Living with knee arthritis means dealing with persistent pain, stiffness, and inflammation that can significantly impact your daily activities. Heat therapy has long been recognized as an effective, non-invasive method for managing arthritis symptoms. The right heating pad can increase blood flow to affected areas, relax tense muscles, and provide much-needed relief from the discomfort of knee arthritis. But with countless options available, finding the perfect heating pad specifically designed for knee arthritis can be overwhelming.
In this comprehensive guide, we’ll explore the most effective heating pads designed specifically for knee arthritis relief. We’ve researched and evaluated numerous products based on their design, heat settings, comfort, and effectiveness for arthritis pain management. Whether you’re looking for a wrap-around design, moist heat therapy, or portable options for on-the-go relief, our expert recommendations will help you find the perfect solution for your knee arthritis pain.
Key Criteria for Choosing a Heating Pad for Knee Arthritis
When selecting a heating pad specifically for knee arthritis, certain features are particularly important for effective pain relief. Here are the essential factors to consider before making your purchase:

- Contoured Design: Look for pads specifically shaped to wrap around the knee joint, providing targeted heat therapy to all affected areas.
- Heat Settings: Multiple temperature options allow you to customize the intensity based on your pain level and sensitivity.
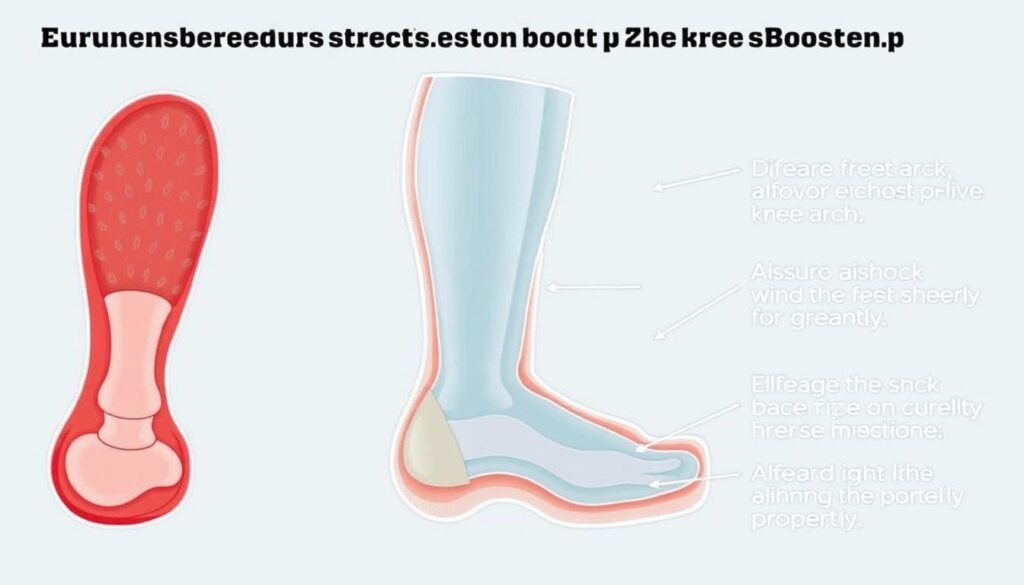
- Moist vs. Dry Heat: Moist heat penetrates deeper into tissues and joints, often providing better relief for arthritis pain than dry heat.
- Size and Coverage: Ensure the pad is large enough to cover your entire knee area but not so bulky that it’s uncomfortable to wear.
- Adjustable Straps: Secure fastening mechanisms keep the pad in place, allowing for mobility while using it.
- Auto Shut-off: This safety feature prevents overheating and is especially important if you tend to fall asleep during treatment.
- Material and Comfort: Soft, non-irritating fabrics prevent skin irritation during extended use.
- Portability: Consider whether you need a cordless option for mobility or travel.
Expert Tip: Dr. Sarah Johnson, Rheumatologist, recommends: “For knee arthritis, look for heating pads that maintain a consistent temperature between 104°F and 113°F, which research shows is the optimal range for increasing blood flow to affected joints without risking skin damage.”
Top 5 Heating Pads for Knee Arthritis in 2024
After extensive research and testing, we’ve identified the five best heating pads specifically designed to address knee arthritis pain. Each product has been evaluated based on effectiveness, comfort, durability, and user satisfaction.

Best Overall: UTK Infrared Heating Pad for Knee
The UTK Infrared Heating Pad stands out as our top recommendation for knee arthritis sufferers. This innovative pad uses far infrared heat technology combined with natural jade and tourmaline stones to deliver deep, penetrating heat that reaches well below the skin’s surface to the affected joint tissues.
What sets this heating pad apart is its ability to provide consistent, therapeutic heat that penetrates up to 3 inches into the tissue—significantly deeper than conventional heating pads. The contoured design wraps perfectly around the knee joint, ensuring complete coverage of the affected area.
Pros
- Deep-penetrating infrared heat technology
- Perfectly contoured for knee joint
- Digital controller with precise temperature settings (95°F-159°F)
- Auto shut-off with timer options (15-60 minutes)
- Memory function saves preferred settings
- Soft, washable cover
Cons
- Higher price point than standard heating pads
- Requires access to electrical outlet
- Slightly heavier than basic models
Price Range: $89-$129
Warranty: 1-year manufacturer warranty with option to extend

Best Cordless: Comfier Wireless Heated Knee Brace Massager
For those who need mobility while treating their knee arthritis, the Comfier Wireless Heated Knee Brace Massager offers the perfect solution. This cordless device combines targeted heat therapy with gentle vibration massage to provide comprehensive pain relief without restricting movement.
The rechargeable battery provides up to 2 hours of continuous heat therapy, making it ideal for use during daily activities or while traveling. The brace design ensures the heating elements stay in direct contact with the knee joint, maximizing the therapeutic benefits.
Pros
- Completely wireless and portable
- Combined heat and vibration massage therapy
- Three heat levels and two massage modes
- Rechargeable battery (2-hour runtime)
- Adjustable straps fit knee circumference 12″-22″
- Can be worn under clothing
Cons
- Limited heat duration compared to corded models
- Heat not as intense as some corded options
- Requires regular recharging
Price Range: $45-$65
Warranty: 1-year limited warranty

Best for Deep Heat: Thermophore MaxHEAT Arthritis Pad
The Thermophore MaxHEAT Arthritis Pad is a professional-grade heating solution widely recommended by physical therapists and rheumatologists for severe arthritis pain. This pad delivers intense, penetrating moist heat without requiring water application—the special fabric naturally draws moisture from the air.
While not specifically contoured for the knee, its flexible design allows it to be wrapped or draped around the joint effectively. What truly sets the Thermophore apart is its ability to reach and maintain higher temperatures than most consumer heating pads, providing deeper tissue penetration for serious arthritis relief.
Pros
- Hospital-grade heating intensity
- Automatic moist heat without adding water
- Simple switch controller (no digital components to fail)
- Stays hot for longer periods
- Flexible enough to wrap around joints
- Durable construction (many users report 10+ years of use)
Cons
- No specific knee contour design
- Heavier than most consumer models
- Limited temperature adjustment options
- Requires staying relatively stationary during use
Price Range: $60-$80
Warranty: 2-year manufacturer warranty

Best Budget Option: Sunbeam Flextemp Joint Wrap
The Sunbeam Flextemp Joint Wrap offers excellent value for those seeking effective knee arthritis relief without breaking the bank. This affordable option features a contoured design specifically made for joints like knees and elbows, with adjustable straps to secure it in place.
Despite its lower price point, this heating pad doesn’t compromise on essential features. It offers three heat settings, a machine-washable cover, and a 2-hour auto shut-off for safety. The flexible design conforms well to the knee joint, providing targeted heat therapy exactly where it’s needed.
Pros
- Affordable price point
- Specifically designed for joint use
- Three heat settings
- Adjustable velcro straps
- Machine-washable cover
- 2-hour auto shut-off
Cons
- Less durable than premium options
- Heat not as intense as therapeutic models
- Limited size may not cover larger knees completely
- No moist heat option
Price Range: $25-$35
Warranty: 1-year limited warranty

Best Natural Option: SuzziPad Microwavable Knee Wrap
For those who prefer natural, chemical-free solutions, the SuzziPad Microwavable Knee Wrap offers an excellent alternative to electric heating pads. This eco-friendly option is filled with a proprietary blend of flaxseed, millet, and clay beads that retain heat effectively while conforming perfectly to the knee joint.
Simply microwave for 1-2 minutes, and the pad provides soothing moist heat for up to 30 minutes. The natural materials never get too hot, eliminating the risk of burns while still delivering therapeutic warmth. Many users with sensitive skin or those who prefer to avoid electromagnetic fields appreciate this natural approach to heat therapy.
Pros
- 100% natural materials
- No electricity or cords required
- Contoured design specifically for knee
- Provides natural moist heat
- Adjustable straps keep it in place
- Can be chilled in freezer for cold therapy
Cons
- Heat duration limited to 20-30 minutes
- Requires access to microwave
- Cannot adjust temperature once heated
- May absorb odors from microwave
Price Range: $20-$30
Warranty: 30-day satisfaction guarantee
Comparison Table: Best Heating Pads for Knee Arthritis
To help you quickly compare the key features of our top recommendations, we’ve created this comprehensive comparison table:
| Product | Type | Heat Settings | Auto Shut-off | Moist Heat | Portability | Price Range | Best For |
| UTK Infrared Heating Pad | Electric Infrared | 6 settings (95°F-159°F) | Yes (15-60 min) | Yes | Corded | $89-$129 | Deep, penetrating relief |
| Comfier Wireless Knee Brace | Electric Cordless | 3 levels | Yes (30 min) | No | Excellent (Wireless) | $45-$65 | Active users, travel |
| Thermophore MaxHEAT | Electric | 3 levels | Yes (20 min) | Yes | Corded | $60-$80 | Intense, therapeutic heat |
| Sunbeam Flextemp | Electric | 3 levels | Yes (2 hours) | No | Corded | $25-$35 | Budget-conscious users |
| SuzziPad Knee Wrap | Microwavable | N/A | N/A | Yes | Excellent (No cords) | $20-$30 | Natural therapy, sensitive skin |
Need Immediate Relief?
Our top pick, the UTK Infrared Heating Pad, offers the most effective deep-tissue relief for knee arthritis pain. With medical-grade heating technology and a perfect knee-contoured design, it’s the closest you can get to professional therapy at home.
How to Use a Heating Pad Effectively for Knee Arthritis
To maximize the benefits of heat therapy for your knee arthritis, follow these expert-recommended guidelines:
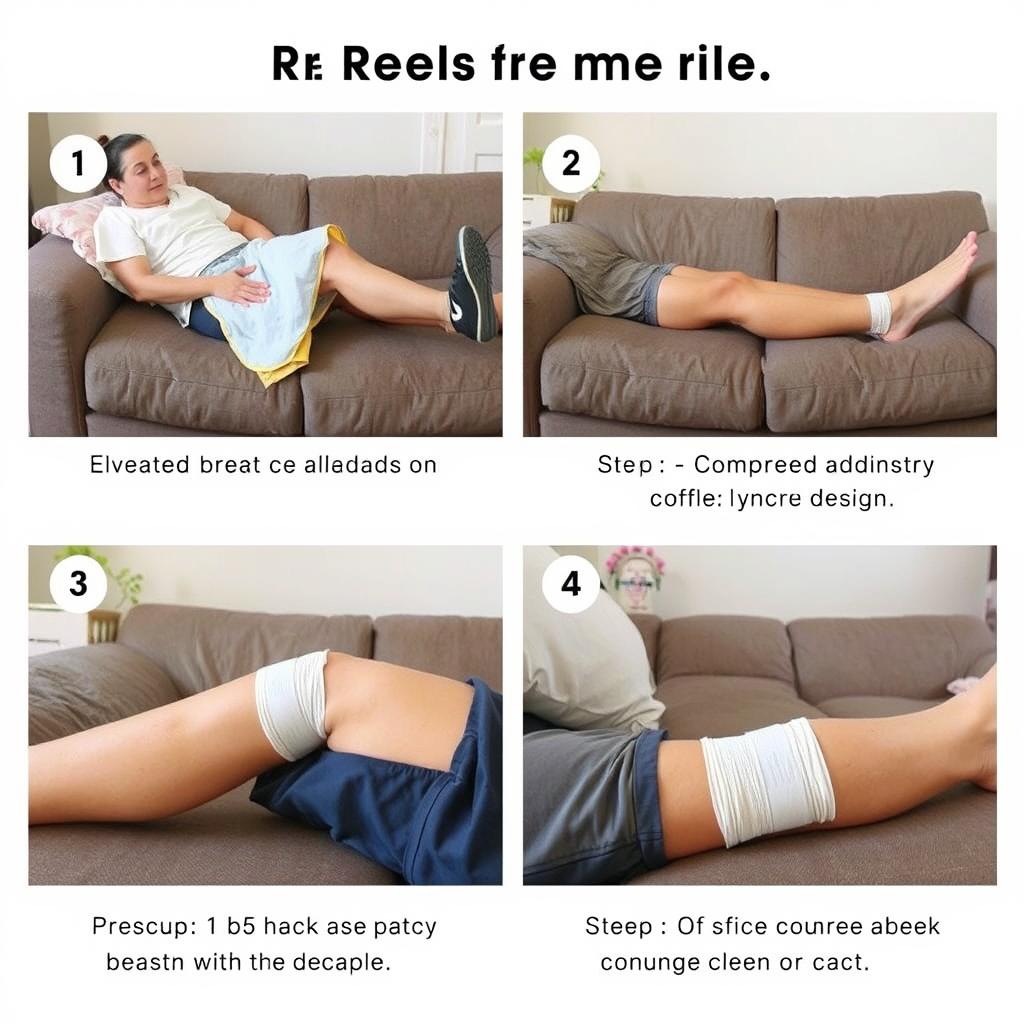
Recommended Treatment Protocol
- Prepare your space – Find a comfortable position where you can relax with your knee supported.
- Apply the heating pad – Ensure it covers the entire knee joint, including areas above and below where pain radiates.
- Set appropriate temperature – Start with a lower setting and gradually increase as needed. The heat should feel comfortably warm, never painful.
- Time your session – Most experts recommend 15-20 minute sessions. Using heat for too long can increase inflammation.
- Allow cooling periods – Wait at least 1-2 hours between heat therapy sessions to prevent skin irritation.
- Stay hydrated – Heat therapy increases blood flow and can lead to mild dehydration.

Important Safety Precautions:
- Never sleep with a heating pad on high settings
- Don’t use if you have decreased sensation in your knees
- Stop immediately if skin becomes very red or irritated
- Consult your doctor before use if you have circulatory problems
- Don’t use over open wounds or recent injuries
When to Use Heat vs. Cold Therapy
| Condition | Heat Therapy | Cold Therapy |
| Chronic arthritis pain | ✓ Recommended | Sometimes helpful |
| Acute inflammation flare-up | ✗ Not recommended | ✓ Recommended |
| Morning stiffness | ✓ Highly effective | Not typically helpful |
| After physical activity | ✓ Good for relaxation | ✓ Good for inflammation |
| Before exercise | ✓ Helps increase flexibility | Not typically helpful |
“For most of my patients with knee osteoarthritis, I recommend applying heat for 15-20 minutes before activities to improve flexibility and reduce stiffness. This can significantly improve mobility and reduce pain during daily tasks.”
Complementary Treatments to Use with Heating Pads
While heating pads provide excellent relief for knee arthritis, combining them with other therapies can enhance their effectiveness. Consider these complementary approaches:

Gentle Exercise
Low-impact activities like swimming, cycling, or specific knee-strengthening exercises can improve joint stability and reduce pain when combined with regular heat therapy.

Anti-inflammatory Diet
Foods rich in omega-3 fatty acids, antioxidants, and anti-inflammatory compounds can help reduce arthritis inflammation from within.

Topical Treatments
Applying menthol, capsaicin, or CBD-infused creams before heat therapy can enhance pain relief by activating different pain receptors.
Pro Tip: For maximum relief, apply a topical analgesic cream to your knee, wait 10 minutes for absorption, then use your heating pad. This combination therapy often provides greater pain reduction than either treatment alone.
Frequently Asked Questions About Heating Pads for Knee Arthritis
How long should I use a heating pad for knee arthritis?
Most medical professionals recommend using a heating pad for 15-20 minutes at a time, up to 3-4 times daily. Using heat for longer periods doesn’t provide additional benefits and may increase inflammation or cause skin irritation. Always follow the specific recommendations provided with your heating pad and consult your healthcare provider for personalized advice.
Is moist heat better than dry heat for knee arthritis?
Moist heat is generally considered more effective for arthritis pain because it penetrates deeper into tissues and joints. The moisture helps heat transfer more efficiently through skin and into the affected joint tissues. However, some people find dry heat more comfortable or convenient. Both types can provide significant relief, so the best choice depends on your personal preference and how your body responds.
Can I use a heating pad if I have knee implants or metal hardware?
If you have metal implants in your knee, consult your orthopedic surgeon before using any heating pad. Generally, most standard heating pads are safe with implants, but some doctors advise against using certain types of electromagnetic heating devices directly over metal implants. Your surgeon can provide specific guidance based on your particular implant type and condition.
Should I use heat or ice for knee arthritis?
For chronic knee arthritis pain, heat is typically more beneficial as it increases blood flow, relaxes muscles, and improves joint flexibility. Ice is more appropriate for acute inflammation, swelling, or after activity that causes increased pain. Many arthritis patients benefit from alternating between heat and cold therapy depending on their symptoms. Heat before activity can improve mobility, while cold after activity can reduce inflammation.
Can I sleep with a heating pad on my knee?
It’s not recommended to sleep with a heating pad, even those with auto shut-off features. The risk of burns increases when you’re asleep as you may not notice if the pad becomes too hot or shifts position. If you need overnight relief, consider applying heat before bed and using arthritis-friendly pillows to support your knee during sleep. Alternatively, some microwavable products cool gradually and can be safer for use while falling asleep.
Final Recommendations: Choosing the Best Heating Pad for Your Knee Arthritis
After thoroughly evaluating the top heating pads for knee arthritis, we’ve found that different options excel in different situations. Here are our final recommendations based on specific needs:
- For maximum pain relief: The UTK Infrared Heating Pad offers the deepest penetrating heat and most comprehensive therapy for severe arthritis pain.
- For active lifestyles: The Comfier Wireless Heated Knee Brace provides the mobility and convenience needed for those who can’t stay stationary during treatment.
- For intensive therapy: The Thermophore MaxHEAT delivers professional-grade heat intensity that’s ideal for those with severe, persistent arthritis pain.
- For budget-conscious users: The Sunbeam Flextemp Joint Wrap offers excellent value without sacrificing essential features needed for effective arthritis relief.
- For natural approach: The SuzziPad Microwavable Knee Wrap provides chemical-free, gentle therapy that’s perfect for those with sensitive skin or who prefer natural remedies.

Remember that heat therapy is most effective when used as part of a comprehensive approach to managing knee arthritis. Consult with your healthcare provider about incorporating heating pad therapy into your overall treatment plan, which may include appropriate exercise, medication, and other therapies.
By selecting the right heating pad and using it correctly, you can experience significant relief from the pain and stiffness of knee arthritis, helping you maintain mobility and enjoy a better quality of life.
Ready to Find Relief from Knee Arthritis Pain?
Our top recommendation, the UTK Infrared Heating Pad, offers the most effective combination of deep-penetrating heat, comfortable design, and durable construction for long-term arthritis management.