Imagine you’re in the middle of painting, but knee pain stops you. Many face this when they have a meniscus tear. Climbing ladders then becomes a big challenge, affecting your project and mobility.
Dealing with ladder climbing and a meniscus tear is tough. We aim to give you expert advice to stay safe. Our tips help you avoid more injuries and keep working on your projects.
Key Takeaways
- Safely assess your knee condition before climbing a ladder.
- Understand the proper techniques for ladder climbing with a meniscus injury.
- Learn how to prevent further knee damage while on a ladder.
- Discover exercises to strengthen your knee before and after ladder climbing.
- Explore alternative solutions for painting projects that minimize ladder use.
Understanding Knee Pain: Common Causes
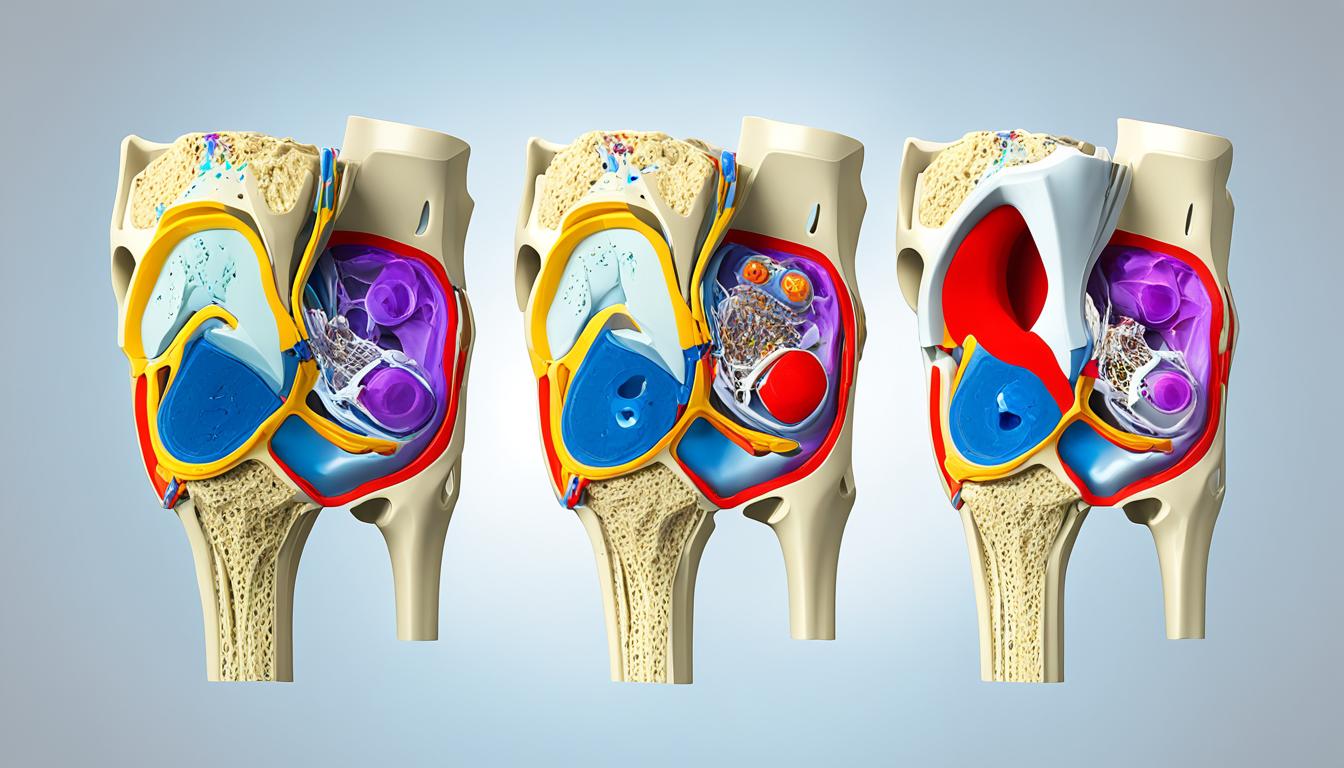
Knee pain comes from many sources. It’s key to know these causes to avoid more harm. Activities like ladder climbing put extra stress on our knees. This can make existing problems worse or cause new ones.
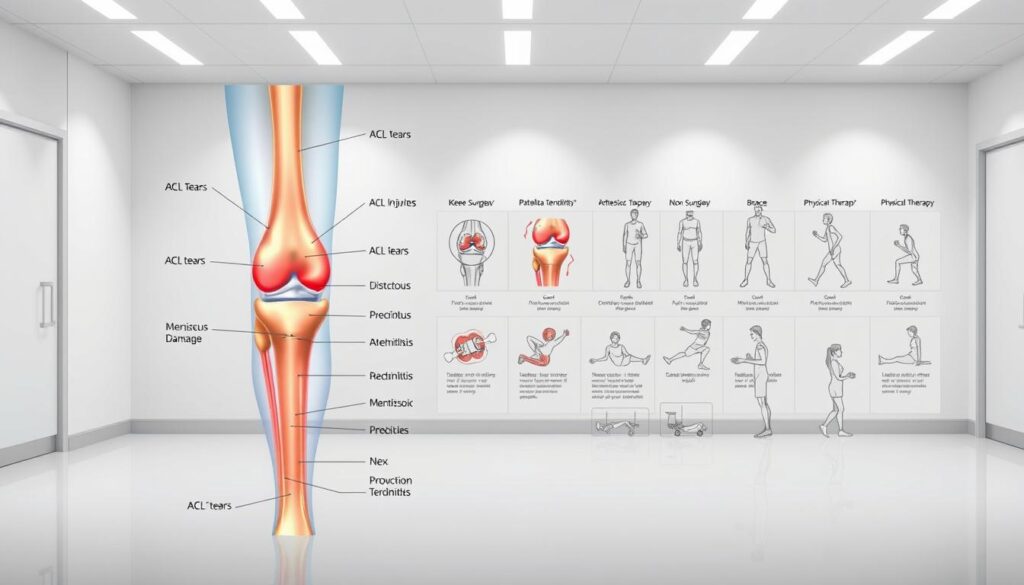
Types of Knee Pain
Knee pain falls into two main groups: acute injuries and chronic conditions. Acute injuries happen suddenly, like from a fall. Chronic conditions develop over time, often from repeated strain or wear.
Some common knee pain types include meniscus tears, ligament sprains, and tendonitis. Knowing the exact type of pain helps find the right treatment and ways to prevent it.
Why Ladder Work Can Exacerbate Pain
Climbing ladders puts a lot of strain on the knees, especially when bending or standing on uneven ground. This strain can make knee problems worse or cause new ones like patellofemoral pain syndrome. The constant stress from ladder work can lead to knee inflammation and pain.
To reduce the risk of making knee pain worse, it’s important to understand how ladder work affects the knee. Knowing this helps us take steps to lessen the strain and protect our knees.
Safety Measures When Using a Ladder

To stay safe while using a ladder, we need to take certain steps. Ladder climbing can be dangerous, especially for those with knee problems. By picking the right ladder and setting it up right, we can lower the chance of accidents.
Choosing the Right Ladder
Picking the right ladder is key. Think about how high you need to go and how much weight the ladder can hold. For painting, a ladder with a strong base and non-slip feet is best. Look for ladders with comfy rungs and think about the material. Aluminum ladders are light, while fiberglass ladders are more stable.
| Ladder Type | Material | Weight Capacity |
|---|---|---|
| Step Ladder | Aluminum | 300 lbs |
| Extension Ladder | Fiberglass | 250 lbs |
Proper Ladder Setup
After picking the right ladder, setting it up correctly is crucial for safety. Make sure the ladder is on a solid, level ground. Having someone hold the ladder can also help. The ladder’s angle is important too; it should be at a 75-degree angle or one foot away from the wall for every four feet of ladder height.
By following these tips, we can make ladder climbing safer. Remember, safety steps are not just suggestions; they’re essential to avoid serious injuries.
Preparing for Your Painting Project

Getting ready for painting is more than just picking up supplies. It also means getting your body ready to avoid knee injury.
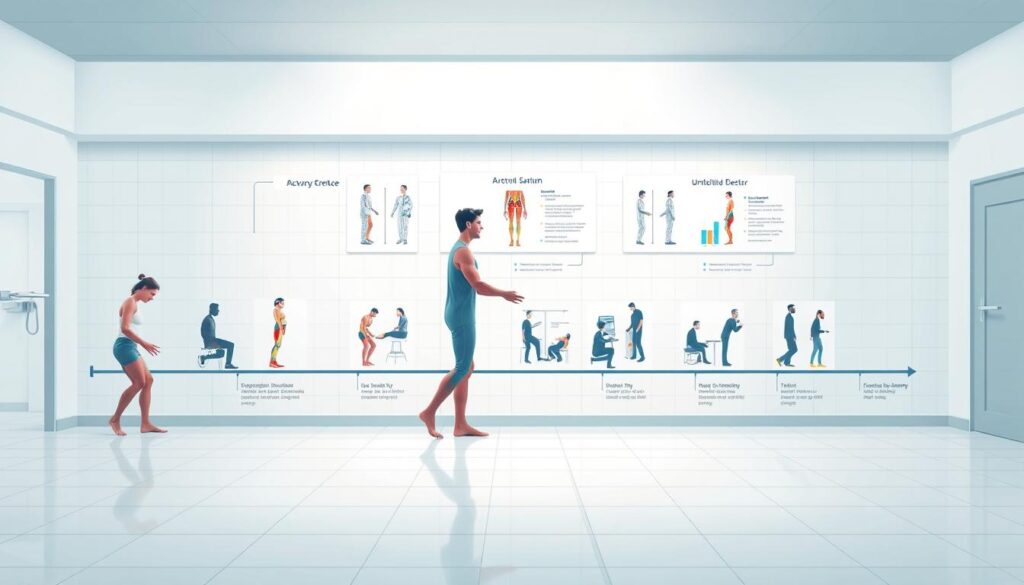
Stretching Exercises Before Climbing
Do some stretching exercises before you start climbing. This helps your knees a lot. Try:
- Leg swings to loosen up your leg muscles
- Knee bends to prepare your knees for the climb
- Calf raises to strengthen your calf muscles, which support your knees
Essential Gear to Minimize Knee Strain
Wearing the right gear can also help your knees. Use:
- Knee pads for extra cushioning and support
- Supportive footwear to stabilize your knees
- Comfortable clothing that allows for a full range of motion
With these steps, you can lower the chance of knee pain and injury while painting.
Painting Techniques to Reduce Knee Strain
There are ways to lessen knee strain while painting on a ladder. Painting can put a lot of pressure on our knees, especially if we have conditions like meniscus tears. Using the right techniques can help avoid making knee pain worse.
Opt for a Brush Instead of a Roller
Choosing a brush over a roller can help reduce knee strain. Brushes allow for more precise strokes and need less force, which is easier on the knees. Plus, they help you paint more accurately, so you might not have to climb the ladder as much.
Take Breaks to Relieve Pressure
It’s important to take breaks to ease knee strain. Stepping down from the ladder often can help take the pressure off your knees. These breaks are a chance to stretch and prevent knee pain.
By using these techniques, we can make painting easier on our knees. This is especially helpful for those with knee pain or meniscus tear symptoms.
When to Seek Medical Advice
Knee pain can really get in the way of doing things. There are times when you need to see a doctor. If you’re feeling pain in your knee while on a ladder, it’s important to know when to get help.
Signs Your Knee Pain Needs Attention
There are signs that mean you should see a doctor. These include:
- Persistent pain that doesn’t improve with rest
- Swelling or redness around the knee
- Instability or feeling like the knee is going to give way
- Warmth or tenderness to the touch
- Loss of mobility or difficulty straightening the knee
If you notice any of these, it’s best to talk to a healthcare professional. Ignoring these signs can lead to further complications.
Recommended Specialists for Knee Pain
Choosing the right specialist is crucial for knee pain. Here’s a table of specialists you might consider:
| Specialist | Description |
|---|---|
| Orthopedic Surgeon | Specializes in surgical treatments for musculoskeletal disorders, including knee pain. They can perform knee surgery if necessary. |
| Rheumatologist | Expert in diagnosing and treating rheumatic diseases that can cause knee pain. |
| Physical Therapist | Can help improve knee mobility and strength through targeted exercises. |
An orthopedic surgeon is often the first choice for serious knee pain or when surgery is needed. They can give a detailed diagnosis and suggest the best treatment.
Home Remedies for Knee Pain Relief
Home remedies are a simple way to handle knee pain and boost your quality of life. We often seek easy, effective solutions to ease discomfort before seeking medical help. Two popular methods are ice and heat therapy, and over-the-counter pain relief.
Ice and Heat Therapy
Ice and heat therapy are easy yet effective for knee pain. Ice therapy reduces swelling and numbs pain, great for sudden injuries or pain spikes. Heat therapy, on the other hand, relaxes muscles and boosts blood flow, helping with long-term pain and stiffness.
To use ice, wrap an ice pack in a towel and apply it for 15-20 minutes, several times a day. For heat, try a warm bath, heating pad, or a warm cloth on your knee. It’s key to alternate between ice and heat based on your pain type.
“The application of ice or heat can significantly alter the pain perception and is a crucial component of a comprehensive pain management plan.”
Over-the-Counter Pain Relief Options
Over-the-counter (OTC) pain meds are also effective for knee pain. Common ones are acetaminophen and ibuprofen. Acetaminophen mainly relieves pain, while ibuprofen also fights inflammation.
- Always follow the recommended dosage on the label.
- Consult with a healthcare provider if you’re unsure about interactions with other medications.
- Be aware of potential side effects and contraindications.
By adding these home remedies to your daily routine, you can better manage knee pain. This lets you enjoy activities like painting on a ladder more comfortably.
Prolonging Knee Health During Painting
To enjoy painting without harming our knees, we need to focus on knee health. Painting on a ladder can be tough on our knees, especially for those with a torn meniscus. By keeping our knees strong and moving regularly, we can protect them.
Tips for Maintaining Strong Knees
Keeping our knees strong involves exercises and careful movements. Physical therapy helps strengthen knee muscles, offering better support and injury prevention. Exercises like squats, lunges, and leg presses are helpful. Also, using the right ladder techniques and taking breaks can ease knee strain.
| Exercise | Benefit | Frequency |
|---|---|---|
| Squats | Strengthens quadriceps and hamstrings | 3 sets of 10 reps, 3 times a week |
| Lunges | Improves balance and strengthens knee muscles | 3 sets of 10 reps (per leg), 3 times a week |
| Leg Presses | Targets quadriceps, hamstrings, and glutes | 3 sets of 12 reps, 3 times a week |
Importance of Regular Movement
Regular movement is key for healthy knees. Sitting still for too long can make knees stiff and painful, especially for those with injuries. Adding gentle exercises to our day keeps knees flexible and lowers injury risk. It’s also important to listen to our bodies and rest when needed.
By using these tips, we can keep our knees healthy while painting. Regular physical therapy, exercises, and careful movements are all important for a safe painting experience.
Equipment to Assist While Painting on a Ladder
To have a safe and fun painting time, the right tools are key. Using the right gear when painting on a ladder helps avoid knee pain and injuries.
Knee Pads and Supportive Gear
Knee pads are a simple yet effective way to protect your knees while working on a ladder. They offer cushioning and support, easing the pressure on your knees. Supportive gear, like knee braces, adds extra stability and protection. Pick knee pads or supportive gear based on your work and needed support.
Look for knee pads that are durable, comfortable, and adjustable. It’s also important to pick knee pads that fit your task. For example, if you’re working on a rough surface, you’ll need sturdier knee pads.
| Type of Knee Pad | Features | Best For |
|---|---|---|
| Hard Cap Knee Pads | Durable, protective | Rough surfaces, heavy-duty work |
| Soft Cap Knee Pads | Comfortable, flexible | General painting, smooth surfaces |
| Gel Knee Pads | Cushioned, shock-absorbing | Long periods of kneeling, comfort |
Choosing the Right Footwear
Along with knee pads, choosing the right footwear is crucial for stability and to prevent slipping on the ladder. Find shoes with good grip and a snug fit to keep your feet steady on the ladder.
- Non-slip soles
- Comfortable fit
- Ankle support
By using knee pads with the right shoes, you can greatly lower the risk of knee injury. This makes painting more comfortable and enjoyable.
Final Thoughts: Enjoying Your Painting Project
As we finish talking about managing knee pain while painting on a ladder, remember it’s not just about the end. It’s also about how we feel during it. By taking care of our knees, we can enjoy painting more without worrying about injuries.
It’s important to love the journey of creating. We can do this by following the tips we’ve shared. From picking the right ladder to stretching, every step matters.
Practical Adjustments for Future Projects
For future painting, we can reduce knee pain. Use knee pads and supportive gear. Also, pick shoes that help you stay stable on the ladder.
Maintaining Knee Health
Keeping our knees healthy is key to enjoying painting and other activities. Regular exercise and movement help make our knees stronger. This makes it easier to handle ladder work.
FAQ
What are the symptoms of a meniscus tear?
Symptoms include knee pain, swelling, and stiffness. Sometimes, we hear a popping sound when it happens.
How can I prevent further injury while climbing a ladder with a meniscus tear?
To avoid more harm, choose the right ladder and set it up right. Wear knee pads and supportive shoes.
What are the treatment options for a torn meniscus?
Treatments include physical therapy, pain meds, and sometimes surgery. An orthopedic surgeon can help decide the best treatment.
Can I continue with my painting projects if I have a meniscus tear?
Yes, you can keep painting. Just be careful to avoid making the injury worse. Use proper techniques, take breaks, and wear supportive gear.
When should I seek medical advice for knee pain?
Get medical help if your knee pain, swelling, or stiffness doesn’t go away. An orthopedic surgeon can find the cause and suggest treatment.
What are some home remedies for knee pain relief?
Try ice and heat, over-the-counter pain meds, stretching, and keeping a healthy weight. These can help ease knee pain.
How can I maintain strong knees while painting on a ladder?
Keep your knees strong by doing physical therapy, wearing supportive gear, and taking breaks. This helps relieve knee pressure.
What type of equipment can assist me while painting on a ladder?
Use knee pads, supportive gear, and the right shoes. They help protect and support your knees while painting.