The anterior knee plays a crucial role in lower body movement and stability. Understanding its anatomy, common injuries, and preventive measures is essential for maintaining knee health and preventing injuries. In this article, we will explore the anatomy of the anterior knee, common injuries affecting the area, and preventive measures for anterior knee health.
Key Takeaways
- Proper training techniques can significantly reduce the risk of ACL injuries.
- Strengthening quadriceps muscles is important for maintaining anterior knee health.
- Flexibility and mobility play a vital role in preventing anterior knee injuries.
- Patellar tendinopathy can impact anterior knee health and should be addressed early.
- Meniscus tears are closely related to anterior knee health and should be managed with care.
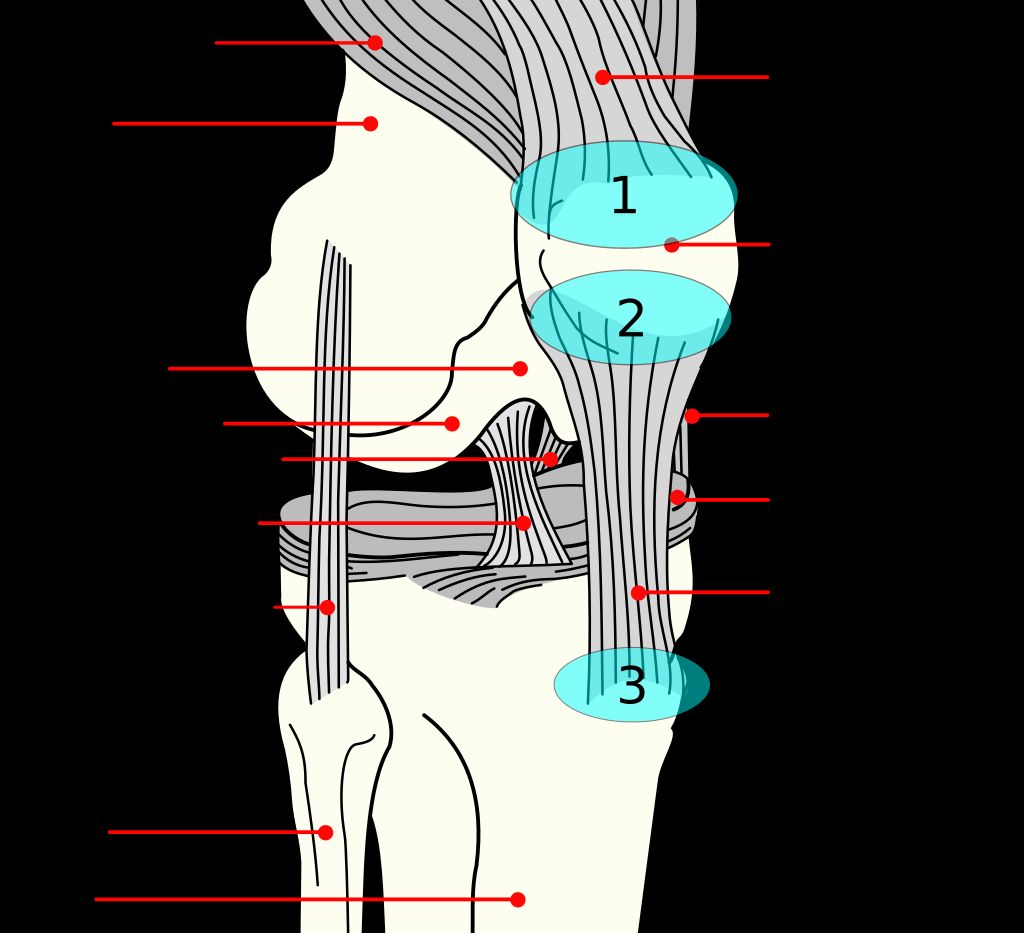
The Anatomy of the Anterior Knee

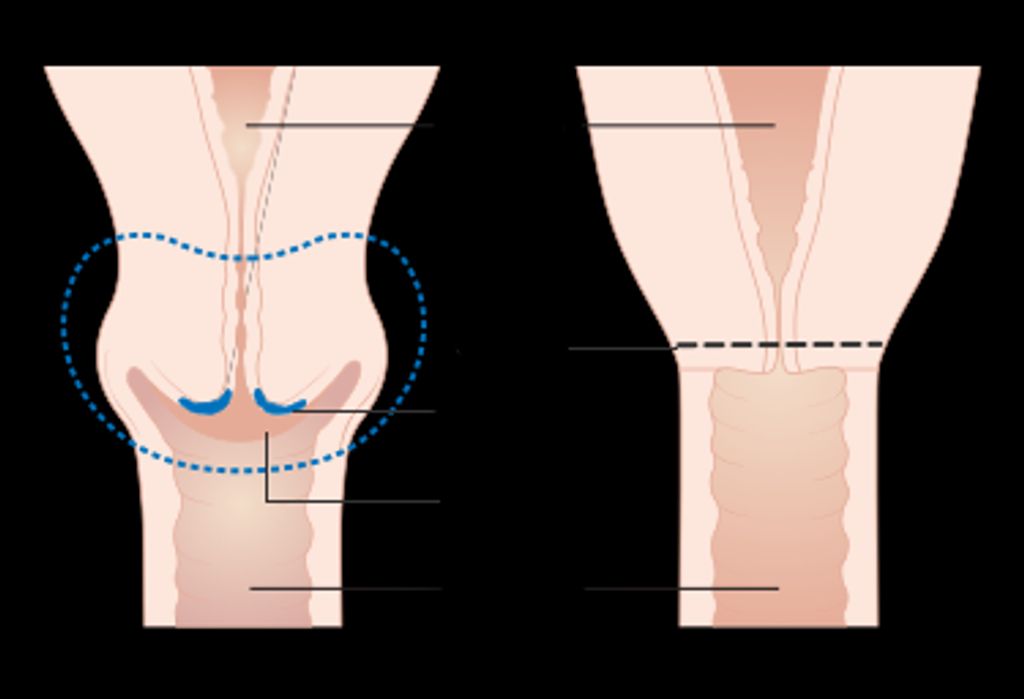
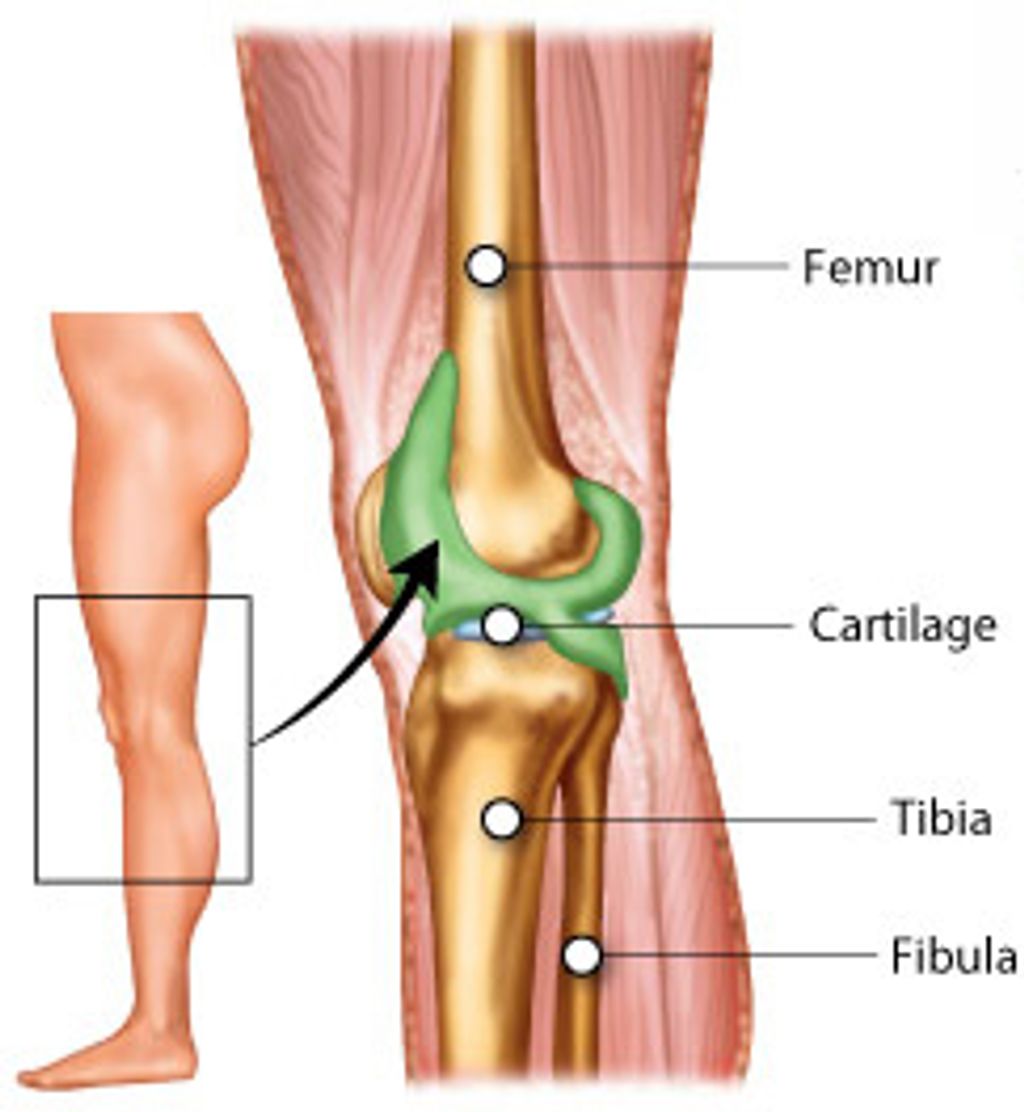
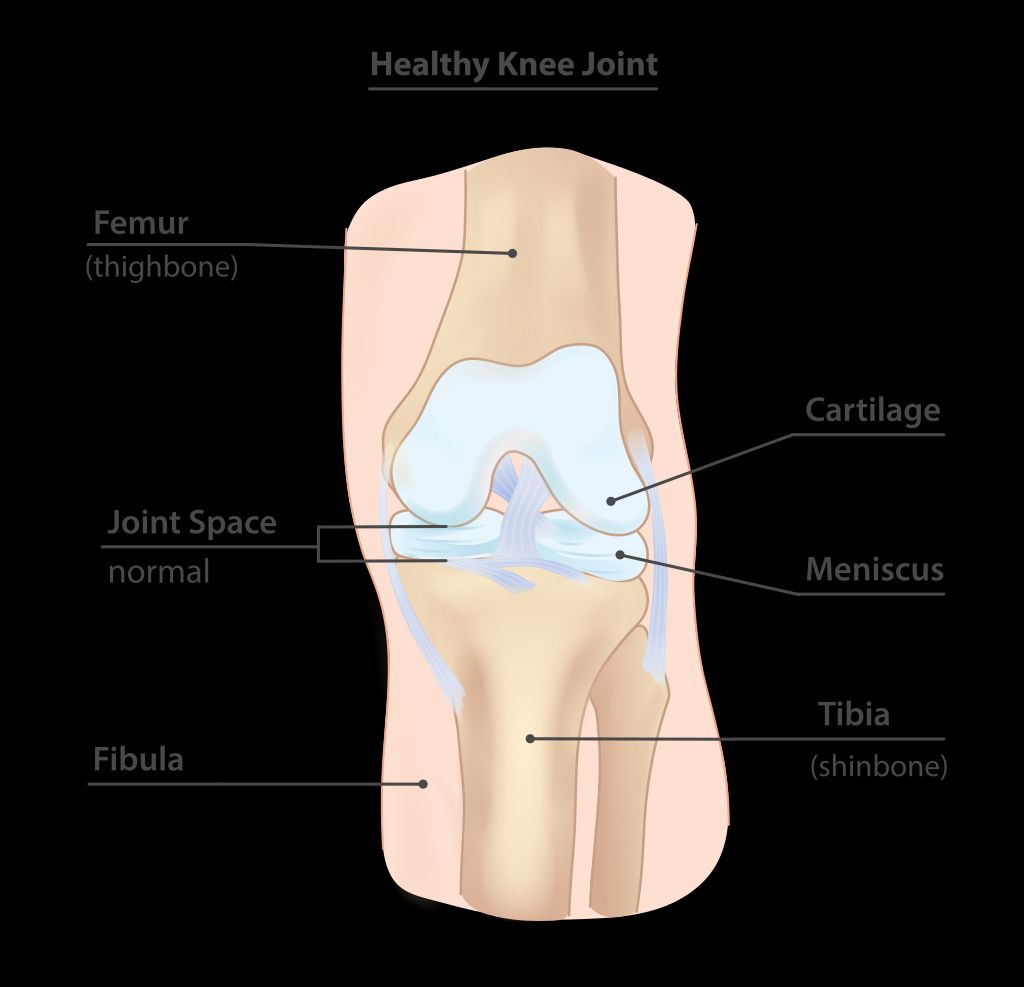
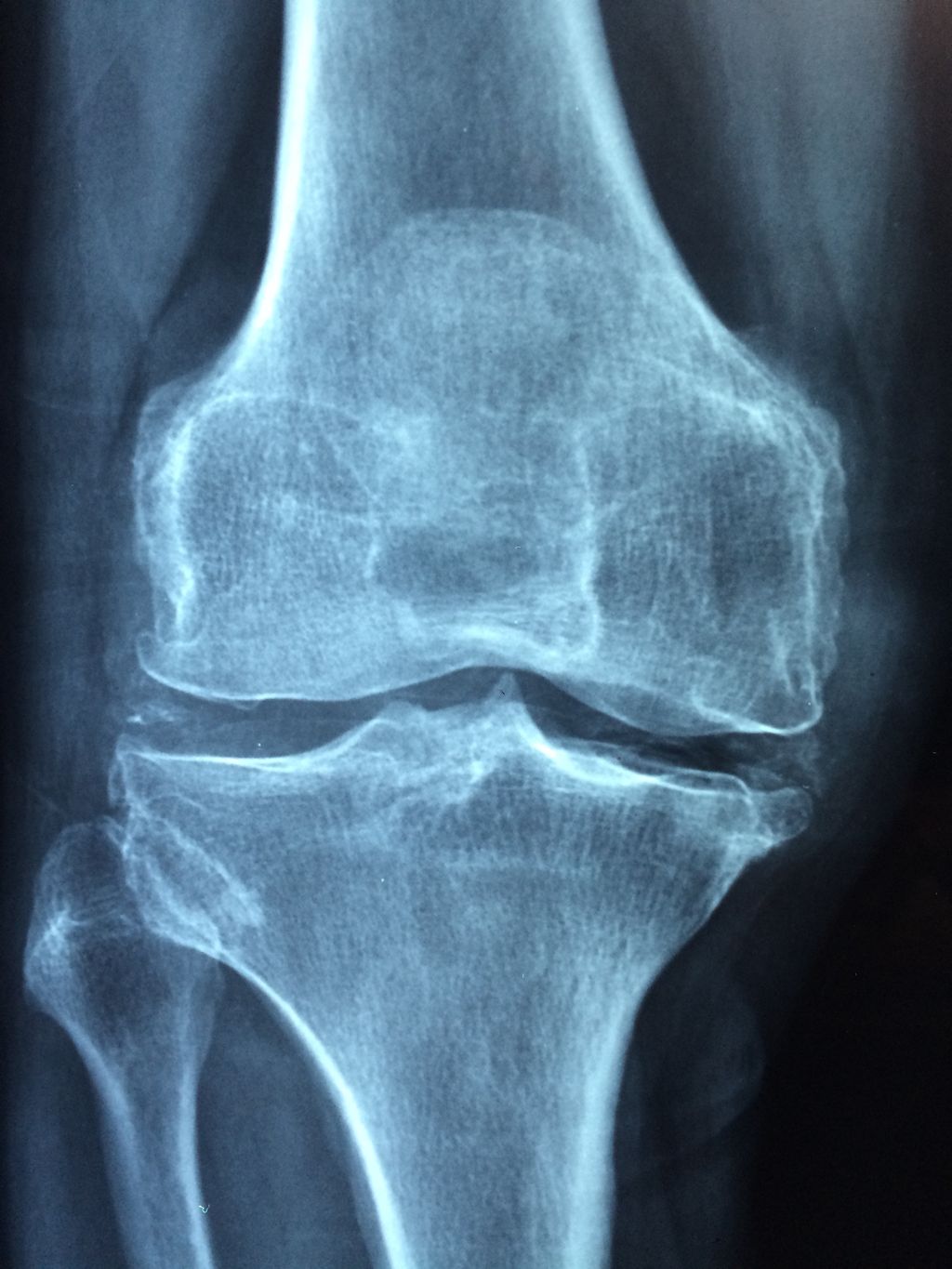
Understanding the Patellofemoral Joint
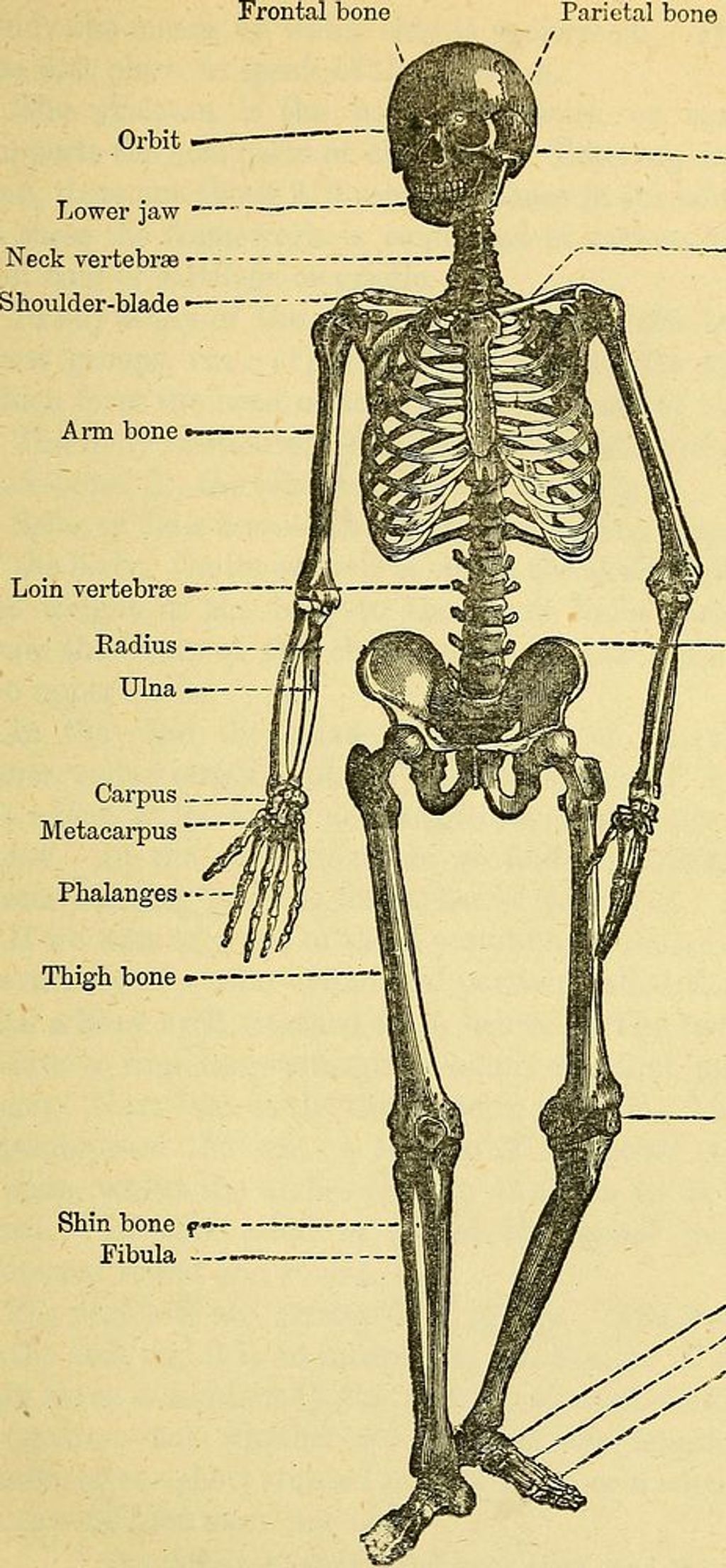
We often overlook the complexity of the knee joint, yet it is crucial for our mobility. The patellofemoral joint is a unique hinge that allows for the intricate movement of the knee. It is formed by the patella, or kneecap, articulating with the femur. This joint is essential for activities such as walking, running, and jumping, as it facilitates the extension and flexion of the knee.
Stability and smooth movement are provided by a combination of muscular support and ligamentous structures. The surrounding muscles, particularly the quadriceps, play a pivotal role in maintaining this stability. The cartilage lining the joint surfaces ensures that movement is fluid and minimizes friction.
- The patella improves the mechanical advantage of the quadriceps tendon.
- Articular cartilage reduces friction and distributes load.
- Ligaments and tendons provide structural support.
Remember, maintaining the health of the patellofemoral joint is vital for overall knee function and longevity. Regular exercise and proper technique can help preserve this joint’s integrity.
The Role of Quadriceps Tendon
We often overlook the critical role that the quadriceps tendon plays in our anterior knee health. This robust tendon is the confluence of the four muscles that comprise the quadriceps muscle group, and it is essential for the proper function of the knee joint. It is responsible for transmitting the force generated by the quadriceps muscles to the patella, enabling knee extension.
The integrity of the quadriceps tendon is vital for activities such as walking, running, and jumping. A healthy tendon is characterized by its ability to withstand significant loads while maintaining flexibility. We must pay attention to the signs of overuse or strain, which can lead to conditions such as tendinopathy.
Tip: Regularly performing exercises that target the quadriceps can help maintain the strength and resilience of the quadriceps tendon, potentially preventing injury.
Understanding the balance between strength and flexibility is crucial in preserving the health of the quadriceps tendon. We should incorporate both resistance training and stretching into our fitness routines to ensure this tendon remains strong and supple.
Function of the Patellar Ligament
We must appreciate the patellar ligament as a critical component in the mechanism of knee extension. This robust structure, originating from the patella and inserting into the tibial tuberosity, plays a pivotal role in transmitting the force generated by the quadriceps muscle to the lower leg, enabling us to perform activities such as walking, running, and jumping.
The integrity of the patellar ligament is essential for maintaining anterior knee health. Any compromise to its function can lead to a cascade of issues, affecting not only mobility but also the stability of the knee joint. It’s important to recognize the signs of patellar ligament dysfunction, which may include pain, swelling, and a decreased ability to straighten the knee.
Prevention and early intervention are key in managing the health of the patellar ligament. Regularly engaging in exercises that strengthen the surrounding musculature can help mitigate the risk of injury. Additionally, maintaining a healthy weight can reduce the stress placed on the ligament during daily activities.
Tip: Always warm up before engaging in high-impact activities to prepare the patellar ligament for the stresses of exercise.
Common Injuries Affecting the Anterior Knee

Patellar Tendinopathy and Its Impact
We often encounter patellar tendinopathy, commonly known as jumper’s knee, in individuals who engage in sports that involve frequent jumping and landing. This condition arises from the overuse of the patellar tendon, which connects the kneecap to the shinbone, leading to pain and inflammation.
The symptoms can range from mild discomfort to severe pain that can impede athletic performance and daily activities. Early diagnosis and intervention are crucial in managing the condition effectively. Here’s a brief overview of the typical progression of symptoms:
- Initial pain after activity, often ignored by athletes
- Persistent pain during and after activity
- Pain affecting performance
- Severe pain, even during daily tasks
Tip: Rest and ice can alleviate symptoms in the early stages, but persistent pain warrants professional assessment and intervention.
Management strategies include a combination of rest, physical therapy, and in some cases, surgery. It’s imperative to address patellar tendinopathy promptly to prevent chronic issues that can lead to complications such as osteoarthritis.
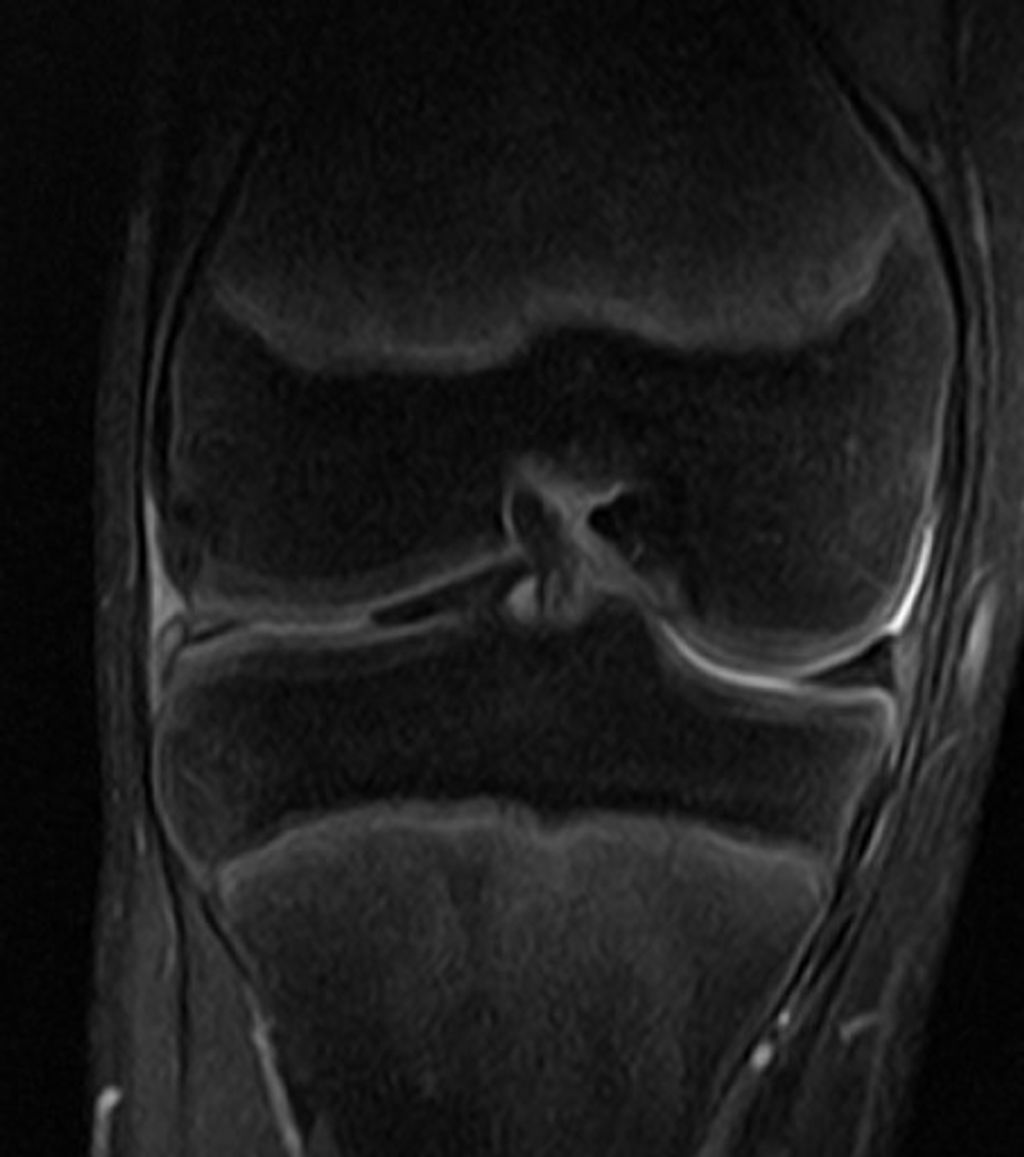
Anterior Cruciate Ligament (ACL) Injuries
After discussing the impact of Anterior Cruciate Ligament (ACL) Injuries, it is crucial for us to emphasize the importance of strengthening quadriceps muscles. This can be achieved through targeted exercises such as leg extensions, squats, and lunges. Additionally, maintaining proper form during these exercises is essential to prevent further strain on the knee.
Furthermore, incorporating flexibility and mobility exercises into our routine can significantly reduce the risk of anterior knee injuries. This includes activities such as yoga, Pilates, and dynamic stretching. Enhancing our range of motion can help in maintaining the health and stability of the knee joint.
It is also beneficial to incorporate a balanced training regimen that focuses on both strength and flexibility. This can be achieved through a combination of resistance training, cardiovascular exercises, and flexibility routines. Balancing these elements will contribute to overall knee health and reduce the likelihood of injuries.
It is important to consult with a qualified healthcare professional or physical therapist to develop a personalized preventive plan based on individual needs and existing knee health.
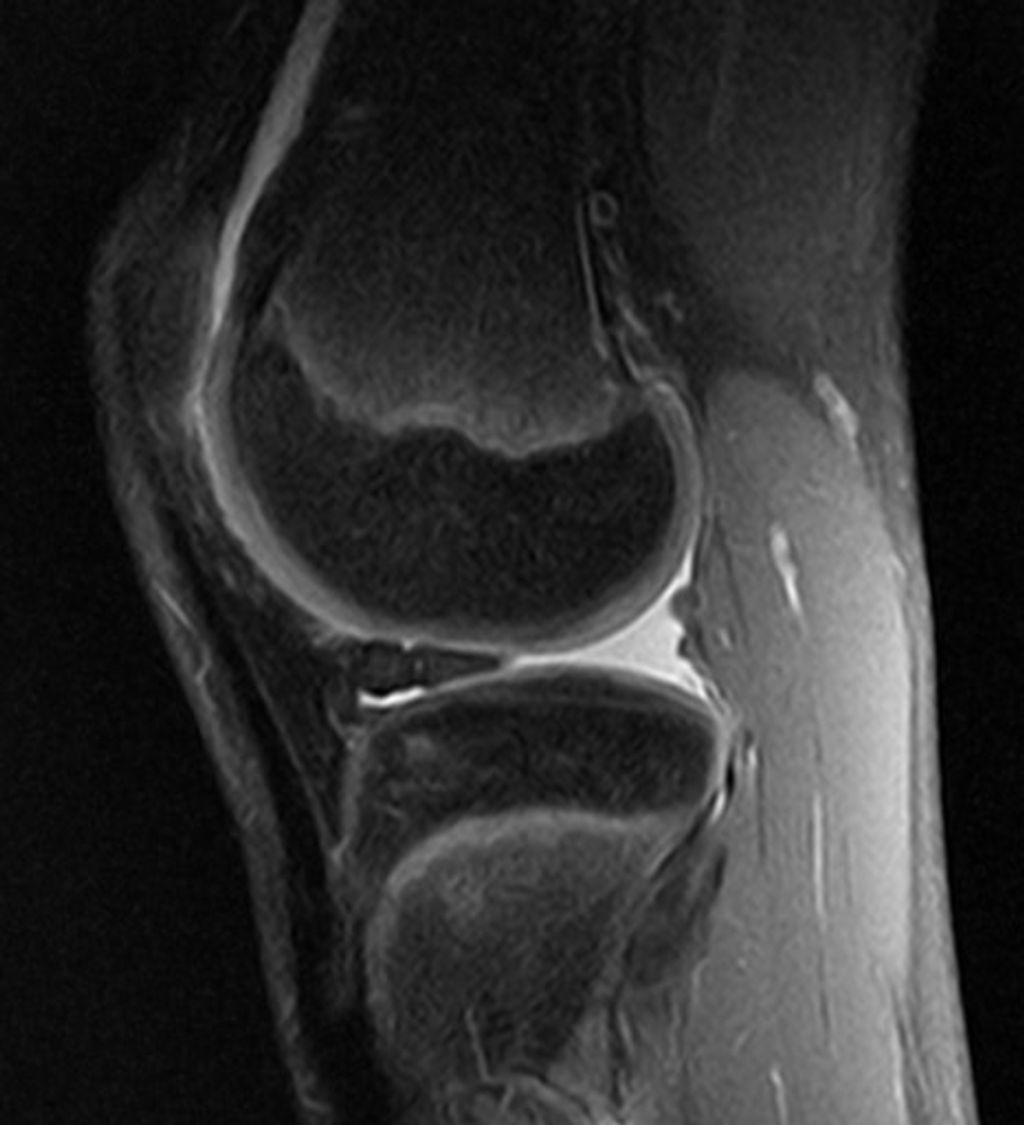
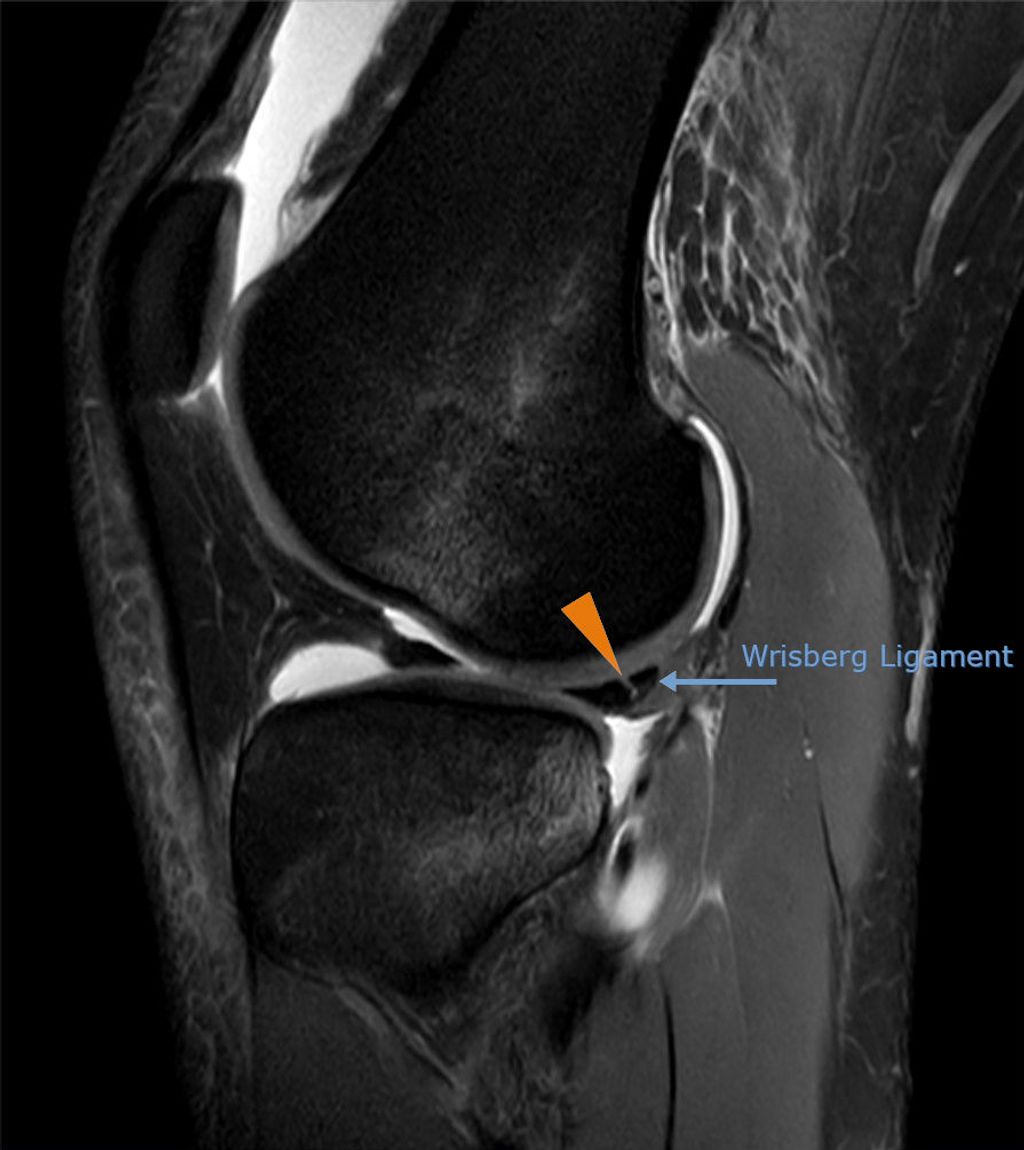
Meniscus Tears and Their Relation to Anterior Knee Health
Meniscus tears are a common injury that can significantly impact anterior knee health. These tears often occur due to sudden twisting or direct impact on the knee. Early diagnosis and appropriate treatment are crucial for preventing long-term complications. In some cases, surgical intervention may be necessary to repair the torn meniscus and restore knee function.
It’s important to note that the severity of meniscus tears can vary, ranging from minor tears to complete ruptures. The choice of treatment, whether conservative or surgical, depends on the extent of the tear and the individual’s overall knee health. Rehabilitation plays a key role in the recovery process, focusing on strengthening the surrounding muscles and improving range of motion.
Preventive measures such as proper warm-up, stretching, and using protective gear can help reduce the risk of meniscus tears. Additionally, maintaining a healthy body weight and avoiding activities that place excessive stress on the knees can contribute to long-term anterior knee health.
It’s essential to seek professional medical advice if you experience symptoms of a meniscus tear, such as pain, swelling, or limited mobility. Early intervention and appropriate management can significantly impact the recovery and long-term health of the knee.
Preventive Measures for Anterior Knee Health

Importance of Strengthening Quadriceps Muscles
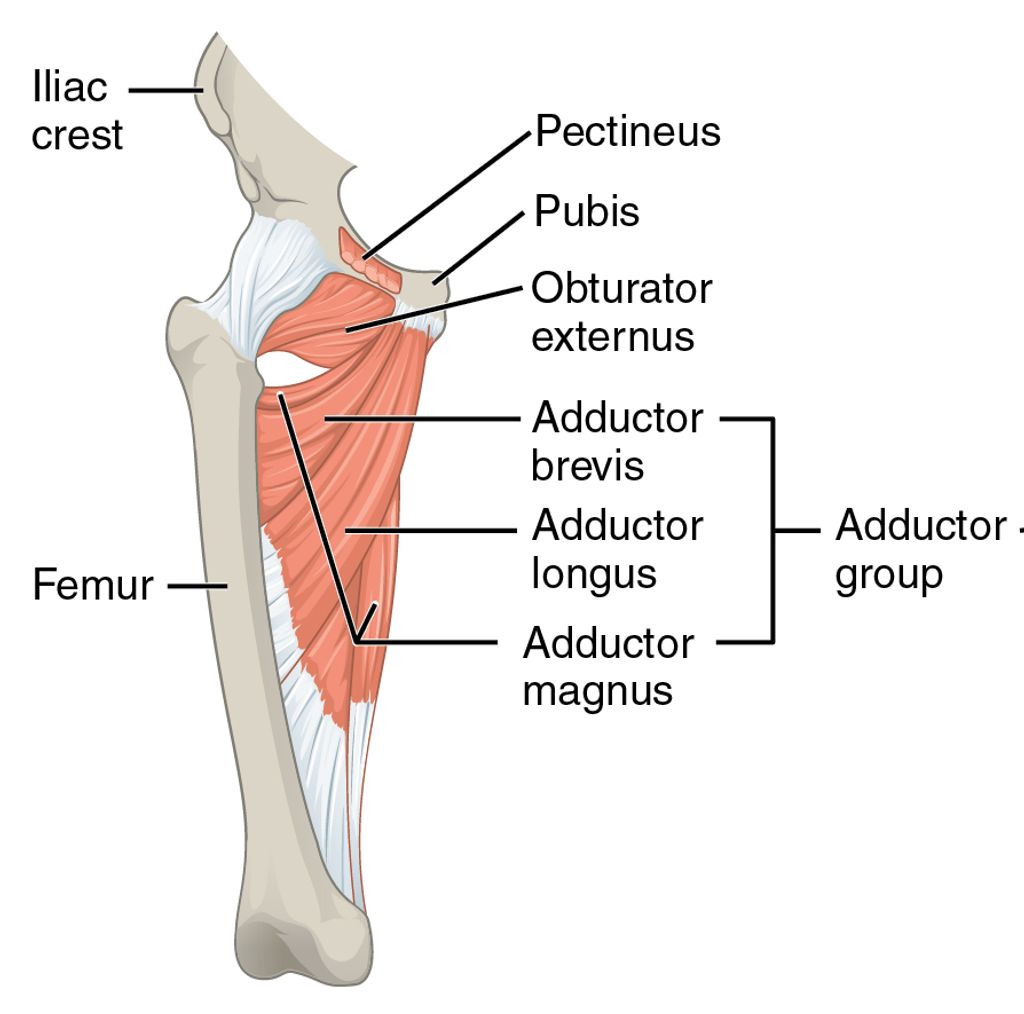
We recognize the quadriceps muscles as a critical component in maintaining anterior knee health. Their strength and conditioning play a pivotal role in stabilizing the patellofemoral joint, which is essential for knee function and mobility.
By engaging in regular quadriceps strengthening exercises, we can significantly reduce the risk of knee injuries. These exercises help in distributing the load across the knee joint more evenly, thereby alleviating excessive pressure on any single structure.
- Here are some effective quadriceps strengthening exercises:
- Straight leg raises
- Seated knee extensions
- Squats with proper form
- Lunges, ensuring knee alignment
Tip: Always warm up before starting your exercise routine to prepare the muscles and reduce the risk of injury.
It is also important to gradually increase the intensity of these exercises to avoid overstraining the muscles, which can lead to counterproductive outcomes. We must be mindful of the balance between strengthening and overuse, especially for individuals recovering from injuries such as ACL surgery.
Proper Training Techniques for Reducing ACL Injury Risk
We recognize the critical role that proper training techniques play in mitigating the risk of ACL injuries. These injuries can be debilitating and often require extensive recovery time, as evidenced by clients who experience setbacks even 10 weeks post-surgery. To prevent such outcomes, we advocate for a multifaceted approach to training.
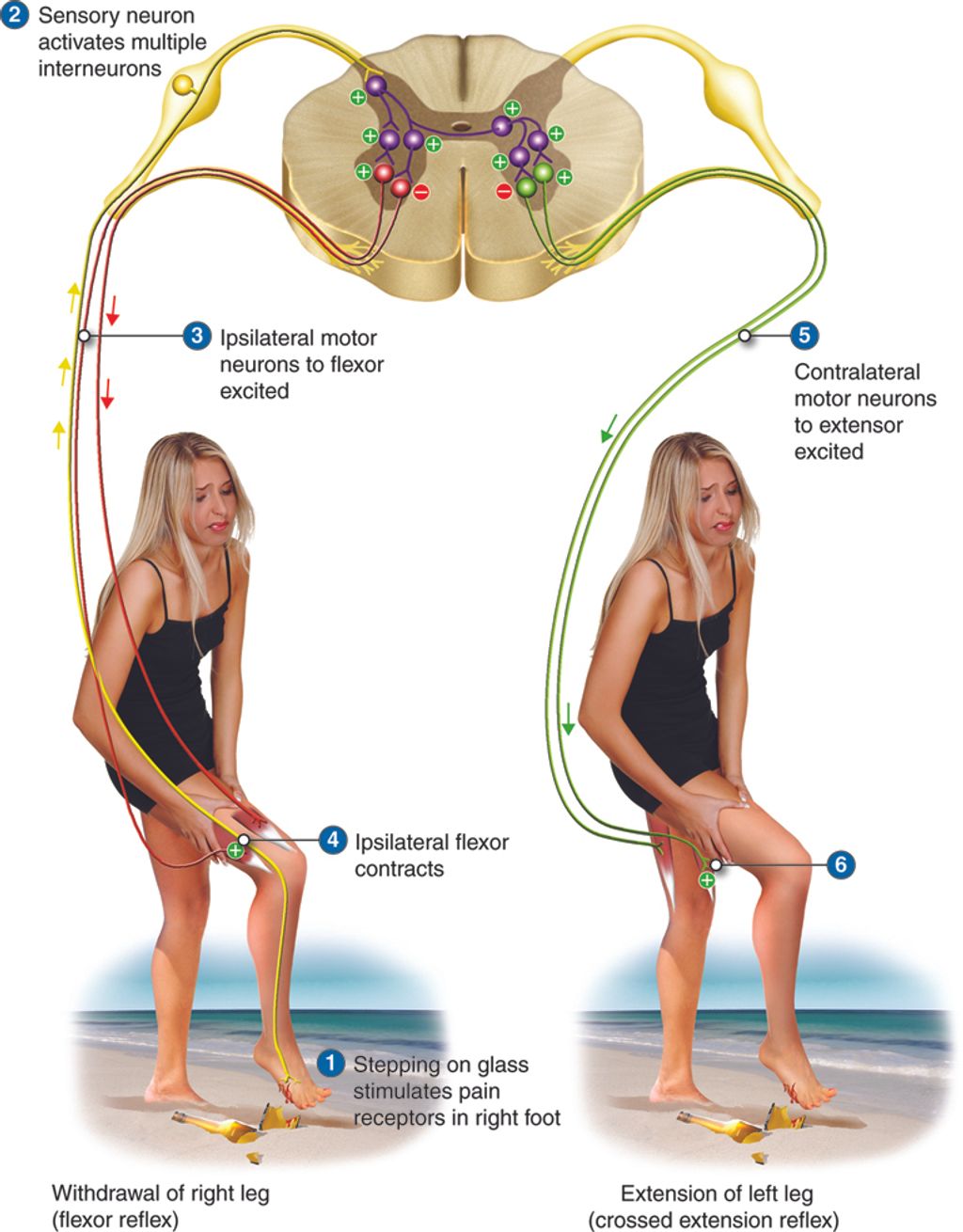
Firstly, we emphasize the importance of neuromuscular training, which includes exercises that improve balance, coordination, and proprioception. This type of training has been shown to significantly reduce the incidence of ACL injuries, especially in athletes.
- Plyometric exercises to enhance power and agility
- Balance training to improve stability
- Strength training focusing on the hamstrings and hips
Additionally, we stress the importance of gradual progression in training intensity and volume to allow the body to adapt safely. It is also crucial to ensure proper technique in all exercises to avoid undue stress on the knee joint.
Tip: Always warm up thoroughly before engaging in any form of exercise to prepare the muscles and joints for the physical activity ahead.
Role of Flexibility and Mobility in Preventing Anterior Knee Injuries
Flexibility and mobility play a crucial role in maintaining anterior knee health. Proper range of motion in the knee joint is essential for preventing injuries and ensuring optimal function. Additionally, incorporating dynamic stretching and mobility exercises can improve joint stability and reduce the risk of overuse injuries. It is important to note that a balanced approach to flexibility and mobility training is key to promoting overall knee health and preventing common injuries.
Conclusion
In conclusion, the maintenance of anterior knee health is of paramount importance for overall physical well-being. Through proper care and attention, individuals can mitigate the risk of various knee-related conditions and maintain an active lifestyle. It is imperative to prioritize preventive measures and seek professional guidance when necessary to ensure the longevity of anterior knee health.
Frequently Asked Questions
What are some common causes of anterior knee pain?
Anterior knee pain can be caused by overuse, muscle imbalances, poor biomechanics, and traumatic injuries. It is important to identify the specific cause in order to develop an appropriate treatment plan.
How can I prevent anterior knee injuries during physical activities?
Engaging in proper warm-up and cool-down routines, using proper footwear, maintaining proper technique, and incorporating strength and flexibility training can help prevent anterior knee injuries during physical activities.
What are the symptoms of patellar tendinopathy?
Symptoms of patellar tendinopathy may include pain and tenderness around the patellar tendon, swelling, and difficulty with activities that involve jumping or bending the knee. Seeking medical evaluation is important for accurate diagnosis and treatment.
Are there specific exercises to strengthen the quadriceps muscles?
Yes, exercises such as squats, lunges, leg presses, and step-ups can help strengthen the quadriceps muscles. It is important to perform these exercises with proper form and under the guidance of a qualified fitness professional.
Can ACL injuries be prevented through training and conditioning?
While it is not possible to completely eliminate the risk of ACL injuries, training and conditioning programs that focus on improving strength, balance, and neuromuscular control can help reduce the risk of ACL injuries, especially in athletes.
What role does flexibility play in preventing anterior knee injuries?
Flexibility plays a crucial role in preventing anterior knee injuries by improving joint mobility, reducing muscle tightness, and enhancing overall movement patterns. Incorporating regular stretching and mobility exercises into a fitness routine can help maintain optimal flexibility.