. Early diagnosis and aggressive treatment are crucial to managing the symptoms and preventing joint damage. Regular monitoring and medication adjustments are often necessary to manage the condition effectively.
It is important to maintain a healthy lifestyle and follow the prescribed treatment plan to minimize the impact of rheumatoid arthritis on daily activities and overall well-being.
Post-Traumatic Arthritis
After discussing Post-Traumatic Arthritis, it is important to understand the impact of these degenerative conditions on the knee joint. One significant factor to consider is the progression of joint deterioration, which can lead to increased pain and reduced mobility. Additionally, the development of these conditions may necessitate surgical intervention, such as knee replacement procedures. It is crucial to recognize the implications of knee degeneration and the potential need for medical intervention.
Indications for Knee Replacement Surgery

Pain and Disability
After carefully evaluating the patient’s condition, it becomes evident that pain and disability are significantly impacting their quality of life. These symptoms persist despite the implementation of various non-surgical treatments. In such cases, the decision to proceed with knee replacement surgery becomes a viable option for improving the patient’s overall well-being. It is important to consider the patient’s individual circumstances and medical history when determining the most suitable course of action.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
Failure of Non-Surgical Treatments
After exhausting all non-surgical treatment options, surgical intervention becomes necessary for addressing the debilitating effects of knee degeneration. Our team carefully evaluates each patient’s unique condition to determine the most suitable course of action. In some cases, the decision to proceed with knee replacement surgery is based on the severity of pain and the extent of disability, which significantly impact the individual’s quality of life. Additionally, we consider the failure of non-surgical treatments as a crucial factor in recommending knee replacement surgery. It is important to note that this decision is made collaboratively with the patient, taking into account their specific needs and concerns.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
Types of Knee Replacement Procedures

Total Knee Replacement
After undergoing a Total Knee Replacement, we, as patients, must be aware of the potential risks and benefits associated with the procedure. It is crucial to follow the post-operative care instructions provided by the healthcare team to ensure proper healing and recovery.
Additionally, understanding the expected outcomes and rehabilitation process is essential. Here is a brief overview of the expected recovery timeline:
| Stage of Recovery | Duration |
|---|---|
| Immediate Post-Op | 1-2 days |
| Early Recovery | 2-6 weeks |
| Mid-Term Recovery | 6-12 weeks |
| Long-Term Recovery | 3-6 months |
It’s important to note that individual recovery may vary, and close communication with the healthcare team is vital for a successful recovery.
Lastly, it is advisable to avoid high-impact activities and to adhere to the prescribed physical therapy regimen to achieve optimal results.
Partial Knee Replacement
In our exploration of knee replacement procedures, we encounter the option of partial knee replacement. This approach is less invasive than total knee replacement and is suitable for patients whose damage is limited to a specific part of the knee. By targeting only the affected compartment, we preserve more of the knee’s natural structure and function.
The benefits of partial knee replacement include a shorter hospital stay, less blood loss, and often a quicker recovery time. However, it’s important to note that not all patients are candidates for this procedure. The decision is based on the location and extent of knee damage, as well as the patient’s overall health and activity level.
- When considering partial knee replacement, we must evaluate the following:
- The severity of knee arthritis
- The specific compartments affected
- The patient’s age and activity demands
- The alignment of the knee joint
Remember, the goal of any knee replacement is to alleviate pain and restore mobility. Partial knee replacement can be an excellent option for those who meet the criteria and wish to maintain as much of their natural knee function as possible.
Revision Knee Replacement
After undergoing a Revision Knee Replacement, our team focuses on providing comprehensive post-operative care to ensure optimal recovery. We monitor the patient’s progress closely and tailor rehabilitation programs to their specific needs. Additionally, we emphasize the importance of regular follow-up appointments to address any concerns and track long-term outcomes. Our approach is centered around promoting mobility, reducing discomfort, and enhancing overall quality of life for our patients.
Conclusion
In conclusion, the advancements in medical technology have revolutionized the field of orthopedics, particularly in the context of artificial knee replacement. The innovative techniques and materials used in modern knee replacement surgeries have significantly improved patient outcomes and quality of life. Continuous research and development in this area are essential to further enhance the effectiveness and longevity of artificial knee replacements, ensuring a better future for individuals suffering from knee-related conditions.
Frequently Asked Questions
What is the recovery time after knee replacement surgery?
The recovery time varies for each individual, but most people can expect to resume normal activities within 3 to 6 weeks after surgery.
What are the potential risks and complications of knee replacement surgery?
Potential risks and complications include infection, blood clots, implant loosening, and nerve or blood vessel damage. Your surgeon will discuss these in detail before the surgery.
Can I engage in sports or physical activities after knee replacement surgery?
Low-impact activities such as swimming, golf, and walking are generally recommended after knee replacement. High-impact activities like running and jumping should be avoided to protect the new knee joint.
How long do knee replacements typically last?
The lifespan of a knee replacement varies, but most implants last at least 15-20 years. Factors such as activity level, weight, and implant type can affect the longevity of the replacement.
What is the difference between total knee replacement and partial knee replacement?
Total knee replacement involves replacing the entire knee joint, while partial knee replacement replaces only the damaged part of the knee. Your surgeon will determine which procedure is suitable for you based on the extent of damage.
What can I do to prepare for knee replacement surgery?
Preparation may include physical therapy, strengthening exercises, and lifestyle adjustments. Your surgeon will provide specific instructions tailored to your individual needs.