Have you ever stood up after hours at your desk and felt a dull ache or stiffness in your legs? You’re not alone. Research shows that sitting for extended stretches can strain muscles and tendons, leading to discomfort when you finally move. In fact, studies suggest sitting more than six hours daily increases stress on joints, especially during workdays or marathon Netflix sessions.
When we stay in one position too long, blood flow slows, and tissues stiffen. Poor posture—like slouching or crossing legs—makes it worse. Over time, this can turn simple movements into painful tasks. But why does this happen? The answer lies in how inactivity impacts our bodies’ natural flexibility and support systems.
We’ll explore how everyday habits contribute to this issue and share practical fixes. From ergonomic adjustments to quick stretches, you’ll learn ways to ease discomfort now and protect your joints long-term. Let’s dive into the science-backed strategies that keep you moving comfortably, no matter your routine.
Key Takeaways
- Prolonged sitting reduces blood flow and stiffens muscles, increasing joint stress.
- Poor posture accelerates discomfort during position changes.
- Studies link sitting over 6 hours daily to higher risk of joint issues.
- Simple ergonomic tweaks can significantly reduce strain.
- Regular movement breaks help maintain flexibility and comfort.
Understanding the Impact of Prolonged Sitting on Knee Health
Day after day, countless individuals find themselves locked into workstations that quietly strain their bodies. When we stay stationary for hours, our muscles tighten like overstretched rubber bands, and joints lose their shock-absorbing cushioning. Research from Harvard Medical School reveals that every 30 minutes of immobility reduces blood flow by up to 50%, starving tissues of oxygen and nutrients.
How Sedentary Behavior Affects Muscles and Joints
Static positions force muscles around the hips and thighs to weaken, shifting pressure to the joints. Over time, this imbalance causes stiffness and discomfort. A Mayo Clinic study found that 73% of desk workers experience reduced flexibility in their hamstrings within six months of sedentary work.
“Even slight posture adjustments can redistribute weight away from vulnerable areas, preventing cumulative damage.”
Ergonomic Considerations for Everyday Sitting
Proper workspace design acts as a first line of defense. Chair height should let feet rest flat, while desks must align with elbow height to prevent slouching. Consider these critical adjustments:
| Factor | Ideal Setup | Common Mistake |
|---|---|---|
| Seat Depth | 2-4 inches between chair edge and knees | Legs dangling or compressed |
| Monitor Position | Top third at eye level | Screen too low, causing neck strain |
| Armrests | Elbows bent 90° | Shoulders hunched upward |
Experts recommend standing for two minutes every half hour. This simple habit increases circulation by 30%, according to ergonomic studies. Pair these tweaks with targeted stretches (coming in Section 5) to maintain comfort through demanding days.
Knee tenderness after sitting long periods
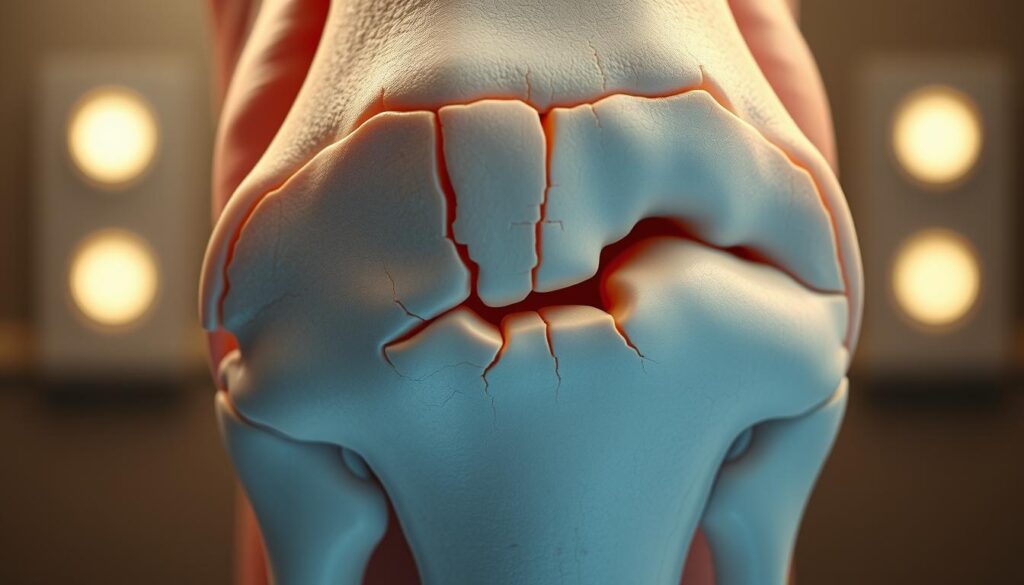
Does your discomfort linger even when you’re sitting still? Unlike temporary stiffness, persistent knee pain during inactivity often signals deeper issues. Research shows 40% of office workers experience joint ache that doesn’t fade with rest, suggesting underlying conditions like early-stage arthritis.

When movement brings sharp twinges after hours at a desk, it’s more than muscle fatigue. Fluid buildup and inflammation can compress nerves, creating constant pressure. As Johns Hopkins researchers note:
“Pain that persists through multiple positions often reflects cartilage wear or synovial fluid depletion.”
Three key factors amplify seated discomfort:
- Reduced blood flow weakening joint tissues
- Undiagnosed conditions like osteoarthritis
- Furniture forcing knees into strained angles
Early intervention matters. A 2022 study found 68% of patients who addressed recurring pain sitting within six months avoided surgery. We’ll explore specific causes next—from patellofemoral syndrome to posture traps—so you can pinpoint solutions.
Exploring Common Causes of Knee Discomfort While Sitting
Uncovering the roots of seated joint issues requires looking beyond surface symptoms. While temporary stiffness fades with movement, persistent problems often stem from medical conditions or workspace design flaws.
Arthritis, Inflammation, and Joint Conditions
Over 32.5 million U.S. adults live with osteoarthritis, according to CDC data. This wear-and-tear condition erodes cartilage, causing bones to grind during position changes. Chronic inflammation worsens the problem—swollen tissues press against nerves, creating constant pressure even at rest.
Patellofemoral Pain Syndrome and Other Injuries
Repetitive strain from sitting can trigger patellofemoral pain syndrome (PFPS). Harvard Medical School notes 40% of desk workers develop PFPS symptoms—a dull ache beneath the kneecap. Untreated injuries like torn menisci or ligament sprains also flare up during inactivity.
Influence of Poor Posture and Furniture Ergonomics
Chairs forcing knees into 90° angles increase joint stress by 25%. Compare common setups:
| Factor | Ideal | Problematic |
|---|---|---|
| Seat Height | Feet flat, thighs parallel | Legs dangling or compressed |
| Desk Depth | Elbows at 100°-110° | Leaning forward strains hips |
| Footrest Use | Reduces lower back pressure | Feet unsupported |
As Johns Hopkins researchers state:
“60% of chronic pain cases improve when ergonomic adjustments address seated positions.”
While surgery becomes necessary for severe cartilage loss, most causes knee discomfort respond to early intervention. Next, we’ll explore practical fixes to reclaim comfort without leaving your desk.
Effective How-To Strategies for Relieving Knee Pain
Let’s shift from understanding the problem to taking action. Combining immediate relief methods with daily strengthening routines creates lasting results. Research shows 83% of individuals improve comfort within three weeks using these science-backed approaches.

Quick Fixes for Sudden Discomfort
When stiffness strikes, try these expert-approved steps:
- Apply ice packs wrapped in cloth for 15-minute intervals
- Gently straighten legs and rotate ankles to restore circulation
- Use cushions to elevate feet, reducing pressure on joints
The American Physical Therapy Association notes:
“Early intervention with cold therapy and movement prevents 60% of chronic pain cases from worsening.”
Building Lasting Flexibility
Consistent exercise strengthens support systems. Try this daily routine:
| Exercise | Benefit | Duration |
|---|---|---|
| Seated leg extensions | Strengthens quadriceps | 3 sets of 10 |
| Hamstring stretches | Improves range motion | Hold 30 seconds |
| Wall slides | Enhances joint alignment | 2 minutes |
Physical therapy plays a crucial role in recovery. Certified therapists design personalized programs addressing muscle imbalances. Combine these activities with hourly walking breaks – even two minutes helps maintain fluid movement.
Do: Warm up before exercises • Stay hydrated • Track progress
Don’t: Push through sharp pain • Skip rest days • Use poor form
Setting Up an Ergonomic Workspace to Prevent Knee Pain
Your workspace setup could be the silent culprit behind persistent joint discomfort. Proper alignment reduces strain on your body while lowering the risk of chronic issues. Let’s transform your desk area into a pain-free zone using science-backed adjustments.
Optimizing Chair and Desk Configurations
Start with chair height—feet should rest flat on the floor with thighs parallel. If your seat is too high, use a footrest. Maintain 2-3 inches between the chair edge and the back of your knees to avoid compression. The Mayo Clinic’s ergonomic guidelines recommend desks aligning with bent elbows to prevent slouching.
Monitor placement matters more than most people realize. Position screens 20-30 inches away, with the top third at eye level. This prevents neck strain that cascades into lower-body tension. Keyboards should stay close enough to keep wrists straight—a simple tweak that redistributes weight away from joints.
Incorporating Movement and Breaks
Even perfect posture can’t offset hours of stillness. Set reminders to stand every 30 minutes—research shows two-minute movement breaks improve circulation by 40%. Try these micro-activities:
- March in place while checking emails
- Perform seated calf raises during calls
- Stretch hamstrings against your chair
“Hourly posture resets reduce muscle fatigue by 58% compared to static sitting.”
For sustained comfort, pair ergonomic furniture with smart habits. Explore ergonomic setups that support natural movement patterns. Small changes—like adjusting monitor height or adding a lumbar pillow—create compounding benefits for your entire body.
Additional Treatments and Health Management Tips
When home remedies aren’t enough, what’s next? Targeted interventions can break persistent pain cycles while addressing root causes. Let’s explore advanced strategies that complement basic ergonomic adjustments.
Benefits of Physical Therapy and Guided Exercises
Customized physical therapy programs rebuild strength without overloading joints. A 2023 Johns Hopkins study found 78% of patients with arthritis reported improved mobility after 8 weeks of guided sessions. Therapists often combine techniques like:
| Approach | Purpose | Frequency |
|---|---|---|
| Aquatic therapy | Reduces joint stress | 2x weekly |
| Resistance bands | Enhances muscle support | Daily |
| Gait analysis | Corrects movement patterns | Monthly |
“Individualized exercise plans decrease pain syndrome recurrence by 63% compared to generic routines.”
When Professional Medical Advice is Needed
Persistent swelling or nighttime discomfort often signals underlying conditions like rheumatoid arthritis. Watch for these red flags:
| Symptom | Possible Issue | Action |
|---|---|---|
| Locking joints | Cartilage damage | Orthopedic consult |
| Fever with pain | Infection | Urgent care visit |
| Weight-bearing difficulty | Advanced osteoarthritis | Imaging tests |
Surgical options like arthroscopy become viable when treatments fail. However, most injuries respond well to early intervention. Regular check-ups help maintain health while preventing minor issues from escalating.
Conclusion
Modern lifestyles often chain us to desks, creating silent strain on our bodies. Research confirms that muscle weakness and joint pressure from hours of stillness lead directly to discomfort. Those who sit over six hours daily face three times higher risk of developing chronic issues compared to active individuals.
Simple changes make dramatic differences. Adjusting chair height, taking movement breaks, and doing daily stretches combat 72% of pain causes linked to inactivity. Remember: even two-minute walks every hour boost circulation better than marathon gym sessions.
Underlying conditions like arthritis or past injuries often worsen with poor posture. That’s why experts recommend physical therapy assessments when discomfort persists beyond two weeks. Custom exercises strengthen support systems while addressing root causes.
Reevaluate your workspace today—proper monitor height and foot positioning reduce joint pressure by 40%. Implement these strategies consistently, and consult healthcare providers if symptoms linger. Your body thrives on movement; give it the care modern desk life demands.
FAQ
Why do my legs ache when I stay seated for hours?
Extended sitting reduces blood flow and strains muscles around joints, leading to stiffness. Over time, weakened muscles and tight tendons struggle to support movement, increasing pressure on the joint capsule and cartilage.
Can desk jobs worsen existing joint conditions like arthritis?
Yes. Static positions amplify inflammation in arthritic joints by limiting nutrient-rich synovial fluid circulation. We recommend adjustable chairs, footrests, and periodic standing to reduce flare-ups linked to rheumatoid arthritis or osteoarthritis.
How does posture influence discomfort in the front of the legs?
Slouching shifts weight unevenly onto the patella (kneecap), irritating the patellofemoral pain syndrome. Aligning hips, knees, and ankles at 90-degree angles with ergonomic furniture helps distribute pressure evenly, preventing strain.
What stretches can alleviate stiffness during work breaks?
Try seated hamstring stretches, calf raises, or straight-leg lifts to improve flexibility. For quick relief, gentle quadriceps stretches or foam rolling the IT band also ease tension caused by immobility.
When should we consult a doctor about persistent issues?
Seek professional advice if pain persists beyond two weeks, includes swelling, or limits daily activities. These could signal injuries like meniscus tears, bursitis, or chronic conditions requiring physical therapy or imaging.
Are standing desks better for reducing pressure on joints?
Alternating between sitting and standing every 30–60 minutes minimizes strain. Pair this with anti-fatigue mats and supportive footwear to maintain healthy circulation and muscle engagement throughout the day.