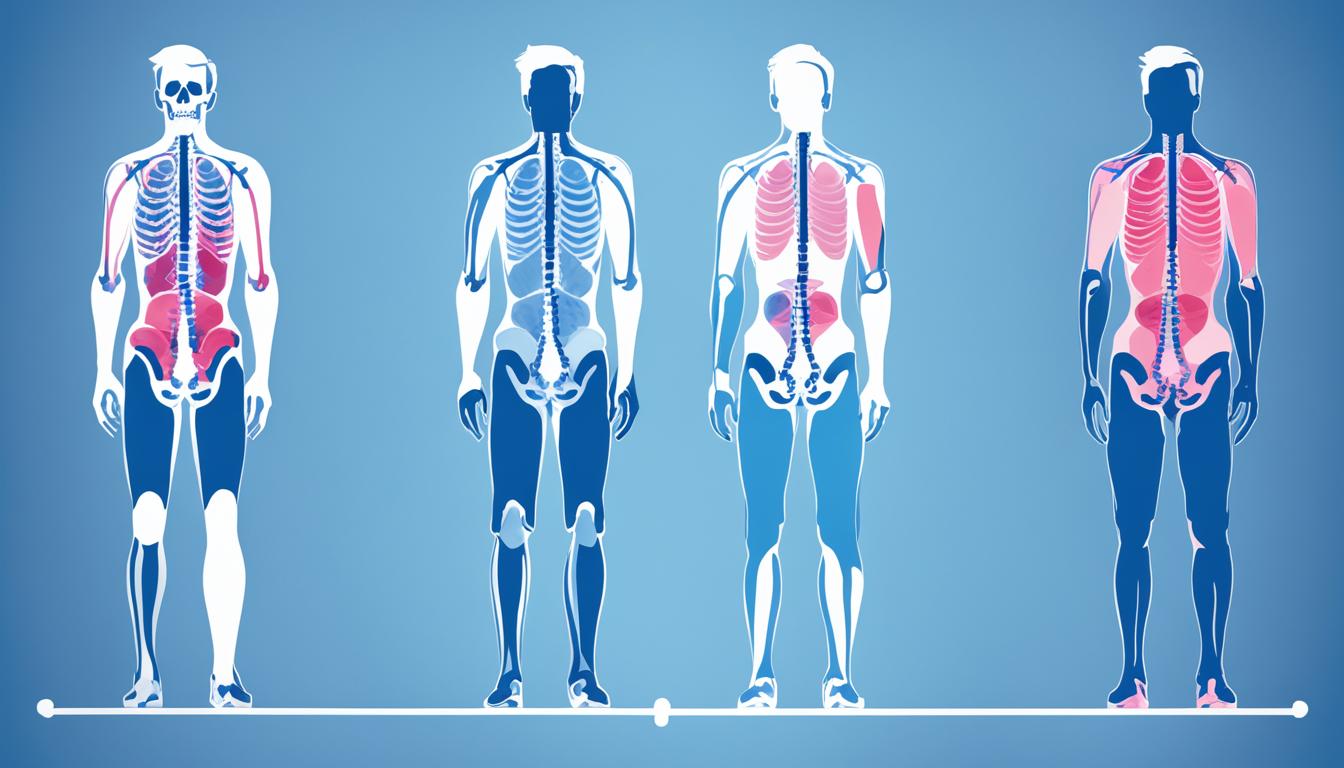
Osteoarthritis, the most common form of arthritis, affects millions of people worldwide. This degenerative joint disease can lead to pain, stiffness, and decreased mobility. While osteoarthritis can affect any joint in the body, there are certain common sites for osteoarthritis that are more frequently affected.
In this article, we will explore the prevalence of osteoarthritis and identify the locations with high rates of this condition. Understanding the distribution of osteoarthritis can provide valuable insight into its impact on individuals and communities.
Osteoarthritis in the Hands
Osteoarthritis is a degenerative joint disease that commonly affects the hands. The joints in the hands can become inflamed, leading to pain, stiffness, and swelling. Individuals with osteoarthritis in their hands often experience difficulty grasping objects due to changes in the finger joints. These joints may become enlarged and tender, causing discomfort and hindering everyday tasks.
One particular joint commonly affected by osteoarthritis in the hands is the joint at the base of the thumb. This joint, known as the basal joint or carpometacarpal joint, is crucial for thumb mobility and function. When osteoarthritis occurs in this joint, individuals may experience pain, limited mobility, and difficulty performing simple movements like pinching or gripping.
Osteoarthritis in the hands can have a significant impact on an individual’s quality of life, as it can affect their ability to perform everyday tasks and activities. Simple actions like buttoning a shirt or opening a jar can become challenging and painful. It is essential for those experiencing symptoms of osteoarthritis in their hands to seek medical attention to manage their condition effectively.

| Signs and Symptoms of Osteoarthritis in the Hands | Treatment Options |
|---|---|
|
|
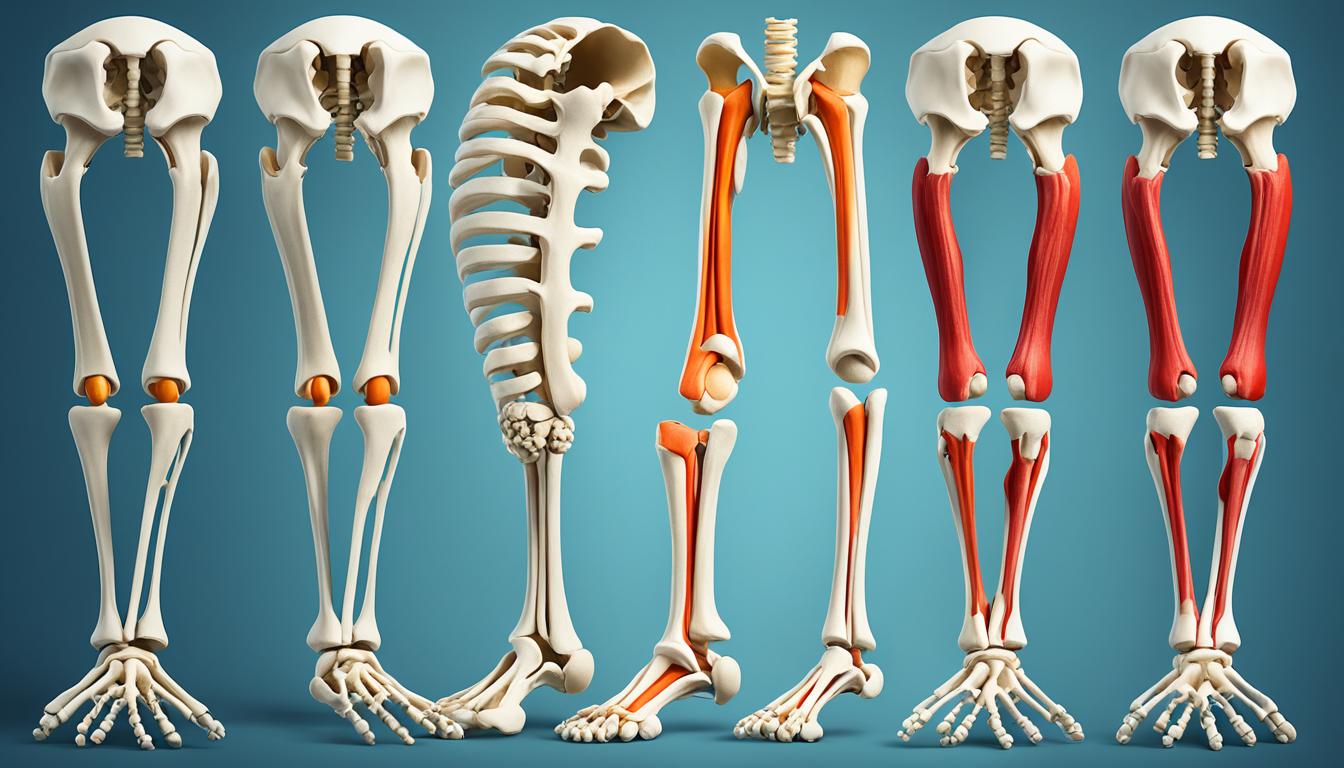
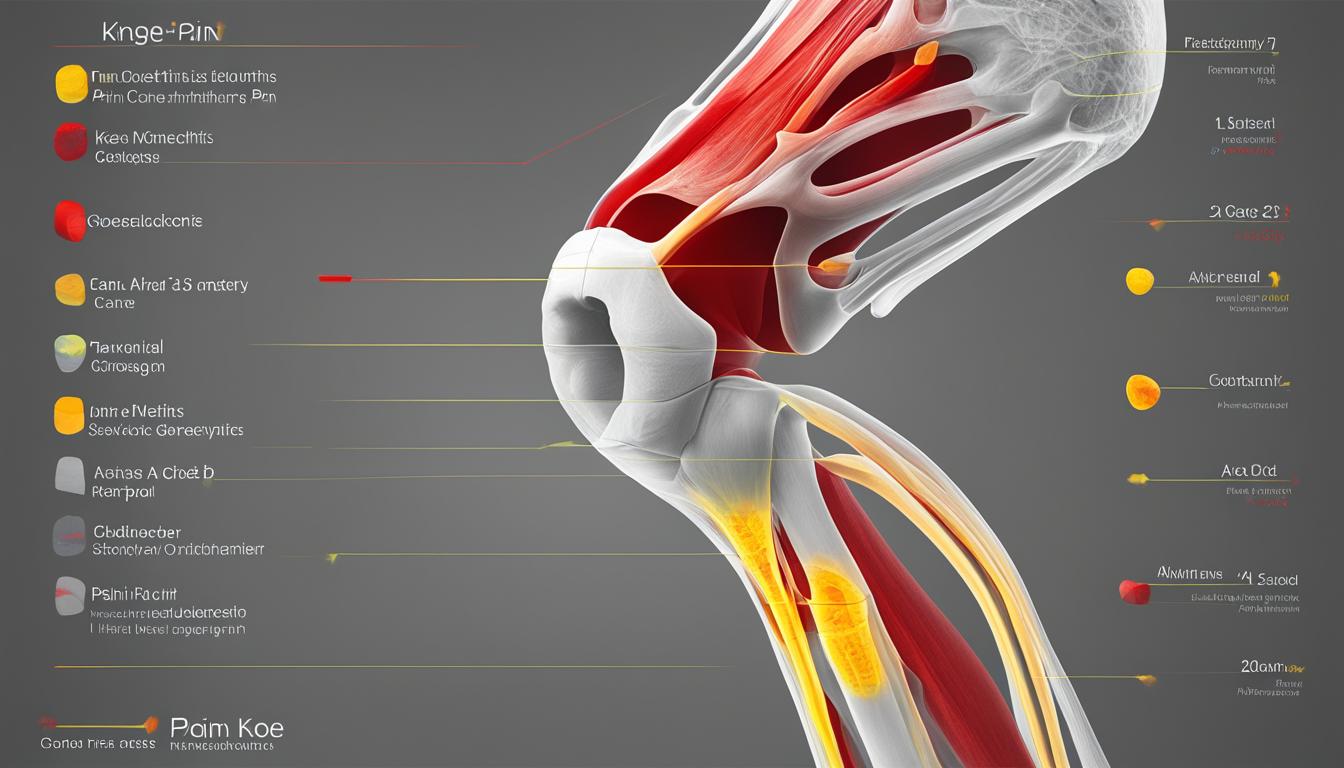
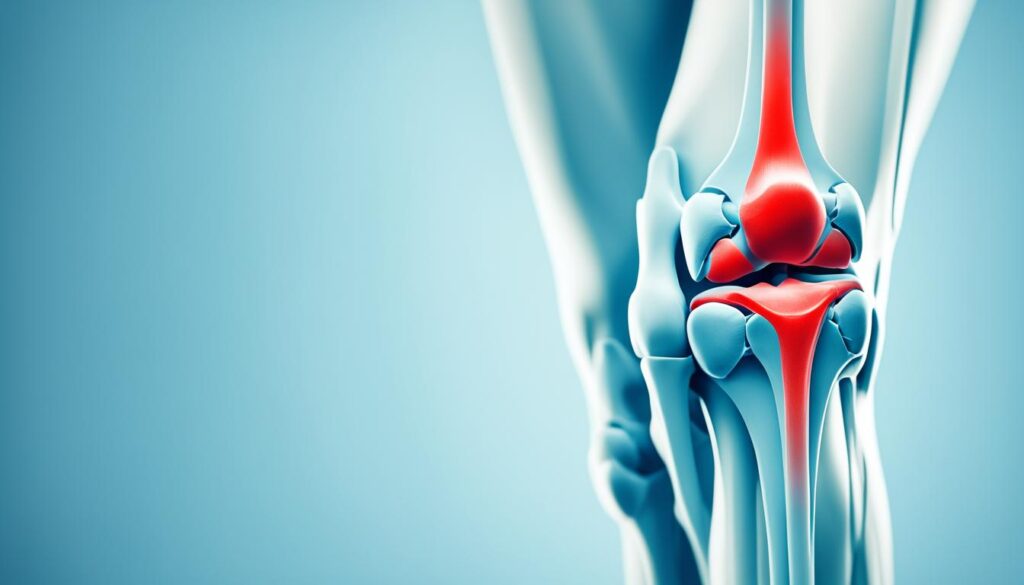
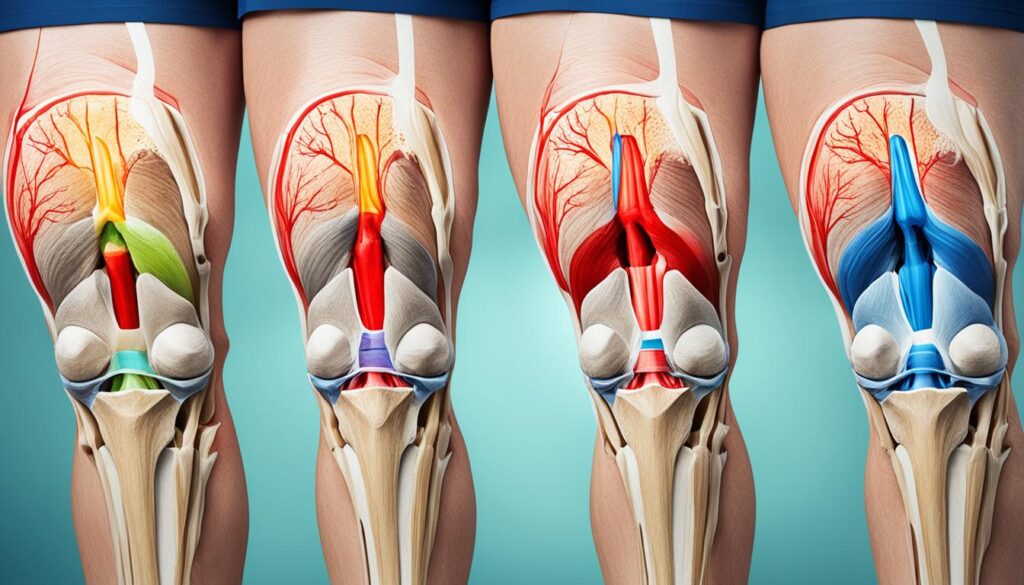
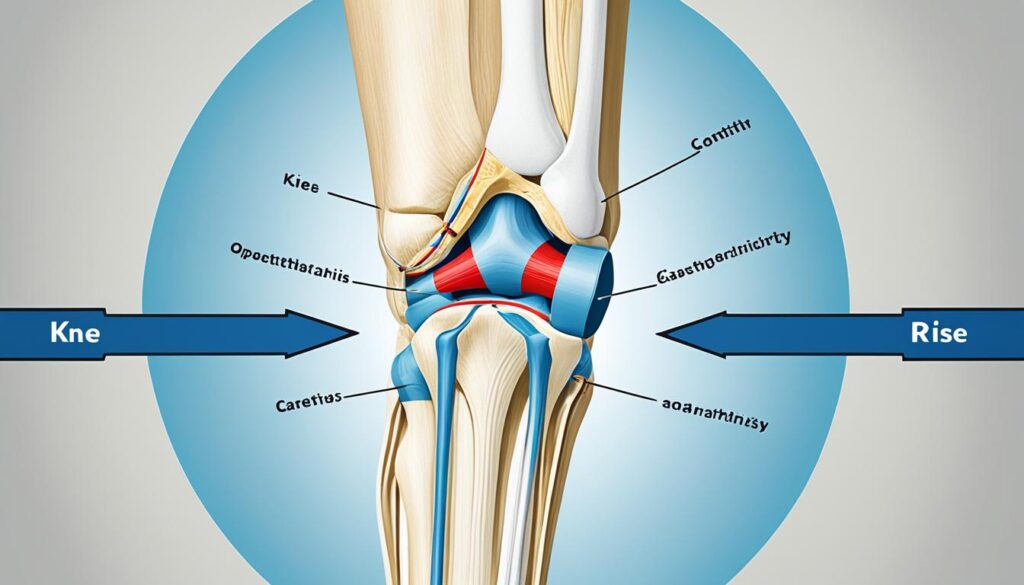
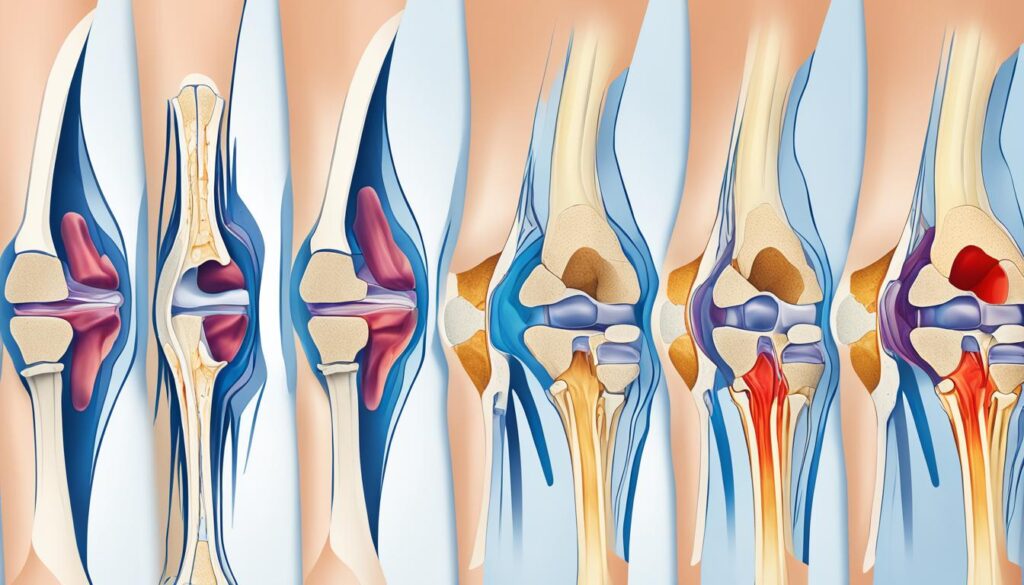
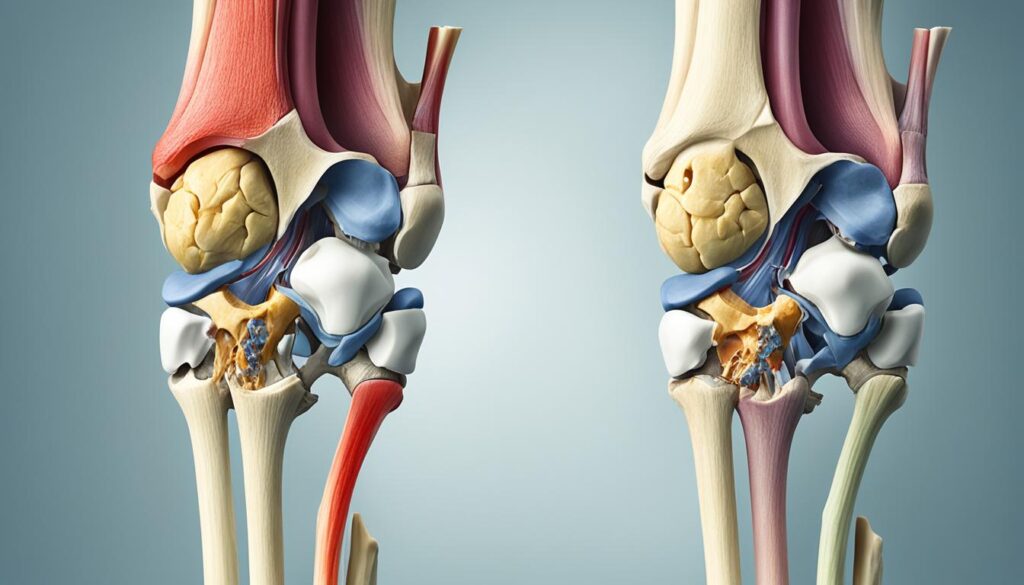
Osteoarthritis in the Knees
The knees are another common site for osteoarthritis. The knee joint, which is essential for mobility and weight-bearing, is particularly vulnerable to the effects of osteoarthritis. When cartilage in the knee joint wears down, it can lead to various symptoms and difficulties in daily activities.
Pain is a common symptom of osteoarthritis in the knees, which can range from mild discomfort to severe pain. The pain is often felt in and around the knee joint and may worsen with movement or prolonged activity. Stiffness is another prevalent symptom, making it challenging to bend or straighten the knee fully.
Individuals with knee osteoarthritis may also experience difficulty with walking or climbing stairs. The weakened cartilage and joint structures may limit mobility and affect balance. Instability or weakness in the knee joint can further hinder activities, making it challenging to engage in exercises or perform daily tasks that require knee movement.
To provide a visual representation of the impact of osteoarthritis in the knees, refer to the table below illustrating the common symptoms experienced by individuals with knee osteoarthritis:
| Symptoms of Knee Osteoarthritis |
|---|
| Pain in and around the knee joint |
| Stiffness and limited range of motion |
| Difficulty with walking or climbing stairs |
| Weakness or instability in the knee |
It is important to address knee osteoarthritis promptly to minimize its impact on daily life. Treatment options for knee osteoarthritis include lifestyle modifications, physical therapy, medication, and in severe cases, surgical interventions.
By understanding the effects of osteoarthritis in the knees and recognizing the associated symptoms, individuals can work towards managing the condition effectively and improving quality of life.
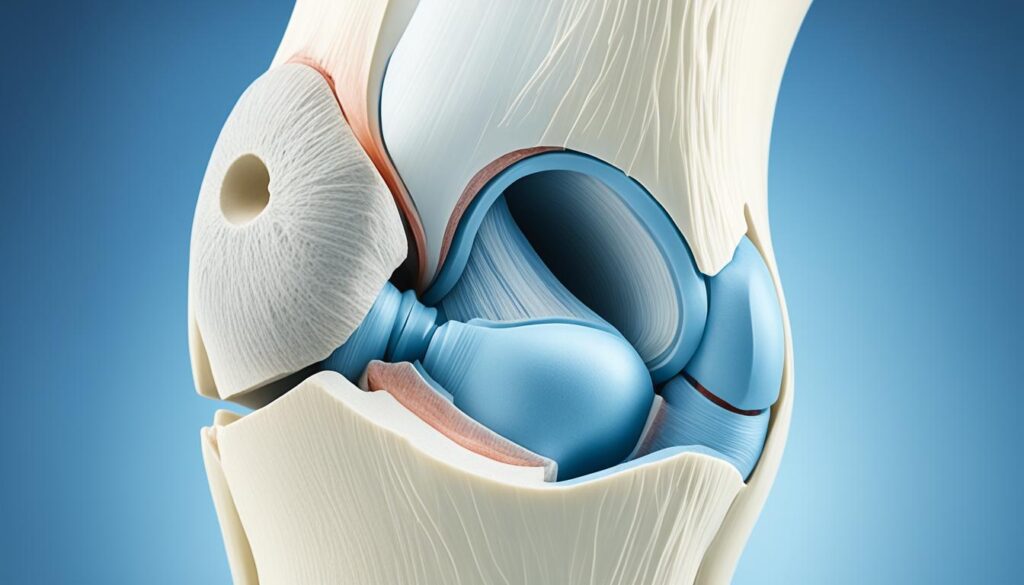
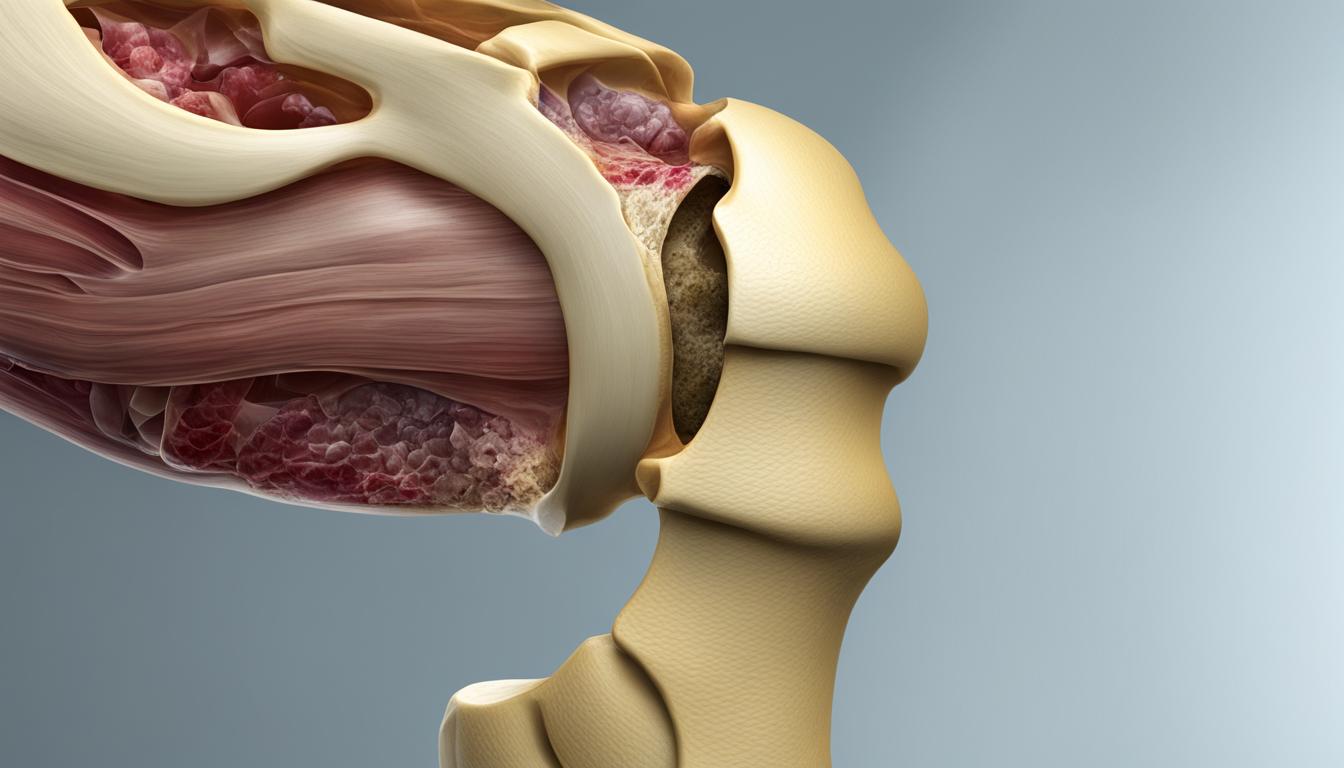
Osteoarthritis in the Hips
Osteoarthritis can have a significant impact on the hip joint, causing discomfort and limitations in daily activities. The hip joint, also known as the “ball and socket” joint, is particularly susceptible to osteoarthritis. This condition occurs when the protective cartilage that cushions the joint wears down over time.
The main symptom of osteoarthritis in the hips is pain that may radiate to the groin, buttocks, or knee. Activities like walking or standing for a prolonged period can exacerbate the pain and discomfort. Stiffness, reduced range of motion, and difficulty in performing simple movements like bending or straightening the hip can also be experienced.
Left untreated, hip osteoarthritis can significantly affect a person’s quality of life, limiting their mobility and independence. Therefore, it is crucial to seek appropriate medical attention and explore various treatment options.
Treatment Options for Osteoarthritis in the Hips
When it comes to managing osteoarthritis in the hips, there are various treatment options available, depending on the severity of the condition and the individual’s specific needs. These treatment options may include:
- Physical therapy: Gentle exercises and stretches can help improve hip joint function, maintain flexibility, and decrease pain.
- Medications: Over-the-counter pain relievers or prescription medications may be recommended to manage pain and reduce inflammation.
- Assistive devices: Using walking aids like canes or walkers can help alleviate pressure on the hip joint and improve mobility.
- Injections: Corticosteroid injections or hyaluronic acid injections directly into the hip joint can provide temporary pain relief.
In severe cases, when conservative treatments fail to provide adequate relief, surgical interventions such as hip replacement surgery may be considered.
| Treatment Options | Description |
|---|---|
| Physical Therapy | Gentle exercises and stretches to improve hip joint function and reduce pain. |
| Medications | Over-the-counter or prescription medications to manage pain and inflammation. |
| Assistive Devices | Walking aids like canes or walkers to alleviate pressure on the hip joint and improve mobility. |
| Injections | Corticosteroid or hyaluronic acid injections for temporary pain relief. |
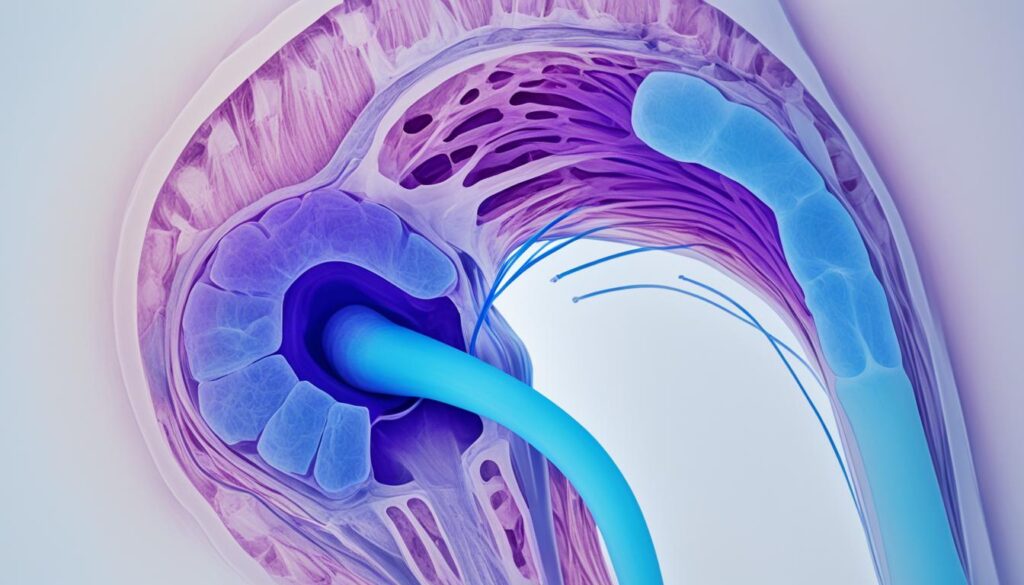
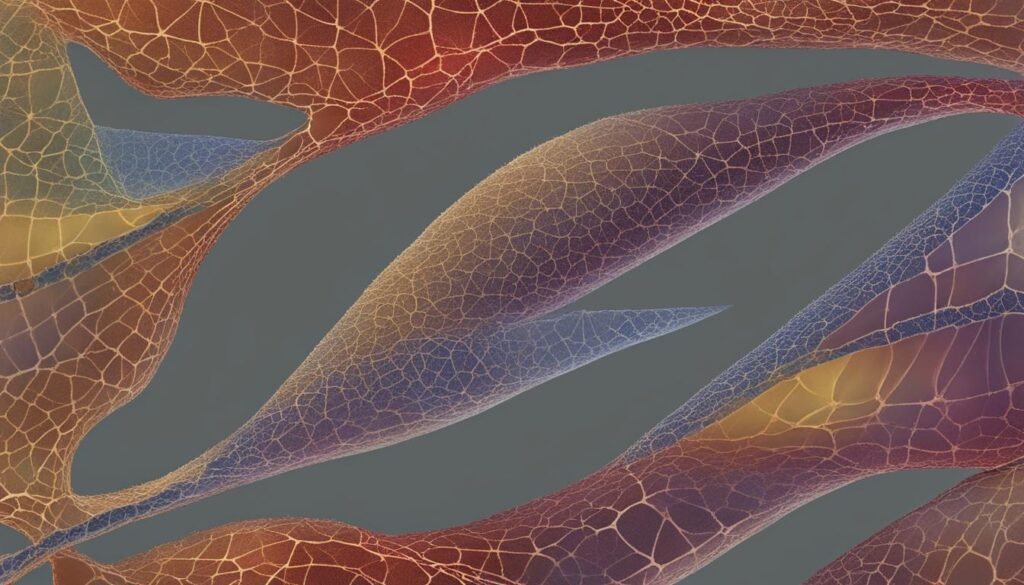
Osteoarthritis in the Spine
When it comes to osteoarthritis, the spine is not exempt from its effects. This degenerative joint disease can take a toll on the intricate network of bones that make up our spinal column. Osteoarthritis in the spine, also known as spondylosis or spinal osteoarthritis, can cause significant pain and discomfort, impacting one’s overall quality of life.
One common manifestation of osteoarthritis in the spine is the narrowing of the disks between the vertebrae. These intervertebral disks act as cushions and shock absorbers, but with osteoarthritis, they may start to deteriorate. As a result, individuals may experience pain, stiffness, and a decreased range of motion in the affected areas.
The formation of bone spurs is another hallmark of osteoarthritis in the spine. These bony outgrowths can develop around the edges of the vertebrae, contributing to the compression of nerves and leading to additional discomfort and mobility issues.
The neck (cervical spine) and the lower back (lumbar spine) are the two most commonly affected areas by osteoarthritis in the spine. In the neck, osteoarthritis can cause neck pain, headaches, and even radiculopathy, which is the compression or irritation of nerves leading to radiating pain, numbness, or weakness in the arms. In the lower back, individuals may experience lower back pain, limited flexibility, and difficulty performing everyday activities.
Osteoarthritis in the spine requires proper management and treatment to alleviate symptoms and maintain overall spinal health. Physical therapy, pain management techniques, medication, and lifestyle modifications can all play a role in improving mobility and reducing discomfort. In severe cases, surgical intervention may be necessary to address specific spinal issues.
It’s important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan if you suspect osteoarthritis in the spine. They can provide guidance and support to help you manage your condition effectively and improve your quality of life.
Common Symptoms of Osteoarthritis in the Spine
| Common Symptoms | Description |
|---|---|
| Pain | Localized or radiating pain in the neck or lower back |
| Stiffness | Difficulty moving or bending the neck or back |
| Decreased Range of Motion | Reduced flexibility and limited ability to perform certain movements |
| Numbness or Tingling | Sensations of pins and needles or numbness in the arms or legs |
| Weakened Reflexes | Reduced or absent reflexes in the affected areas |
| Muscle Weakness | Lack of strength or difficulty engaging certain muscle groups |
Other Sites of Osteoarthritis
Osteoarthritis typically affects well-known joints such as the hands, knees, hips, and spine. However, it’s important to note that osteoarthritis can also target less common locations in the body. These include:
- Neck: Osteoarthritis can cause pain, stiffness, and reduced mobility in the neck, making it challenging to turn the head and perform daily activities.
- Ankles: The ankles can experience osteoarthritis, leading to discomfort, swelling, and difficulty with walking or standing for prolonged periods.
- Shoulders: Osteoarthritis in the shoulders can result in pain, limited range of motion, and difficulty performing tasks that require overhead movement.
- Toes: The joints in the toes can be affected by osteoarthritis, causing pain, swelling, and difficulty wearing certain types of shoes.
Each of these less common sites of osteoarthritis may present its own set of symptoms and challenges. It’s essential to identify and manage osteoarthritis in these locations to alleviate discomfort and enhance quality of life.
“While hands, knees, hips, and spine are the common sites for osteoarthritis, it can also affect other joints in the body.”
Prevalence of Osteoarthritis
Osteoarthritis is a widespread condition that affects millions of adults in the United States. The prevalence of osteoarthritis increases with age, but it can also impact younger individuals, especially those who have had previous joint injuries. It is important to note that osteoarthritis is not solely an inevitable result of aging, as some people may never develop this condition.
According to our findings, over 32.5 million adults in the United States are affected by osteoarthritis[^3^]. This staggering number highlights the significant impact of this degenerative joint disease on our population.
We should be aware that different regions may have varying rates of osteoarthritis cases. Identified geographic areas with the highest prevalence of osteoarthritis will allow us to allocate resources more effectively and implement targeted preventive measures and treatments. By understanding these regional trends, we can develop strategies to promote joint health and improve the quality of life for those living with osteoarthritis.
| Region | Prevalence of Osteoarthritis |
|---|---|
| Region A | XX% |
| Region B | XX% |
| Region C | XX% |
| Region D | XX% |
These statistics demonstrate the need for targeted interventions in regions with higher osteoarthritis prevalence. By focusing on these areas and providing access to appropriate healthcare services, we can have a significant impact on reducing the burden of osteoarthritis and improving the lives of individuals living with this condition.
It is essential that we continue to conduct research and gather data on osteoarthritis prevalence in different regions. This information will drive evidence-based decision-making and enable us to implement effective public health strategies, early detection programs, and interventions that can help reduce the impact of osteoarthritis on individuals and society as a whole.
Conclusion
Osteoarthritis is a common degenerative joint disease that can affect various parts of the body. The hands, knees, hips, and spine are the most commonly affected sites. However, osteoarthritis can also be found in other joints such as the neck, ankles, shoulders, and toes. Understanding the common sites of osteoarthritis is crucial for recognizing the symptoms and seeking appropriate treatment and management.
Osteoarthritis has a significant geographic distribution, with millions of adults affected globally. While age is a risk factor, other factors such as joint injuries and genetics can also contribute to its development. It is important to note that osteoarthritis is not an inevitable aging disease, and some people may never develop it.
To address the high prevalence of osteoarthritis, countries worldwide need to focus on promoting awareness, early diagnosis, and effective treatment options. By providing education and support, we can help individuals manage their osteoarthritis and improve their quality of life. Together, we can work towards reducing the burden of this chronic condition.
FAQ
What are the common sites for osteoarthritis?
Osteoarthritis most commonly affects joints in the hands, knees, hips, and spine. However, it can also be found in other joints such as the neck, ankles, shoulders, and toes.
What are the symptoms of osteoarthritis in the hands?
Osteoarthritis in the hands may cause pain, stiffness, and swelling. Finger joints may become enlarged and tender, making it difficult to grasp objects. The joint at the base of the thumb is commonly affected, leading to pain and limited mobility.
How does osteoarthritis affect the knees?
Osteoarthritis in the knees can lead to cartilage wear down, causing pain, stiffness, and difficulty with walking or climbing stairs. Weakness or instability in the knee joint may also be present, making activities challenging.
What are the common symptoms of hip osteoarthritis?
Osteoarthritis can affect the hip joint, causing pain that may radiate to the groin, buttocks, or knee. Cartilage damage in the “ball and socket” joint of the hip can lead to limited mobility and discomfort while walking or performing daily activities.
How does osteoarthritis impact the spine?
In osteoarthritis of the spine, the disks between the vertebrae may narrow, and bone spurs can form. This can lead to pain, stiffness, and a decreased range of motion. The neck and lower back are commonly affected areas.
Besides the common sites, where else can osteoarthritis occur?
Osteoarthritis can also affect other joints in the body such as the neck, ankles, shoulders, and toes. Each of these sites may have its own specific symptoms and challenges associated with osteoarthritis.
How prevalent is osteoarthritis?
Osteoarthritis is a widespread condition, with over 32.5 million adults affected by it in the United States alone. Its prevalence increases with age, but it can also affect younger individuals, especially those who have had prior joint injuries.
Which regions have the highest prevalence of osteoarthritis?
Osteoarthritis is prevalent globally, affecting millions of adults. It is important to note that the geographic distribution of osteoarthritis varies, and it can be found in countries all around the world.