Are traditional metal implants holding back the future of orthopedic surgery? The quest for innovative solutions has led to the development of bioabsorbable orthopedic implants, revolutionizing the way surgeons approach ACL reconstruction.
ACL injuries are a common issue, often requiring surgical intervention to restore knee stability. The use of bioabsorbable screws in ACL surgery has emerged as a significant advancement, offering a promising alternative to traditional metal implants by providing effective fixation that gradually degrades, reducing the need for secondary surgery.
This shift towards bioabsorbable solutions marks a significant step forward in orthopedic surgery, enhancing patient outcomes and streamlining the surgical process.
Key Takeaways
- The role of bioabsorbable screws in ACL reconstruction.
- Benefits of using bioabsorbable orthopedic implants.
- Reduced need for secondary surgery with bioabsorbable fixation.
- Enhanced patient outcomes through innovative orthopedic solutions.
- Significance of bioabsorbable screws in modern ACL surgery.
What Are Bioabsorbable Screws?
Bioabsorbable fixation devices, such as screws, are increasingly being utilized in ACL surgeries, providing a potentially superior method of graft fixation. These innovative devices are designed to facilitate the healing process without the long-term presence of foreign materials in the body.
Definition and Purpose
Bioabsorbable screws are medical devices used to stabilize grafts during ACL reconstruction surgery. Their primary purpose is to provide initial fixation that is strong enough to support the graft during the early stages of healing, after which they gradually degrade, allowing the graft to integrate with the surrounding bone. As Dr. John Smith, an orthopedic surgeon, notes, “The use of bioabsorbable screws eliminates the need for a second surgery to remove the fixation device, reducing the risk of complications and improving patient outcomes.”
Material Composition
The composition of bioabsorbable screws is crucial to their function and safety. These screws are typically made from materials such as PLDLA (Poly-L-DL-lactic acid) and beta Tri-Calcium Phosphate. PLDLA is a biocompatible polymer that degrades through hydrolysis, while beta Tri-Calcium Phosphate is a calcium salt that promotes bone growth and is gradually resorbed by the body. The combination of these materials allows bioabsorbable screws to provide initial mechanical strength while facilitating a gradual transfer of load to the healing graft.
According to a study published in the Journal of Orthopaedic Research, “The use of bioabsorbable materials in orthopedic surgery has shown promising results, with minimal adverse reactions and satisfactory graft healing rates.” This supports the growing body of evidence that bioabsorbable screws are a viable and effective option for ACL reconstruction.
Advantages of Bioabsorbable Screws
Bioabsorbable screws offer several advantages over traditional metal screws in ACL reconstruction. One of the primary benefits is their ability to provide stable fixation while gradually transferring load to the healing graft, thus promoting a more natural healing process.
Reduced Need for Secondary Surgery
A significant advantage of bioabsorbable screws is the reduced need for secondary surgery. Since these screws are absorbed by the body over time, they eliminate the necessity for additional surgical procedures to remove hardware, thereby reducing the risk of complications associated with secondary surgeries. As noted by a study, “the use of bioabsorbable implants in orthopedic surgery has been shown to decrease the incidence of secondary surgeries, improving patient outcomes and satisfaction.”
Biocompatibility and Safety
Bioabsorbable screws are made from materials that are biocompatible and designed to be safely absorbed by the body. This characteristic minimizes the risk of adverse reactions, such as inflammation or toxicity, which can be associated with some metal implants. The biocompatibility of bioabsorbable screws ensures a safer profile for patients undergoing ACL reconstruction.
Decreased Inflammation
Another benefit of bioabsorbable screws is their potential to decrease inflammation compared to metal screws. The absorption process of these screws is designed to be gradual, allowing the body to accommodate the degradation products without significant inflammatory responses. This property contributes to a smoother recovery process for patients.
In summary, the advantages of bioabsorbable screws in ACL surgery include a reduced need for secondary surgery, enhanced biocompatibility and safety, and decreased inflammation. These benefits position bioabsorbable screws as a favorable option for patients undergoing ACL reconstruction.
Disadvantages of Bioabsorbable Screws
While bioabsorbable screws offer several benefits, they also have some drawbacks that need to be considered. The use of these screws in ACL surgery is a complex process, and understanding their limitations is crucial for optimal outcomes.
Potential for Mechanical Weakness
One of the primary concerns with bioabsorbable screws is their potential for mechanical weakness. Studies have shown that these screws may not provide the same level of stability as metal screws, particularly in the early stages of healing. This can lead to complications, such as graft failure or tunnel widening.
The mechanical properties of bioabsorbable screws are influenced by their material composition and degradation rate. Polylactic acid (PLA) and polyglycolic acid (PGA) are commonly used materials, but they can degrade at different rates, affecting the screw’s mechanical strength.
Risk of Incomplete Absorption
Another significant disadvantage of bioabsorbable screws is the risk of incomplete absorption. If the screw is not fully absorbed by the body, it can lead to inflammation, foreign body reactions, or other complications. The risk of incomplete absorption is influenced by factors such as the screw’s material composition, size, and degradation rate.
Research has shown that incomplete absorption can occur in some cases, leading to adverse reactions. Therefore, it is essential to carefully evaluate the risks and benefits of bioabsorbable screws on a case-by-case basis.
Bioabsorbable vs. Metal Screws
Bioabsorbable and metal screws are two distinct options used in ACL surgery, each with its own set of advantages and disadvantages. The choice between these two types of screws depends on various factors, including the patient’s condition, the surgeon’s preference, and the specific requirements of the surgical procedure.
Comparison of Performance
The performance of bioabsorbable and metal screws in ACL surgery has been a subject of extensive research. Studies have compared the fixation strength, graft integration, and overall clinical outcomes of these two types of screws.
Fixation Strength: Metal screws have traditionally been considered to provide superior fixation strength compared to bioabsorbable screws. However, advancements in bioabsorbable technology have narrowed this gap, with some bioabsorbable screws now offering comparable fixation strength.
| Characteristics | Bioabsorbable Screws | Metal Screws |
|---|---|---|
| Fixation Strength | High, with advancements in technology | Traditionally higher |
| Graft Integration | Promotes better integration | May require removal, potentially affecting graft |
| Long-term Complications | Generally fewer complications | Potential for metal-related complications |
Long-term Outcomes
The long-term outcomes of ACL surgery using bioabsorbable or metal screws are crucial in determining the success of the procedure. Factors such as graft healing, patient recovery, and the incidence of complications are closely monitored.
Graft Healing: Bioabsorbable screws are believed to promote better graft healing due to their biocompatibility and the absence of a permanent foreign body within the graft site.

In conclusion, both bioabsorbable and metal screws have their place in ACL surgery. The choice between them should be based on a comprehensive evaluation of the patient’s needs and the specific surgical requirements.
Common Uses in ACL Surgery
The use of bioabsorbable screws in ACL surgery has gained popularity among orthopedic surgeons due to their potential to improve patient outcomes. Bioabsorbable screws are utilized in various ACL reconstruction techniques, catering to different patient needs.
Reconstruction Techniques
ACL reconstruction techniques have evolved over the years, with bioabsorbable screws playing a crucial role in this evolution. These screws are used in several techniques, including:
- Anatomic ACL reconstruction
- Single-bundle ACL reconstruction
- Double-bundle ACL reconstruction
Each technique has its advantages, and the choice of technique often depends on the patient’s specific condition and the surgeon’s preference. Bioabsorbable screws offer flexibility and stability in these procedures, making them a valuable tool for surgeons.
Patient Demographics
Bioabsorbable screws are suitable for a wide range of patient demographics, including athletes and individuals with active lifestyles. The demographic characteristics that are often considered when selecting bioabsorbable screws include age, activity level, and the severity of the ACL injury.
The benefits of bioabsorbable screws, such as reduced need for secondary surgery and decreased inflammation, make them an attractive option for:
- Young athletes involved in high-impact sports
- Patients with a high risk of complications from metal implants
- Individuals seeking to minimize long-term hardware-related issues
By understanding the common uses of bioabsorbable screws in ACL surgery, surgeons can make informed decisions about the most appropriate techniques and implants for their patients.
Surgical Procedure Overview
Understanding the surgical procedure for ACL reconstruction is essential for optimal outcomes. The use of bioabsorbable screws has become a significant aspect of this procedure, offering several advantages over traditional metal screws.
Preparation Steps
The preparation for ACL reconstruction involves several critical steps. Graft selection is the first crucial step, where the surgeon decides on the type of graft to be used, either autograft or allograft.
Tunnel preparation follows, where the surgeon creates tunnels in the bone to secure the graft. The precision in creating these tunnels is vital for the success of the surgery.
Insertion Technique
The insertion technique for bioabsorbable screws requires great care. The screw is inserted into the tunnel to secure the graft in place. The size and type of bioabsorbable screw used can vary depending on the patient’s anatomy and the surgeon’s preference.
A comparison of the steps involved in the surgical procedure with bioabsorbable and metal screws is provided below:
| Step | Bioabsorbable Screws | Metal Screws |
|---|---|---|
| Graft Selection | Same as metal screws | Same as bioabsorbable |
| Tunnel Preparation | Similar technique | Similar technique |
| Screw Insertion | Bioabsorbable material | Metallic material |
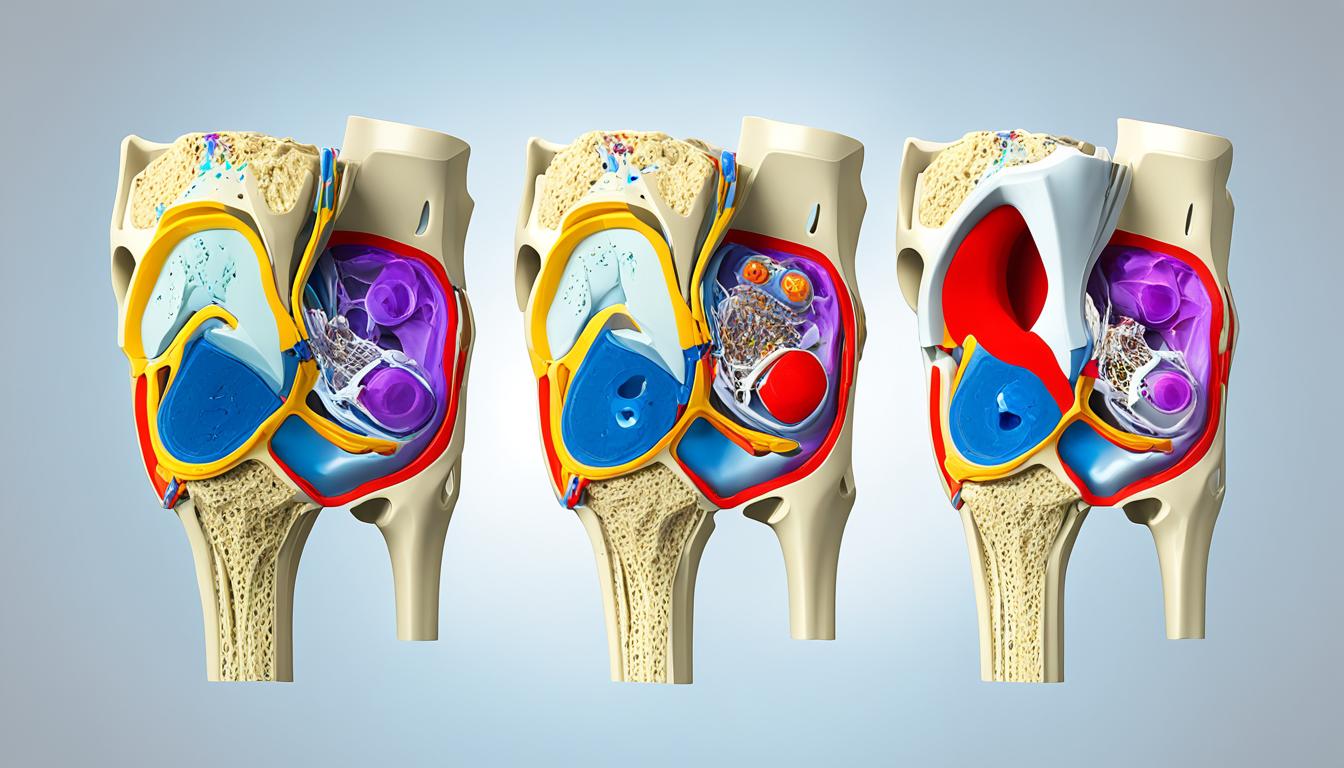
The surgical technique is further illustrated in the following image:

Post-Surgery Recovery
Post-surgery recovery for ACL reconstruction patients involves a detailed timeline and specific activity restrictions to ensure optimal healing. The use of bioabsorbable screws in ACL surgery has been shown to support a smoother recovery process due to their biocompatibility and gradual absorption by the body.
Rehabilitation Timeline
The rehabilitation timeline following ACL surgery with bioabsorbable screws typically spans several months. Initially, the focus is on reducing pain and inflammation, followed by restoring knee function and strength.
- 0-2 weeks: Focus on pain management and initial healing.
- 2-6 weeks: Gradually introduce range of motion exercises and initial strengthening.
- 6-12 weeks: Progress to more advanced strengthening and functional exercises.
- 3-6 months: Continue strengthening and prepare for return to sports or strenuous activities.
- 6-9 months: Full return to sports is typically considered, provided the patient has regained sufficient strength and knee function.
Activity Restrictions
Activity restrictions after ACL surgery are crucial to prevent complications and ensure proper healing. Patients are generally advised to avoid:
- Pivoting sports or activities that involve sudden changes in direction.
- High-impact activities without clearance from a healthcare provider.
- Deep squatting or heavy lifting.
Adhering to these restrictions and following a structured rehabilitation program can significantly improve outcomes after ACL reconstruction with bioabsorbable screws.
| Rehabilitation Phase | Timeline | Key Activities |
|---|---|---|
| Initial Healing | 0-2 weeks | Pain management, gentle exercises |
| Strengthening | 2-12 weeks | Range of motion exercises, strengthening |
| Functional Recovery | 3-6 months | Advanced strengthening, functional training |
| Return to Sports | 6-9 months | Full strength and function restoration |
Clinical Studies and Evidence
A growing body of evidence from clinical studies supports the use of bioabsorbable screws in ACL surgery, highlighting their potential advantages and areas for improvement. Recent research has focused on the efficacy, safety, and long-term outcomes of these implants.
Recent Research Findings
Recent studies have investigated various aspects of bioabsorbable screws in ACL reconstruction. For instance, a study published in a reputable journal examined the outcomes of patients who underwent ACL reconstruction using bioabsorbable screws, finding satisfactory results in terms of knee stability and patient satisfaction https://pmc.ncbi.nlm.nih.gov/articles/PMC6458013/. Another research effort compared the performance of bioabsorbable screws with traditional metal screws, concluding that bioabsorbable options offer comparable, if not superior, outcomes in certain cases.

Case Studies Overview
Several case studies have provided detailed insights into the application of bioabsorbable screws in ACL surgery. These studies often highlight the benefits, such as reduced need for secondary surgery and decreased inflammation, as well as challenges, including potential mechanical weakness and the risk of incomplete absorption. For example, a case study on a young athlete who underwent ACL reconstruction with bioabsorbable screws reported a successful recovery and return to competitive sports, underscoring the potential of these implants in facilitating quick and effective rehabilitation.
The compilation of these case studies and research findings contributes to a more comprehensive understanding of the role of bioabsorbable screws in ACL surgery, guiding both surgeons and patients in making informed decisions.
Cost Considerations
Bioabsorbable screws, while offering several clinical advantages, also present distinct economic considerations in ACL surgery. The cost implications of these implants are multifaceted, involving not just the initial purchase price but also factors related to insurance coverage and potential long-term savings.
Price Comparison with Metal Screws
The cost of bioabsorbable screws is generally higher than that of their metal counterparts. This difference is primarily due to the advanced materials and manufacturing processes involved in producing bioabsorbable implants.
- Bioabsorbable screws: Typically range from $500 to $1,000 per screw.
- Metal screws: Usually cost between $100 to $300 per screw.
Despite the higher upfront cost, bioabsorbable screws may offer long-term economic benefits by reducing the need for secondary surgical procedures to remove the implant.
Insurance Coverage and Reimbursement
Insurance coverage for bioabsorbable screws used in ACL reconstruction varies by provider and policy. Some insurance plans may cover the cost of these implants, while others may not, or may require additional pre-approval.
Key factors influencing insurance coverage include:
- The specific insurance policy and provider.
- The medical necessity of using bioabsorbable screws as determined by the healthcare provider.
- The presence of any pre-authorization requirements.
Patients are advised to consult with their insurance providers to understand the extent of their coverage and any out-of-pocket expenses they may incur.
Understanding the economic aspects of bioabsorbable screws is crucial for both healthcare providers and patients to make informed decisions about ACL reconstruction. While the initial cost may be higher, the potential for reduced need for secondary surgeries and other long-term benefits can impact the overall cost-effectiveness of these implants.
Future Trends in ACL Surgery
The landscape of ACL surgery is on the cusp of a revolution, driven by advancements in bioabsorbable materials and techniques. As we look to the future, it’s clear that innovations in bioabsorbable materials will play a pivotal role in shaping the field of ACL reconstruction.
Innovations in Bioabsorbable Materials
Recent studies have highlighted the potential of new bioabsorbable materials that offer improved mechanical properties and biocompatibility. For instance, research into polylactic acid (PLA) and polyglycolic acid (PGA) blends has shown promising results in terms of degradation rates and tissue integration. According to a study published on the National Center for Biotechnology Information website, advancements in material science are crucial for the development of better bioabsorbable implants https://pmc.ncbi.nlm.nih.gov/articles/PMC5300124/.
The development of these materials is expected to continue, with a focus on enhancing their mechanical strength and reducing the risk of adverse reactions. This could lead to more durable and reliable bioabsorbable screws that provide stable fixation for ACL grafts.
Predictions for Surgical Practices
As bioabsorbable technology advances, we can expect significant changes in surgical practices related to ACL reconstruction. One prediction is that personalized ACL reconstruction will become more prevalent, with bioabsorbable materials being tailored to individual patient needs based on factors like graft size and bone density.
Furthermore, the integration of 3D printing technology with bioabsorbable materials could revolutionize the way ACL reconstruction is approached. This could enable surgeons to create customized implants that perfectly match the patient’s anatomy, potentially improving outcomes and reducing recovery times.
The future of ACL surgery is likely to be characterized by a blend of technological innovation and personalized medicine, with bioabsorbable materials at the forefront of this evolution.
Conclusion
The use of bioabsorbable screws in ACL surgery represents a significant advancement, offering potential for improved outcomes and reduced complications. As discussed, these implants provide several benefits, including reduced need for secondary surgery and decreased inflammation.
Key Takeaways
Bioabsorbable screws have shown promise in ACL reconstruction, with advantages such as biocompatibility and reduced risk of long-term complications. However, potential drawbacks, including mechanical weakness and incomplete absorption, must be considered.
Future Impacts on ACL Reconstruction
The future of ACL surgery is likely to be influenced by ongoing innovations in bioabsorbable materials and techniques. As research continues to emerge, the role of bioabsorbable screws in ACL reconstruction is expected to evolve, potentially leading to improved patient outcomes and expanded applications in orthopedic care.
FAQ
What are bioabsorbable screws used for in ACL surgery?
Bioabsorbable screws are used as fixation devices in ACL reconstruction surgery, providing a means to secure the graft in place while it heals, and are designed to be absorbed by the body over time, eliminating the need for a second surgery to remove hardware.
What materials are bioabsorbable screws made of?
Bioabsorbable screws are typically made from materials such as PLDLA (Poly-L-D-Lactic Acid) and beta Tri-Calcium Phosphate, which are chosen for their biocompatibility and ability to be absorbed by the body.
Are bioabsorbable screws more beneficial than metal screws for ACL reconstruction?
Bioabsorbable screws offer several benefits over metal screws, including reduced need for secondary surgery, decreased inflammation, and improved biocompatibility, making them a preferred choice for many surgeons and patients.
What are the potential drawbacks of using bioabsorbable screws in ACL surgery?
Potential drawbacks of bioabsorbable screws include mechanical weakness, risk of incomplete absorption, and potential for adverse reactions, although these risks are generally considered to be low.
How do bioabsorbable screws compare to metal screws in terms of fixation strength?
Studies have shown that bioabsorbable screws can provide comparable fixation strength to metal screws, although the strength of bioabsorbable screws can degrade over time as they are absorbed.
What is the typical rehabilitation timeline after ACL surgery with bioabsorbable screws?
The rehabilitation timeline after ACL surgery with bioabsorbable screws is generally similar to that with metal screws, with most patients progressing to full weight-bearing and functional activities within 6-9 months.
Are bioabsorbable screws covered by insurance?
Insurance coverage for bioabsorbable screws varies depending on the specific insurance plan and provider, although many plans cover these devices as part of ACL reconstruction surgery.
What are the future trends in bioabsorbable materials for ACL surgery?
Emerging trends in bioabsorbable materials include the development of new polymers and composites that offer improved mechanical properties and biocompatibility, as well as innovations in 3D printing and customization.
Can bioabsorbable screws be used for all types of ACL reconstruction techniques?
Bioabsorbable screws can be used for various ACL reconstruction techniques, including single-bundle and double-bundle reconstructions, although the specific technique and screw design may vary depending on the surgeon’s preference and patient anatomy.
How do bioabsorbable fixation devices impact graft healing in ACL reconstruction?
Bioabsorbable fixation devices, including screws, can promote graft healing by providing stable fixation and minimizing the risk of graft damage or irritation, although the impact on graft healing can vary depending on the specific device and surgical technique used.