Are you tired of the strain traditional ladders put on your knees? Working at heights shouldn’t have to come at the cost of knee discomfort or long-term damage. We’re exploring the world of ergonomic solutions designed to make a difference in our daily lives, whether we’re DIY enthusiasts or professionals.
As we continue to work at heights, it’s essential to consider ergonomic ladder options that prioritize our knee health. By choosing the right equipment, we can significantly reduce the risk of knee injuries and improve our overall well-being.
Key Takeaways
- Ergonomic solutions can reduce knee strain when working at heights.
- Choosing the right equipment is crucial for knee health.
- There are various knee-friendly options available for DIY enthusiasts and professionals.
- Prioritizing knee health can improve overall well-being.
- Long-term damage can be prevented with the right ladder alternatives.
Understanding the Need for Knee-Friendly Options

When we try to get things done quickly, we often forget about the harm ladders can do to our knees. As we get older or use ladders a lot, this harm can get worse. It can cause pain or even hurt our knees.
It’s important to know how ladders affect our knee health. This helps us make better choices about our workspaces and tools.
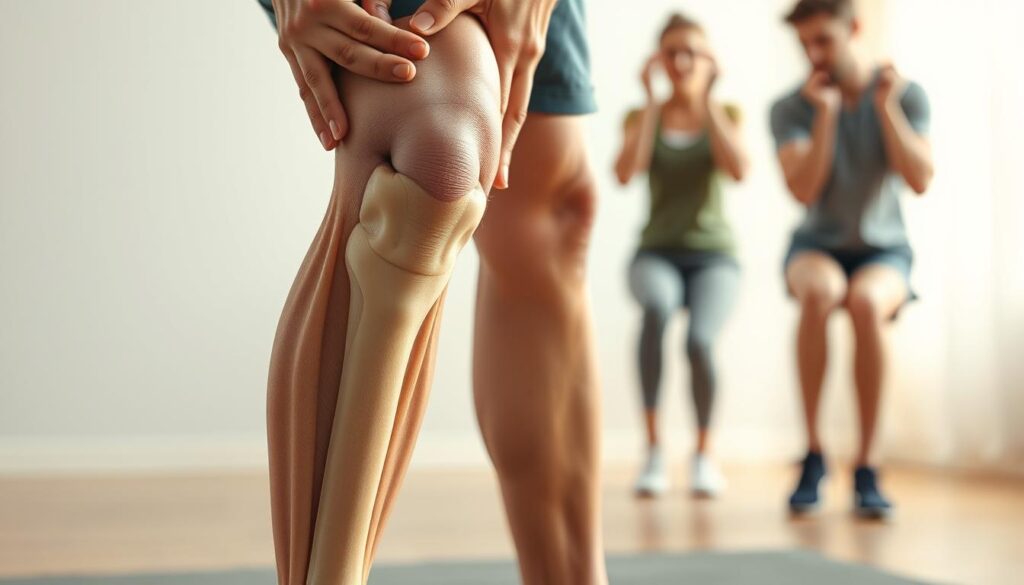
The Impact of Traditional Ladders on Knee Health
Traditional ladders make us climb, bend, and sometimes get into awkward positions. This can hurt our knees a lot. Climbing ladders over and over can make knee problems worse or even cause new ones.
The key areas of concern include:
- The strain from climbing up and down
- The pressure on the knee joint from bending
- The potential for accidents due to ladder instability
| Potential Risks | Impact on Knee Health |
|---|---|
| Climbing and Descending | Strain on knee ligaments and joints |
| Bending and Stretching | Pressure on the knee cap and surrounding muscles |
| Ladder Instability | Risk of falls and acute knee injuries |
“The design of traditional ladders often overlooks the ergonomic needs of the user, leading to potential long-term health issues.”
Benefits of Choosing Knee-Friendly Alternatives
Choosing knee-friendly ladders can really help our knees. These ladders are made to be easy on our joints. They make it safer and more comfortable to do tasks at heights.
The benefits include:
- Reduced strain on the knee joint
- Improved stability and safety
- Enhanced comfort during use
By choosing ergonomic ladder options and joint-friendly climbing solutions, we can keep our knees safe. We can still be productive too.
Popular Knee-Friendly Ladder Alternatives

Looking for safer ways to reach high shelves or change light bulbs has led to new options. These alternatives are easier on our knees and offer convenience in many places.
Step Stools: A Simple Solution for Low Heights
Step stools are great for tasks that don’t need you to go very high. They’re perfect for indoor use, like in kitchens, libraries, or offices. They help you get to items just out of reach.
One big plus of step stools is their compact design. This makes them easy to store in tight spots. They’re also light, so you can move them around easily.
Platform Lifts: For Elevated Access with Comfort
Platform lifts are a good choice for higher access needs. They offer a big platform for standing while working at heights.
They’re great in industrial or commercial settings where workers often need to go up high. They come with safety features like guardrails to prevent falls.
| Feature | Step Stools | Platform Lifts | Folding Ladders |
|---|---|---|---|
| Height Access | Low to Moderate | High | Moderate to High |
| Space Requirement | Compact | Large | Compact when folded |
| Safety Features | Non-slip steps | Guardrails, Non-slip surface | Non-slip steps, Stabilizing bars |
Folding Ladders: Space-Saving and Functional
Folding ladders are a top pick for those looking for knee-friendly options. They’re space-efficient and easy to store when not in use.
These ladders are versatile and work well in many settings. They’re great for both household tasks and professional jobs. Their design makes them easy to carry and store.
Exploring these knee-friendly ladder alternatives can greatly lower the risk of knee injuries. Whether you need a step stool for low heights, a platform lift for higher access, or a folding ladder for versatility, there’s a safe choice for you.
Comparing Knee-Friendly Options to Traditional Ladders

When it comes to ladder safety, it’s important to compare traditional ladders with knee-friendly options. We’ll look at weight capacity, stability, ease of use, and safety features.
Weight Capacity and Stability Concerns
Choosing the right ladder is key. Traditional ladders are often sturdy but can be unstable on uneven ground. Knee-friendly ladders, like platform lifts, have a wide base for better stability.
Here’s a table comparing traditional ladders with knee-friendly alternatives:
| Ladder Type | Weight Capacity | Stability Features |
|---|---|---|
| Traditional Ladder | Up to 300 lbs | Non-slip feet, narrow base |
| Step Stool | Up to 250 lbs | Wide base, non-slip steps |
| Platform Lift | Up to 500 lbs | Wide, stable platform, guardrails |
Ease of Use: Setup and Maneuverability
Choosing a ladder that’s easy to use is important. Traditional ladders can be hard to set up. Knee-friendly ladders, like folding ladders, are lightweight and easy to carry.
When looking at ease of use, think about setup, weight, and how easy it is to move. Knee-friendly ladders often win in these areas, making them easier to use.
Safety Features to Consider
Safety is a top priority when picking a ladder. Traditional ladders might not have the safety features that knee-friendly ladders do. For example, knee-friendly ladders often have non-slip surfaces, guardrails, and secure locks.
Here’s a list of safety features to look for:
- Non-slip surfaces: Helps prevent slipping off.
- Guardrails: Adds extra support and protection.
- Secure locking mechanisms: Keeps the ladder stable and secure.
By considering these safety features, you can make a better choice between traditional ladders and knee-friendly alternatives.
How to Choose the Right Knee-Friendly Ladder Alternative
Choosing the right knee-friendly ladder alternative needs careful thought. It’s not just about picking the first one you see. You must think about what you need and what you prefer.
Assessing Your Specific Needs and Space
First, think about what you need and where you’ll use the ladder. Consider how high you need to go and where you’ll store the ladder. Measure the area where you’ll use it to make sure it fits right.
If you work in small spaces, a folding ladder is a good choice. It saves space. But if you often need to reach high places, a platform lift is better. It’s comfortable and stable.
Material Considerations: Aluminum vs. Wood
The ladder’s material is key. Aluminum ladders are light and don’t rust, making them popular. Wooden ladders are heavier but last longer and look traditional.
| Material | Weight | Durability | Aesthetic Appeal |
|---|---|---|---|
| Aluminum | Lightweight | High | Modern |
| Wood | Heavy | High | Traditional |
Budgeting for Quality vs. Cost
When setting a budget for a ladder, balance quality and cost. Cheap ladders might look good but may not last or be safe. Spending more on a quality ladder can save money in the long run and keep you safe.
Think about your budget and what you need. Prioritize ladders that offer good value. This way, you get what you need without spending too much.
Maintenance Tips for Knee-Friendly Alternatives
Keeping your knee-friendly ladder alternative in good shape is key for safety and longevity. By following a few simple steps, you can make sure your ergonomic ladder options stay safe and reliable.
Regular Inspection for Safety and Durability
Regular checks are vital to spot any issues with your ladder. Look for signs of wear and tear, like loose rungs or damaged feet. Also, make sure all moving parts work right.
- Inspect the ladder’s rungs and rails for any signs of damage or wear.
- Check that all locking mechanisms are secure and functioning properly.
- Ensure that the ladder’s feet are in good condition and not slippery.
Cleaning and Care for Longevity
Proper cleaning and care can make your ergonomic ladder options last longer. Clean your ladder often to remove dirt and grime that could harm it.
- Use a mild detergent and water to clean the ladder’s surfaces.
- Avoid using harsh chemicals or abrasive materials that could damage the ladder’s finish.
- Dry the ladder thoroughly after cleaning to prevent water spots and corrosion.
By following these maintenance tips, you can keep your knee-friendly ladder alternative safe and reliable for years.
User Experiences: Real Stories from Safer Alternatives
Many people have moved to knee-friendly ladders, sharing their success stories. They talk about better safety and comfort. These stories show the real benefits of safer ladders.
Case Studies: Transitioning from Traditional to Knee-Friendly
Case studies show the good effects of switching to knee-friendly ladders. A contractor said using platform lifts eased his knee pain during long hours. This change boosted his comfort and work speed.
A homeowner also shared her story. She replaced old ladders with step stools for household tasks. She felt less knee pain and more confident while working at heights.
Success Stories from DIY Enthusiasts and Professionals
DIY fans and pros alike have seen the ladder benefits. A DIYer found folding ladders easier for tight spaces, lowering knee injury risks.
A painter praised the stability and comfort of knee-friendly ladders. He said they made his work more efficient and reduced fatigue. These stories highlight the importance of joint-friendly climbing solutions.
These tales prove switching to safe ladder choices for knees improves health and work efficiency. Whether you’re a pro or a DIYer, the right ladder can greatly impact your work.
Future Trends in Knee-Friendly Access Solutions
The future of knee-friendly access solutions is exciting. We’re seeing more low-impact ladder substitutes that focus on comfort and knee health. These ladders are designed to reduce strain and make work safer.
Advancements in Design
New knee-conscious ladder alternatives are being made with advanced materials and ergonomic designs. These ladders are changing how we access high places, making it easier to work without harming our knees.
Market Growth and Accessibility
The need for knee-friendly ladders is growing, leading to more options in the market. As companies meet these needs, we’ll see even more creative solutions. This will help make our workspaces safer and more welcoming for everyone.
FAQ
What are knee-friendly ladder alternatives?
Knee-friendly ladder alternatives are made to ease the pressure on our knees. They offer a safer and more comfortable way to reach high places. Examples include step stools, platform lifts, and folding ladders.
How do traditional ladders impact knee health?
Traditional ladders can harm our knees. Climbing up and down puts strain and pressure on them. This can cause pain and even long-term damage.
What are the benefits of using knee-friendly ladder alternatives?
Using knee-friendly ladder alternatives can reduce knee strain and improve comfort. They also make working at heights safer. Plus, they’re convenient and versatile for many tasks.
How do I choose the right knee-friendly ladder alternative?
To pick the right ladder, think about your needs, space, material preferences, and budget. This will help you find a ladder that’s both comfortable and meets your needs.
What are some popular knee-friendly ladder alternatives?
Popular options include step stools, platform lifts, and folding ladders. They offer benefits like saving space and providing comfortable access.
How do I maintain my knee-friendly ladder alternative?
Keeping your ladder in good shape is key. Regularly check it, clean it, and follow care tips to make it last longer.
Are knee-friendly ladder alternatives stable and secure?
Yes, they are designed to be stable and secure. Look for ladders with a high weight capacity, good stability, and safety features.
Can knee-friendly ladder alternatives be used for heavy-duty tasks?
Yes, many are made for heavy-duty tasks. Choose ones with high weight capacities and strong construction to meet your needs.
What are some innovative features in knee-friendly ladder alternatives?
They often have ergonomic designs, advanced materials, and smart storage solutions. These features improve comfort, convenience, and safety.
How do knee-friendly ladder alternatives impact productivity?
They can boost productivity by reducing fatigue and discomfort. They make working at heights more comfortable and safe, helping you work better and faster.