Bending your legs shouldn’t feel like a battle. Yet millions experience sharp twinges or dull aches during one of humanity’s oldest motions. Could something as simple as lowering your body hold hidden risks?
Squatting appears in countless routines – from gym workouts to picking up groceries. But improper form, muscle imbalances, or underlying conditions can turn this functional movement into a source of joint stress. Discomfort often centers around the kneecap, though tendons and cartilage may also contribute to the issue.
This guide explores practical solutions rooted in sports medicine and rehabilitation science. We’ll break down how inflammation patterns differ between acute injuries and chronic overuse. You’ll also discover why temporary fixes rarely address the root cause of persistent knee pain.
Key Takeaways
- Multiple factors contribute to discomfort during squatting motions
- Early symptom recognition prevents long-term joint damage
- Home treatments like ice packs and compression offer immediate relief
- Targeted exercises strengthen supporting muscle groups
- Professional evaluation ensures proper diagnosis for chronic cases
Through evidence-based strategies, we empower readers to reclaim pain-free movement. Upcoming sections detail step-by-step prevention techniques and adaptive training modifications. Let’s transform how you approach this essential daily action.
Understanding Knee Pain When Squatting
The human body thrives on movement, but certain motions can reveal hidden vulnerabilities. Discomfort during bending often stems from complex interactions between bones, tendons, and soft tissues. While temporary soreness resolves quickly, persistent issues demand deeper investigation.
What is Knee Pain?
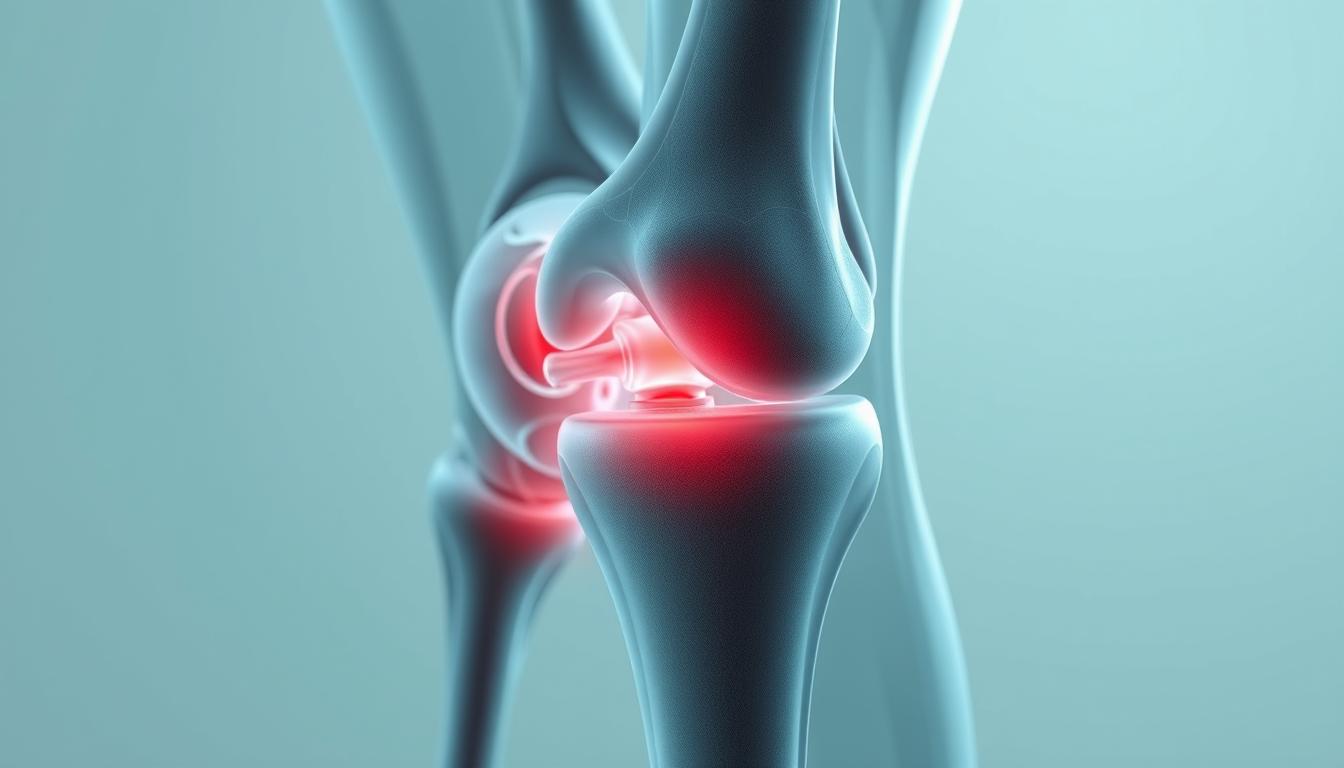
Joint discomfort ranges from acute twinges to chronic aching. Conditions like patellar tendonitis create inflammation below the kneecap, particularly during repetitive motions. Weak quadriceps or tight hamstrings may also redistribute stress unevenly across joint surfaces.
How Squatting Affects the Joint
Descending into a squat multiplies forces through the lower body. Research shows kneecap pressure increases sevenfold during deep flexion. Proper form engages glutes and core muscles to share the load, while poor technique overloads connective tissues.
Muscle imbalances frequently contribute to instability. When hip stabilizers weaken, the knees compensate by rotating inward under strain. This misalignment accelerates cartilage wear and may also trigger tendon inflammation over time, particularly in cases of existing patellar tendonitis.
Causes and Symptoms of Knee Pain During Squats
Joint discomfort during lower-body movements often signals underlying mechanical issues. Three primary culprits dominate clinical observations: repetitive strain, structural deterioration, and inflammatory responses. Let’s examine how these factors manifest during weighted or deep bending motions.
Common Knee Injuries and Conditions
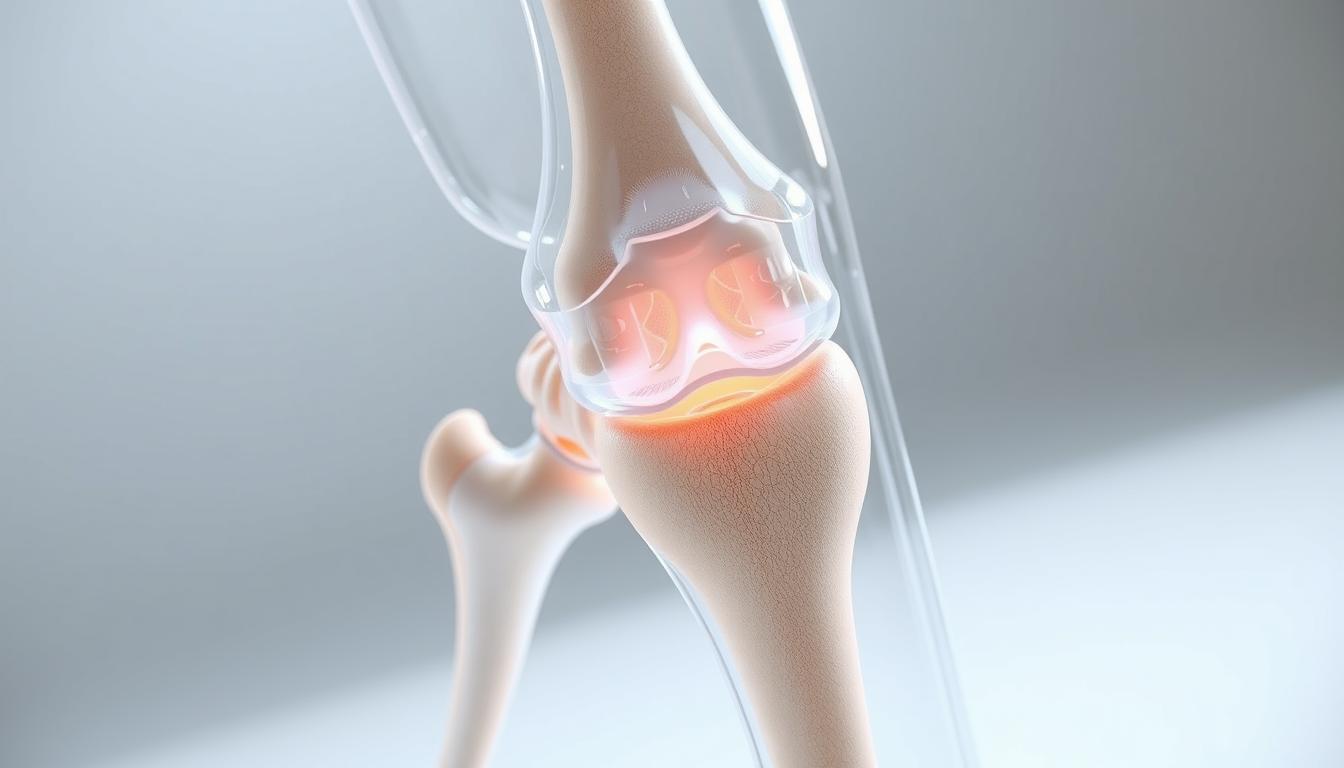
Patellofemoral syndrome tops the list, causing grinding sensations beneath the kneecap. Meniscus tears create sharp stabbing feelings, often accompanied by audible pops. Osteoarthritis gradually erodes protective cartilage, making joint surfaces rub painfully during squats.
Tendonitis frequently develops near the patellar tendon, particularly with excessive jumping or abrupt stops. Research shows improper squat depth increases pressure on tendons by 52% compared to controlled partial bends. Over months, this strain can trigger chronic inflammation.
Recognizing Early Warning Signs
Swelling around the joint capsule often precedes severe damage. Many notice increased stiffness after prolonged sitting or morning wake-ups. Dull throbbing following exercises suggests microtears requiring rest.
Listen to your body’s alerts. Clicking noises during movement or sudden weakness when standing signal potential ligament issues. Persistent warmth around the kneecap indicates active inflammation needing attention.
While targeted strengthening exercises can alleviate mild cases, worsening symptoms demand professional evaluation. Early intervention prevents minor irritations from becoming career-ending injuries.
Why does my knee hurt when I squat down: A Closer Look
The mechanics behind squat-related discomfort often trace back to repetitive strain patterns. Two primary injuries dominate clinical findings among active individuals – patellar tendonitis and runner’s knee. Both conditions thrive on overuse, though their causes and manifestations differ significantly.
Patellar Tendonitis and Runner’s Knee
Patellar tendonitis creates inflammation along the rope-like structure connecting kneecap to shinbone. Repeated jumping or abrupt stops strain this critical stabilizer. Runner’s knee (patellofemoral pain syndrome) involves cartilage irritation beneath the kneecap, often worsening during stair climbing or prolonged sitting.
| Condition | Primary Cause | Key Symptom |
|---|---|---|
| Patellar Tendonitis | Repetitive jumping motions | Localized pain below kneecap |
| Runner’s Knee | Poor kneecap alignment | Dull ache around kneecap edges |
| Both Conditions | Muscle imbalances | Increased discomfort during flexion |
Additional Contributing Factors
Excess weight multiplies joint stress during daily activities like lifting or bending. Studies show every pound of body mass generates four pounds of pressure on knees during squats. Tight iliotibial bands or weak hip abductors further disrupt movement mechanics.
Recognizing early symptoms – swelling, creaking sounds, or persistent warmth – helps prevent chronic damage. While targeted exercises address muscular causes, lasting relief requires addressing biomechanical roots through professional evaluation.
Diagnosis and Medical Evaluation
Persistent joint issues demand precise investigation. Healthcare providers use multi-step evaluations to separate temporary strains from chronic conditions. This systematic approach identifies both immediate triggers and hidden contributors to discomfort.

Assessing Your Symptoms and History
Doctors first evaluate activity patterns that might accelerate joint wear. They’ll ask about exercise routines, occupational demands, and recreational habits. Previous injuries often resurface as secondary causes of current discomfort.
Physical exams include compression tests to locate tender areas. Clinicians check for fluid buildup and restricted motion ranges. They observe how stiffness changes during movement compared to rest periods.
Imaging tools like X-rays reveal bone alignment and cartilage gaps. These scans help rule out fractures or arthritis. For soft tissue assessment, MRI scans might be ordered if ligament damage is suspected.
A complete history review connects dots between past traumas and present symptoms. This process helps differentiate new injuries from recurring conditions. Accurate diagnosis guides effective treatment plans tailored to each individual’s needs.
Professional evaluations often uncover surprising links. A misaligned pelvis or weak core muscles might contribute to joint stress during activity. Addressing these root causes prevents symptom recurrence after initial recovery.
Treatment Options and Home Remedies
Effective management of joint discomfort begins with immediate action. Early interventions can reduce recovery time and prevent chronic issues from developing. Let’s explore proven strategies that combine self-care techniques with professional guidance.
R.I.C.E. Method and At-Home Care
The R.I.C.E. protocol remains a gold standard for acute injuries. Follow these steps within 48 hours of symptom onset:
- Rest: Pause activities causing pain – continued strain delays healing
- Ice: Apply cold packs for 15-minute intervals to reduce swelling
- Compression: Use elastic bandages to stabilize the joint
- Elevation: Keep legs raised above heart level when resting
Controlled movement becomes crucial after initial inflammation subsides. Gentle range-of-motion exercises maintain circulation without overloading tissues. For arthritis sufferers, low-impact activities like swimming preserve joint function.
Medication, Massage, and Physical Therapy
Over-the-counter NSAIDs temporarily relieve pain and swelling. Always follow dosage instructions – prolonged use risks stomach irritation. Therapeutic massage improves blood flow to stiff muscles surrounding joints.
| Treatment | Benefits | Frequency |
|---|---|---|
| Ice Therapy | Reduces inflammation | 3-5x daily |
| Physical Therapy | Strengthens support muscles | 2-3x weekly |
| Topical Creams | Targets localized pain | As needed |
Persistent conditions require customized rehabilitation plans. Physical therapists design exercise programs addressing muscle imbalances and movement patterns. If symptoms persist beyond two weeks, consult a specialist to rule out structural damage.
Prevention Strategies and Exercise Modifications
Movement quality determines joint longevity. Strategic adjustments to daily motions and training routines can dramatically reduce strain on vulnerable areas. Let’s explore techniques that protect the knee joint while maintaining functional strength.
Mastering Movement Mechanics
Proper alignment during bending activities distributes forces evenly. Keep your chest upright and feet aligned with hips. Push through heels rather than toes to engage glutes effectively. This reduces pressure on the front knee joint by 37% according to biomechanical studies.
Three critical form checkpoints:
- Maintain neutral spine position
- Control descent speed (2-3 seconds)
- Stop at pain-free depth
Building Resilient Support Systems
Targeted exercises address common causes knee pain develops from. Focus on strengthening quadriceps and hip abductors while stretching tight hamstrings. For those with iliotibial band syndrome, lateral leg raises and foam rolling improve tissue mobility.
| Exercise | Benefit | Frequency |
|---|---|---|
| Step-Ups | Enhances single-leg stability | 3x weekly |
| Clamshells | Strengthens hip rotators | Daily |
| Calf Stretches | Reduces tendon tension | Post-workout |
Gradual progression prevents overload. Increase workout intensity by no more than 10% weekly. Supportive braces or orthotics help correct alignment issues during the strengthening phase. These methods collectively prevent knee pain recurrence while building durable movement patterns.
Managing Knee Pain in Daily Activities
Active lifestyles demand smart adaptations to preserve mobility without sacrificing performance. Strategic modifications to movement patterns and exercise routines help maintain joint integrity while addressing common discomfort triggers.
Adjusting Workouts and Lifestyle Changes
Proper technique remains the foundation of joint protection. Focus on these three form corrections during lower-body movements:
- Align hips over ankles during squats to reduce front knee pressure
- Engage core muscles before lifting to prevent knee instability
- Maintain 90-degree ankle flexion to avoid improper form
Footwear choices significantly impact joint stress. Opt for shoes with arch support and shock absorption, particularly if managing runner knee or band syndrome. Orthopedic inserts can further correct alignment issues that cause knee strain.
| High-Impact | Low-Impact Alternative | Benefit |
|---|---|---|
| Running | Elliptical training | Reduces joint compression |
| Jump squats | Wall sits | Builds quad strength safely |
| Basketball | Cycling | Maintains cardio without pounding |
Gradual progression proves essential when reintroducing activities. Start with 20-minute sessions of swimming or yoga, increasing duration by 10% weekly. Listen for warning signs like runner knee tenderness or band syndrome tightness along the outer thigh.
Preventive measures work best when combined. Use compression sleeves during demanding workouts and ice packs after intense sessions. These simple adjustments help prevent knee issues from derailing fitness goals while addressing root cause knee stressors.
Conclusion
Maintaining joint health demands equal parts awareness and action. Through this guide, we’ve explored how movement mechanics, muscle balance, and conditions like iliotibial band syndrome influence discomfort during bending motions. Early intervention remains critical – temporary fixes often mask deeper issues requiring professional assessment.
Proper form during daily activities reduces strain on vulnerable tissues. Simple adjustments like controlled squat depth and strategic exercise modifications protect joints long-term. For those managing recurring stiffness, targeted strengthening routines address imbalances that contribute to flare-ups.
Persistent symptoms signal the need for expert evaluation. Imaging tests and physical exams uncover hidden contributors, from cartilage wear to iliotibial band tightness. Pair clinical guidance with our prevention strategies – compression gear, low-impact alternatives, and gradual training progressions – to sustain mobility.
Share these insights with others facing similar challenges. For personalized solutions, consult a sports medicine specialist or physical therapist. Together, we can transform how communities approach joint care – one smart movement at a time.
FAQ
What causes discomfort during squats?
Discomfort often stems from repetitive stress, improper form, or underlying conditions like patellar tendonitis or iliotibial band syndrome. Weak muscles, poor alignment, or cartilage wear can increase joint pressure, leading to inflammation.
How do I differentiate tendonitis from arthritis?
Patellar tendonitis typically causes sharp pain below the kneecap during activity, while arthritis involves stiffness, swelling, and dull aches worsened by prolonged rest. Imaging tests or a physical exam by an orthopedist can confirm the diagnosis.
Can squatting worsen existing injuries?
Yes. Movements like deep squats or heavy loading strain ligaments and tendons. Conditions like runner’s knee or meniscus tears may flare up without proper modifications. We recommend reducing range of motion or using resistance bands temporarily.
What exercises reduce strain on the joint?
Focus on low-impact activities like swimming or cycling. Strengthen quadriceps and hamstrings with leg raises or wall sits. Stretch the iliotibial band and calves to improve flexibility and reduce compression during squats.
When should I consult a doctor?
Seek medical advice if pain persists beyond two weeks, swelling limits mobility, or clicking/popping occurs. Sudden instability or inability to bear weight may indicate ligament damage requiring urgent care.
Are braces effective for managing symptoms?
Supportive braces or patellar straps can redistribute pressure during activity. However, they’re not a long-term fix. Pair them with physical therapy to address muscle imbalances and improve biomechanics.
How does footwear impact squat-related pain?
Shoes with poor arch support or excessive cushioning alter alignment, increasing knee stress. Opt for flat-soled shoes or weightlifting footwear to stabilize the foot and reduce joint torsion.
Can weight loss alleviate symptoms?
Excess body weight heightens compressive forces on cartilage. Losing even 5–10 pounds through diet and low-impact cardio can significantly reduce discomfort during daily activities or workouts.