Welcome to our informative guide on understanding knee osteoarthritis diagnosis. In this article, we will explore the process of diagnosing knee osteoarthritis, including when it is diagnosed and how it can be detected early. If you are experiencing knee pain or have concerns about osteoarthritis, read on to gain valuable insights into this common condition.
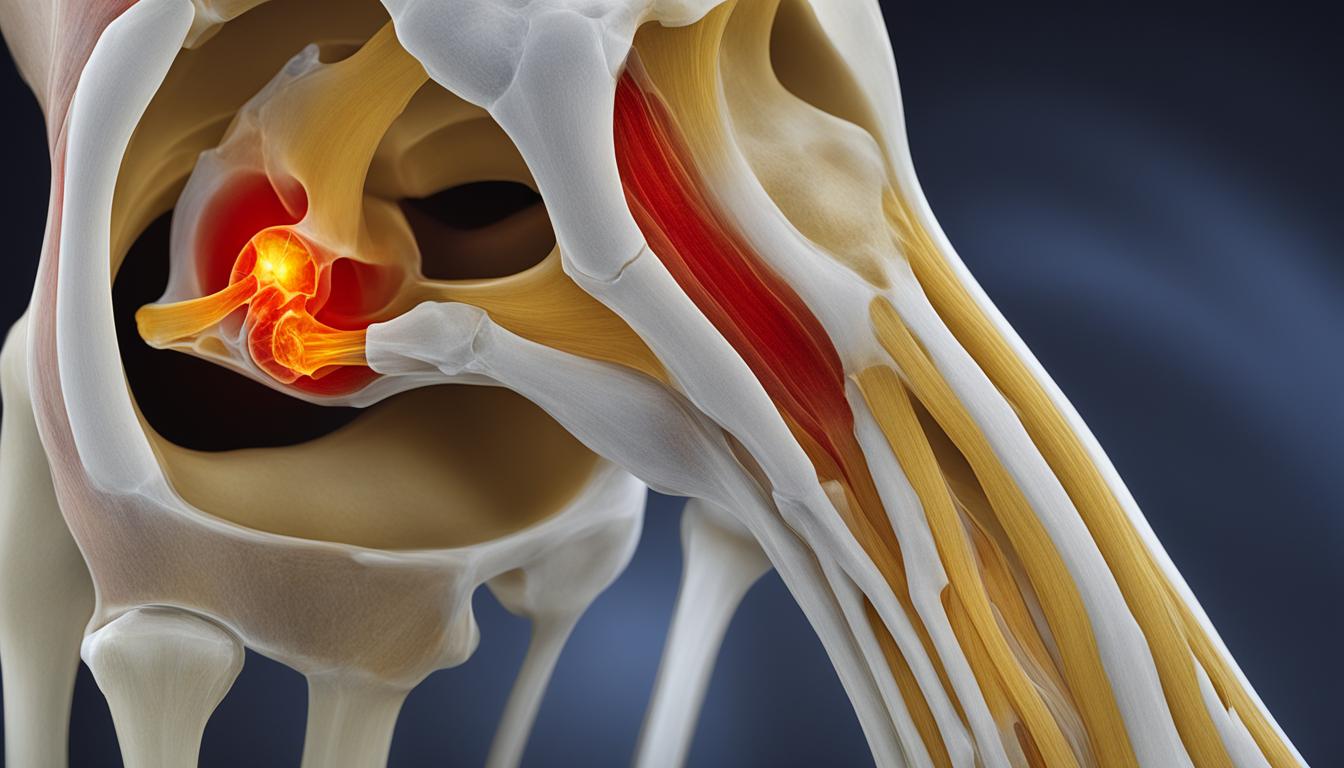
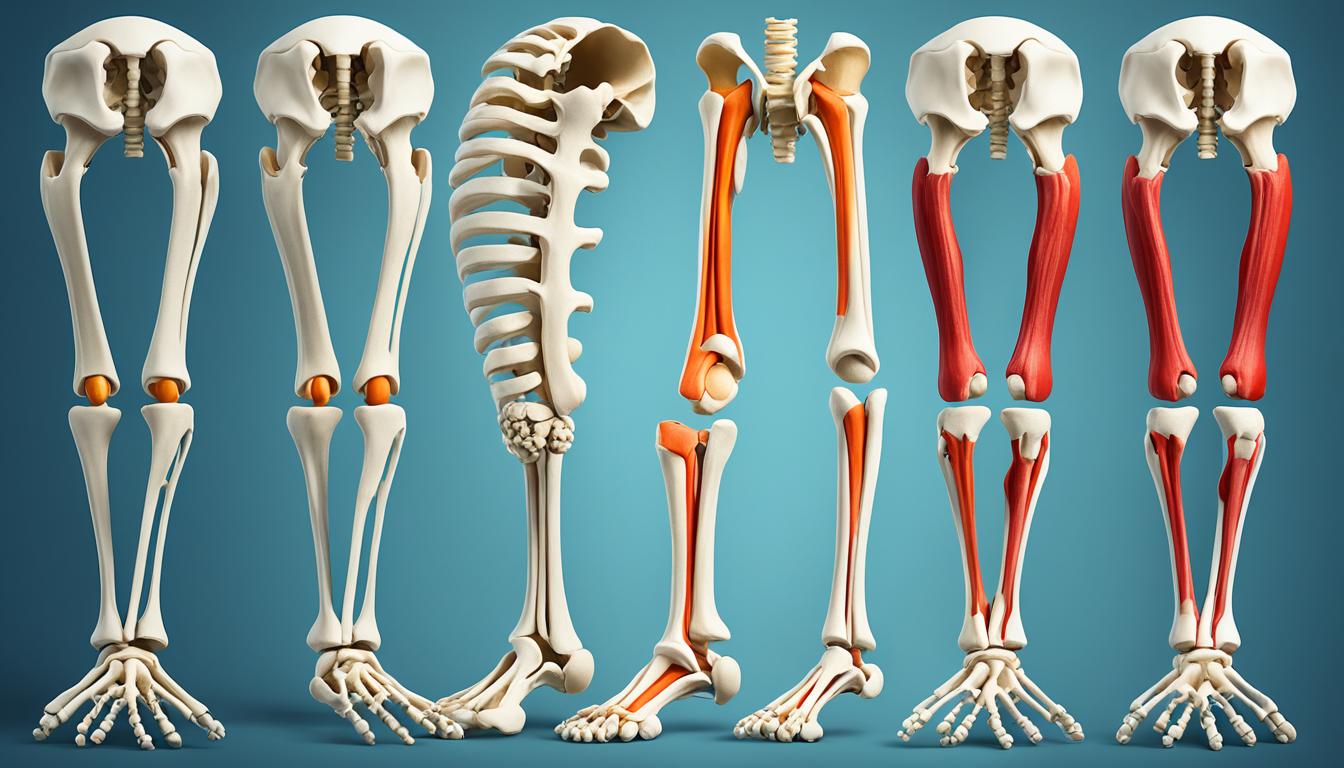
Knee osteoarthritis is a progressive condition that affects the knee joint, causing aching pain, stiffness, and a loss of mobility. It can occur in people over the age of 60, as a result of years of daily movements, or in younger individuals due to knee injuries or high-impact activities.
The diagnosis of knee osteoarthritis is based on a combination of symptoms and diagnostic imaging tests. This involves a thorough medical history and physical examination, as well as the use of imaging techniques such as X-rays and ultrasound.
Early detection of knee osteoarthritis is crucial for effective management and treatment. By accurately diagnosing the condition, healthcare professionals can develop a personalized treatment plan that focuses on reducing pain, improving joint function, and preventing further progression of the disease.
Throughout this article, we will delve deeper into the symptoms, diagnostic methods, and available treatment options for knee osteoarthritis. Join us on this journey to gain a better understanding of this common condition and find the support you need for optimal knee health.
Symptoms of Knee Osteoarthritis
Knee osteoarthritis is characterized by several distinct symptoms. Understanding and identifying these symptoms is crucial for the detection and diagnosis of this degenerative joint disease.
The key symptoms of knee osteoarthritis include:
- Aching pain: Individuals with knee osteoarthritis often experience persistent pain in the knee joint. This pain may be present all the time or may worsen during certain activities.
- Stiffness: A common symptom of knee osteoarthritis is stiffness in the knee joint, making it difficult to move or bend the knee smoothly.
- Loss of mobility: As knee osteoarthritis progresses, individuals may notice a gradual loss of mobility in the affected knee, making it challenging to perform daily activities or engage in physical exercise.
- Grinding or clicking sound: Some people with knee osteoarthritis may hear a grinding or clicking sound when they move their knee joint. This sound, known as crepitus, occurs due to the rubbing of bone surfaces.
- Limitation of day-to-day activities: Knee osteoarthritis can significantly impact one’s ability to perform day-to-day activities, such as walking, climbing stairs, or getting up from a chair, due to pain or stiffness.
- Swelling, warmth, or redness: In some cases, the affected knee joint may exhibit symptoms of inflammation, such as swelling, redness, or warmth.
To identify these symptoms and make an accurate diagnosis of knee osteoarthritis, healthcare professionals rely on a combination of methods, including medical history assessments, physical examinations, and diagnostic imaging tests, such as X-rays.

| Symptom | Description |
|---|---|
| Aching pain | Persistent pain in the knee joint, experienced all the time or during certain activities |
| Stiffness | Difficulty moving or bending the knee smoothly |
| Loss of mobility | Gradual decrease in the ability to perform activities due to knee joint limitations |
| Grinding or clicking sound | Noise during knee movement caused by bone-on-bone friction |
| Limitation of day-to-day activities | Difficulty performing routine tasks due to pain or stiffness |
| Swelling, warmth, or redness | Inflammation-related symptoms in the knee joint |
Identifying these symptoms early on can help individuals seek proper medical care and develop an effective treatment plan that targets the management of knee osteoarthritis.
Diagnosing Knee Osteoarthritis
When it comes to diagnosing knee osteoarthritis, doctors employ a comprehensive approach that involves gathering relevant medical history and conducting a thorough physical examination. By combining these methods with diagnostic imaging tests, healthcare professionals can accurately diagnose knee osteoarthritis and determine the most appropriate treatment plan for the patient.
Medical history plays a crucial role in diagnosing knee osteoarthritis. It provides valuable information about the patient’s symptoms, including the onset of pain or stiffness, previous knee injuries or surgeries, and any other relevant medical conditions. By understanding the patient’s history, doctors can start to form a clearer picture of the potential causes of knee pain and identify the presence of osteoarthritis.
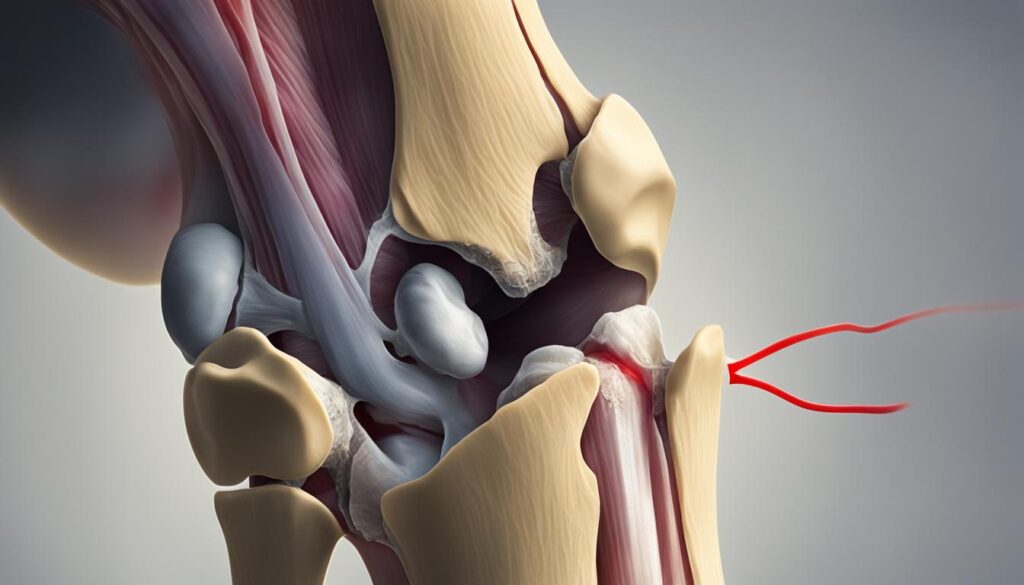
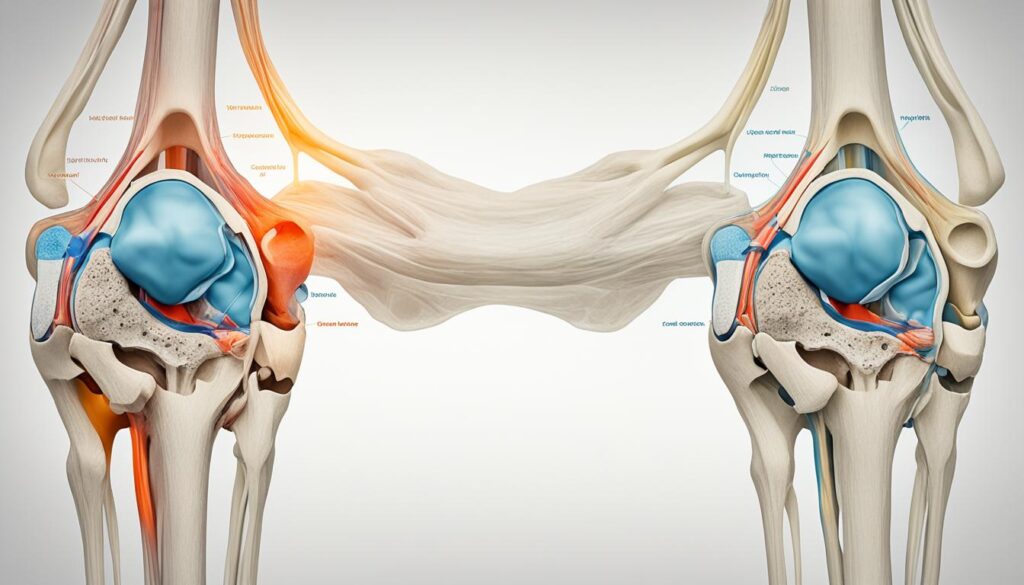
The physical examination further aids in the diagnosis of knee osteoarthritis. During this evaluation, doctors assess the flexibility and range of motion of the knee joint. They also look for signs of joint damage, such as tenderness, swelling, or deformity. By analyzing these factors, healthcare professionals can gather vital insights into the condition of the knee joint and determine the severity of osteoarthritis.
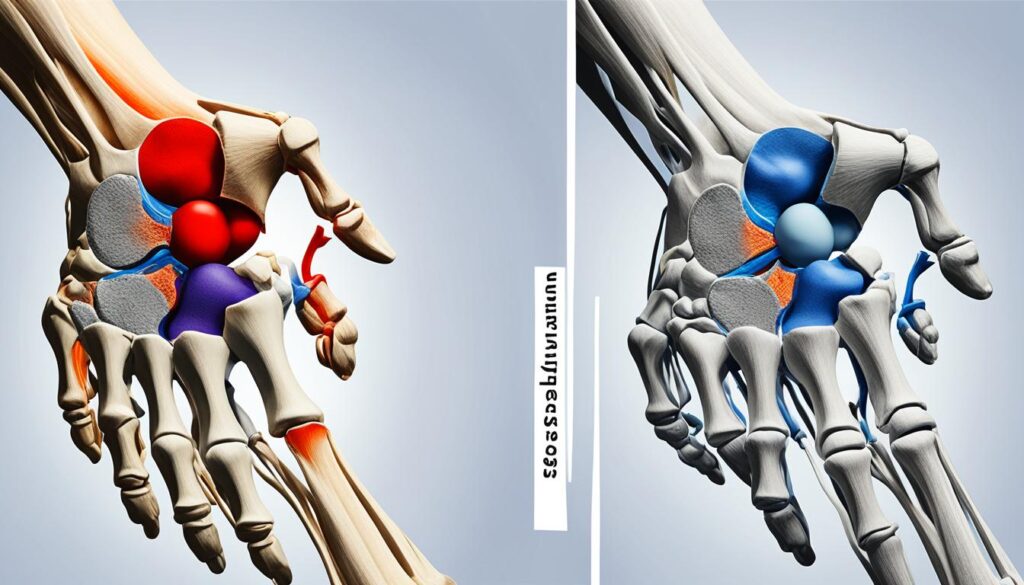
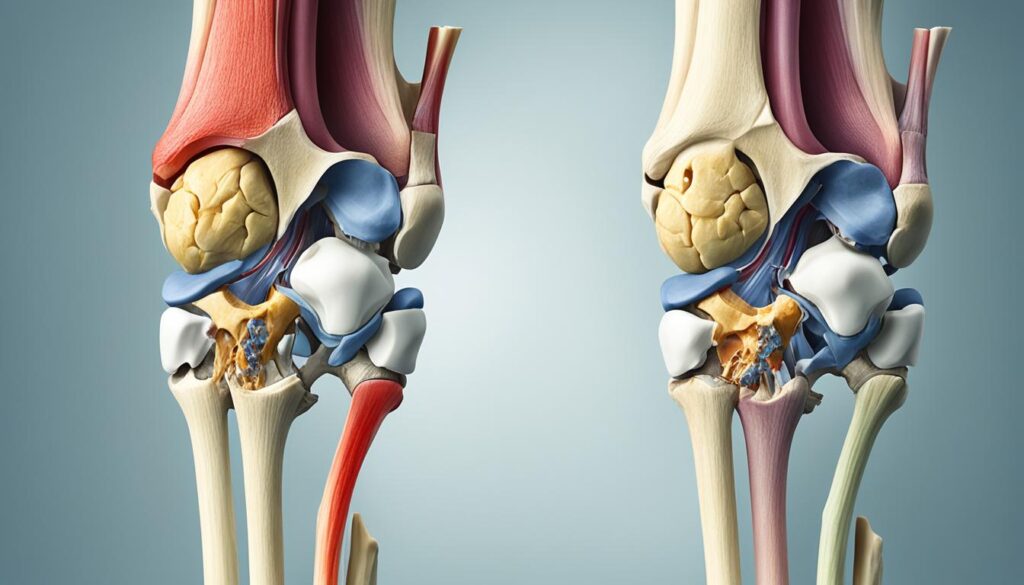
Diagnostic imaging tests are key components of the knee osteoarthritis diagnosis process. X-rays are commonly used to visualize the knee joint and identify characteristic signs of osteoarthritis, such as cartilage erosion, bone spurs, and narrowing of the joint space. This imaging technique provides a detailed view of the knee joint’s structure and helps confirm the presence of osteoarthritis.
In addition to X-rays, ultrasound is another valuable imaging tool used in the diagnosis of knee osteoarthritis. It can visualize soft tissue inflammation and excess fluid accumulation in the knee joint. By examining the joint with ultrasound, doctors can assess the extent of inflammation and determine if it contributes to the patient’s symptoms.
To further investigate the cause of joint pain and inflammation, doctors may perform arthrocentesis. This procedure involves removing fluid from the knee joint for analysis. By examining the fluid, healthcare professionals can identify any underlying conditions or infections that may be causing or contributing to the patient’s knee pain.
Another valuable tool in the diagnostic process is patient-reported outcome scores. These scores help assess the type of knee pain the patient is experiencing and provide insights into their level of function. By collecting detailed information directly from the patient, doctors can better understand the impact of knee osteoarthritis on their daily life and tailor the treatment plan accordingly.
Overall, diagnosing knee osteoarthritis entails a combination of medical history, physical examination, and diagnostic tests. The comprehensive approach enables healthcare professionals to make an accurate diagnosis and provide appropriate treatment options to manage knee osteoarthritis effectively.

| Diagnostic Methods | Key Information |
|---|---|
| Medical History | Onset of symptoms, previous knee injuries or surgeries |
| Physical Examination | Assessment of flexibility, range of motion, and signs of joint damage |
| X-rays | Visualization of cartilage erosion, bone spurs, and narrowing of joint space |
| Ultrasound | Visualize soft tissue inflammation and excess fluid accumulation |
| Arthrocentesis | Analysis of fluid from the knee joint to determine the cause of pain and inflammation |
| Patient-Reported Outcome Scores | Assessment of type of knee pain and level of function |
Treatment of Knee Osteoarthritis
When it comes to the treatment of knee osteoarthritis, our focus is on reducing pain, improving joint function, and preventing further progression of the disease. There are various options available, both surgical and non-surgical, depending on the severity of the condition and individual needs.
Surgical Options
In severe cases of knee osteoarthritis, surgical interventions may be necessary to provide relief and restore joint function. Some common surgical options include:
- Osteotomy: This procedure involves cutting and repositioning the bones around the knee joint to relieve pressure and improve alignment.
- Partial or Total Joint Replacement Surgery: This involves removing the damaged parts of the knee joint and replacing them with artificial components, such as metal or plastic.
- Other Procedures: In addition to the above options, cortisone injections and lubrication injections can also be performed to reduce pain and inflammation in the knee joint.
Non-Surgical Options
Non-surgical treatment options are often recommended as the first line of defense and can be effective in managing knee osteoarthritis. These options include:
- Exercise: Regular exercise, such as low-impact activities and strengthening exercises, can help improve joint flexibility and strengthen the surrounding muscles, reducing pain and improving function.
- Weight Management: Maintaining a healthy weight can significantly reduce the stress on the knee joints, relieving pain and slowing down the progression of the disease.
- Physical Therapy: Working with a physical therapist can help develop a customized treatment plan, including targeted exercises and techniques to improve joint mobility and reduce pain.
- Medications: Pain relievers and anti-inflammatory drugs may be prescribed to manage pain and reduce inflammation in the knee joint, providing temporary relief.
- Injections: Corticosteroids or hyaluronic acid injections can be administered directly into the knee joint to relieve pain and inflammation.
Alternative Therapies
In addition to traditional treatment options, alternative therapies can also be considered for managing knee osteoarthritis. These therapies include:
- Acupuncture: This ancient Chinese practice involves the insertion of thin needles into specific points on the body to reduce pain and promote healing.
- Glucosamine and Chondroitin Supplements: These supplements are thought to support cartilage health and may help reduce pain and stiffness in some individuals.
- Other Complementary Approaches: Some individuals find relief from knee osteoarthritis symptoms through techniques such as heat or cold therapy, massage, or transcutaneous electrical nerve stimulation (TENS).
By considering these various treatment options, individuals with knee osteoarthritis can work with their healthcare team to develop a personalized and effective treatment plan that best suits their needs.
| Treatment | Description |
|---|---|
| Surgical Options | Includes osteotomy, partial or total joint replacement surgery, cortisone injections, and lubrication injections. |
| Non-Surgical Options | Includes exercise, weight management, physical therapy, medications, and injections. |
| Alternative Therapies | Includes acupuncture, glucosamine and chondroitin supplements, and other complementary approaches. |
Conclusion
Diagnosing knee osteoarthritis is a comprehensive process that involves evaluating a patient’s medical history, conducting a physical examination, and utilizing diagnostic tests. Early detection and diagnosis are crucial for effectively managing knee pain and maintaining mobility. By identifying the condition in its early stages, healthcare professionals can implement appropriate treatment strategies to reduce symptoms, improve joint function, and prevent further disease progression.
Treatment options for knee osteoarthritis aim to alleviate pain, enhance mobility, and slow down the degenerative process. Non-surgical approaches, such as targeted exercises and medication, have proven to be effective in managing knee osteoarthritis and improving the quality of life for patients. However, in severe cases where non-surgical treatments are insufficient, surgical interventions may be necessary to restore joint function and alleviate pain.
It is crucial for individuals with knee osteoarthritis to collaborate with a healthcare team consisting of physicians, physiotherapists, and other specialists. By working together, patients can obtain personalized treatment plans that align with their specific needs and goals. Whether it’s through non-surgical interventions or surgical procedures, a comprehensive approach to knee osteoarthritis diagnosis and treatment can help individuals regain their mobility, reduce pain, and enhance their overall well-being.
FAQ
When is knee osteoarthritis diagnosed?
Knee osteoarthritis can be diagnosed at any age, but it is most commonly diagnosed in people over the age of 60. However, it can also occur in younger individuals due to knee injuries or high-impact activities.
What are the symptoms of knee osteoarthritis?
The symptoms of knee osteoarthritis include aching pain, stiffness, and loss of mobility in the knee joint. Pain may be experienced all the time or during certain activities. People with knee osteoarthritis may also hear a grinding or clicking sound during movement and may experience swelling, warmth, or redness in the knee joint.
How is knee osteoarthritis diagnosed?
The diagnosis of knee osteoarthritis is based on symptoms and diagnostic imaging tests. Medical history and physical examination are important in diagnosing knee osteoarthritis. X-rays and ultrasound are commonly used imaging tests to diagnose knee osteoarthritis. Patient-reported outcome scores and arthrocentesis, a procedure to remove fluid from the knee joint, are also used in the diagnostic process.
What is the treatment for knee osteoarthritis?
The treatment of knee osteoarthritis focuses on reducing pain, improving joint function, and preventing further progression of the disease. Non-surgical treatment options include exercise, weight management, physical therapy, and medications such as pain relievers and anti-inflammatory drugs. Injections of corticosteroids or hyaluronic acid may be recommended to relieve pain and inflammation. Surgical options for severe cases include osteotomy, partial or total joint replacement surgery, and other procedures like cortisone injections and lubrication injections. Alternative therapies like acupuncture, glucosamine and chondroitin supplements, and other complementary approaches can also be considered.