Did you know that the patella, also known as the kneecap, is the largest sesamoid bone in the human body? This small but mighty bone has a significant impact on our knee joint function and leg movement. Let’s explore the anatomical importance of the patella and its role in ensuring knee stability and efficient leg motion.
As we delve into the significance of the patella, we’ll discover how this unique bone serves as an attachment point for crucial tendons and ligaments, increasing the extension capacity of the quadriceps muscle. It also acts as a protective shield for deeper structures in the knee joint, safeguarding the quadriceps tendon from frictional forces.
Furthermore, the patella plays a key role in enhancing quadriceps efficiency by increasing the moment arm of the knee. This contributes to knee stability and allows for smooth and coordinated leg movement.
Join us as we uncover the structure, function, and clinical relevance of the patella, shedding light on common conditions affecting this vital bone and exploring the tests, imaging techniques, and treatment options available for patellar disorders.
By delving into the world of the patella, we can gain a deeper understanding of its importance in our daily lives and take proactive steps to maintain the health and well-being of our knees.
Common Conditions and Disorders Affecting the Patella
When it comes to the patella, there are several common conditions and disorders that individuals may experience. These conditions can have a significant impact on the stability and comfort of the knee joint, leading to discomfort and potential mobility issues. It is important to be aware of these conditions and seek medical attention if any symptoms arise. Let’s explore some of the common conditions that affect the patella:
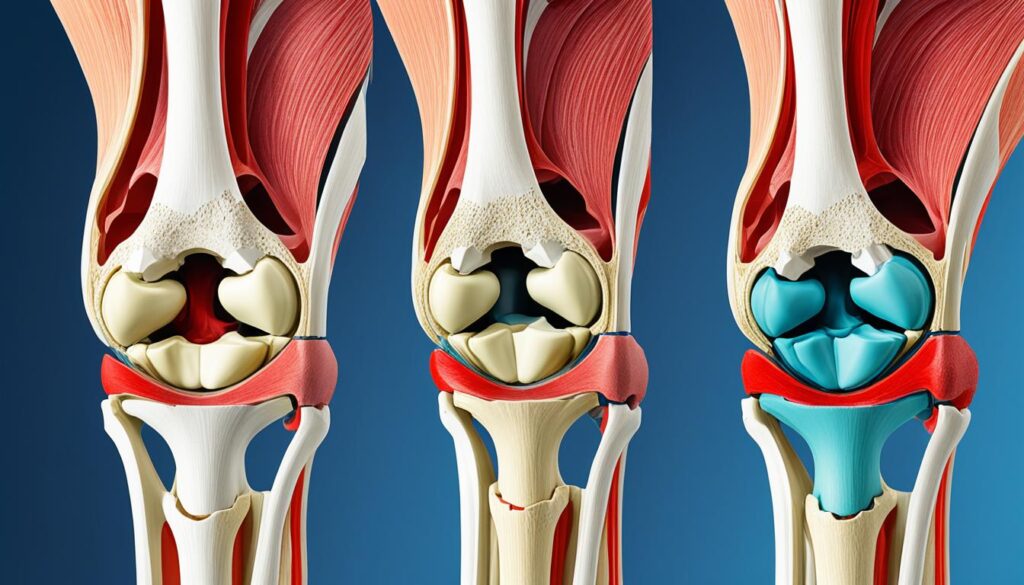
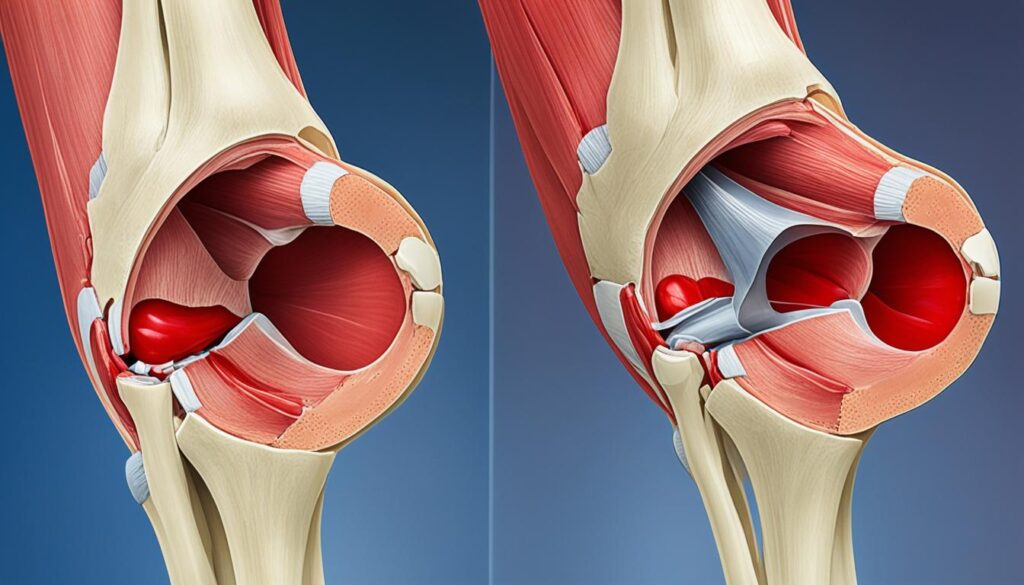
1. Patellar Dislocation
One common condition involving the patella is patellar dislocation. This occurs when the patella moves out of its normal position within the patellofemoral groove. Patellar dislocation can result from sudden twisting movements of the knee, causing instability and discomfort. Prompt medical attention is crucial to assess the severity of the dislocation and to determine the appropriate treatment plan.
2. Patellar Subluxation
Another condition that affects the patella is patellar subluxation. Similar to patellar dislocation, patellar subluxation involves the partial displacement of the patella from its normal position. This can also cause instability and discomfort in the knee joint. Individuals experiencing patellar subluxation should consult a healthcare professional for a proper evaluation and treatment.
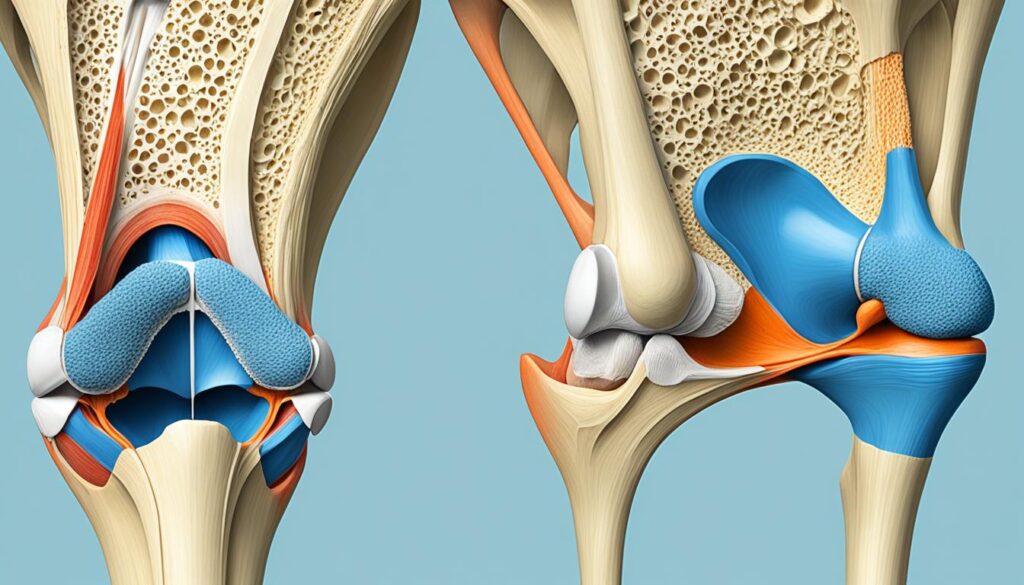
3. Osteoporosis
Osteoporosis, a condition characterized by a decrease in bone density, can also affect the patella. Weakened bones can make the patella more susceptible to fractures, as the reduced bone strength cannot withstand normal stress. It is important for individuals with osteoporosis to take precautions to prevent injuries, including proper nutrition, strength-building exercises, and medical management of the condition.
4. Knee Pain and Chondromalacia Patella
Knee pain is a common complaint that can be caused by various factors, including damage to the patella or the surrounding structures. A specific condition associated with knee pain is chondromalacia patella. This condition involves the softening and degeneration of the cartilage behind the patella, leading to discomfort and difficulty in knee movement. Individuals experiencing knee pain or chondromalacia patella should consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
It is important to note that this is not an exhaustive list of conditions that can affect the patella, but rather a starting point to raise awareness of the potential issues individuals may encounter. If you are experiencing new symptoms in your knees or difficulty walking or moving, it is essential to seek medical attention for an accurate diagnosis and personalized treatment plan.
| Condition | Description |
|---|---|
| Patellar Dislocation | When the patella moves out of its normal position within the patellofemoral groove |
| Patellar Subluxation | Partial displacement of the patella from its normal position |
| Osteoporosis | Condition characterized by decreased bone density, making the patella more susceptible to fractures |
| Knee Pain and Chondromalacia Patella | Discomfort caused by damage to the patella or surrounding structures, including softening and degeneration of the cartilage behind the patella |

Tests and Imaging for Patella Assessment
When diagnosing and evaluating conditions affecting the patella, healthcare professionals often utilize specific tests and imaging techniques to assess the extent of the injury or disorder. This section will discuss two commonly used approaches: the patella reflex test and various imaging tests.
Patella Reflex Test
The patella reflex test is a straightforward examination that helps assess the integrity of the neural connections in the knee. By tapping just below the patella with a reflex hammer, we can observe the involuntary leg extension that occurs when the associated nerves and muscles are functioning correctly. This test is crucial in evaluating the patellar reflex arc and identifying any underlying neurological abnormalities or injuries.
Performing the patella reflex test involves the following steps:
- Have the patient sit on the examination table with their legs dangling freely.
- Hold the reflex hammer firmly and, with a swift tap, strike the area just below the patella.
- Observe and record the patient’s leg response, including the intensity and timing of the extension.
The patella reflex test is a non-invasive and quick diagnostic tool that provides valuable information about the functionality of the reflex arc involving the patellar tendon and the quadriceps muscle.
Imaging Tests
If there is a suspected patellar injury or fracture, healthcare professionals may order imaging tests to gain a more detailed understanding of the condition. Common imaging techniques used for patella assessment include:
- X-rays: X-ray images allow us to evaluate the alignment, structure, and integrity of the patella bone. They can help identify fractures, dislocation, osteoarthritis, or other abnormalities.
- MRI scans: Magnetic Resonance Imaging (MRI) provides a more comprehensive view of the soft tissues surrounding the patella, such as ligaments, tendons, and cartilage. This imaging modality is particularly useful for detecting injuries or degenerative changes in these tissues.
Based on the results obtained from the imaging tests, healthcare professionals can formulate an accurate diagnosis and determine the appropriate treatment plan for the patient.
Treatment Options
Treatment for patella fractures depends on several factors, including the type and severity of the fracture. In some cases, immobilization with a brace or cast may be sufficient for healing the fracture, while more severe fractures may require surgical intervention to realign the bone.
When it comes to managing osteoporosis, treatments may involve a combination of lifestyle changes, exercise programs, and medications. Healthcare professionals may recommend weight-bearing exercises to improve bone density and strength, along with calcium and vitamin D supplements to support overall bone health. In severe cases, prescription medications may be prescribed to slow down bone loss or promote bone formation.
It is important to consult with healthcare professionals for a proper diagnosis and to discuss suitable treatment options based on individual circumstances.
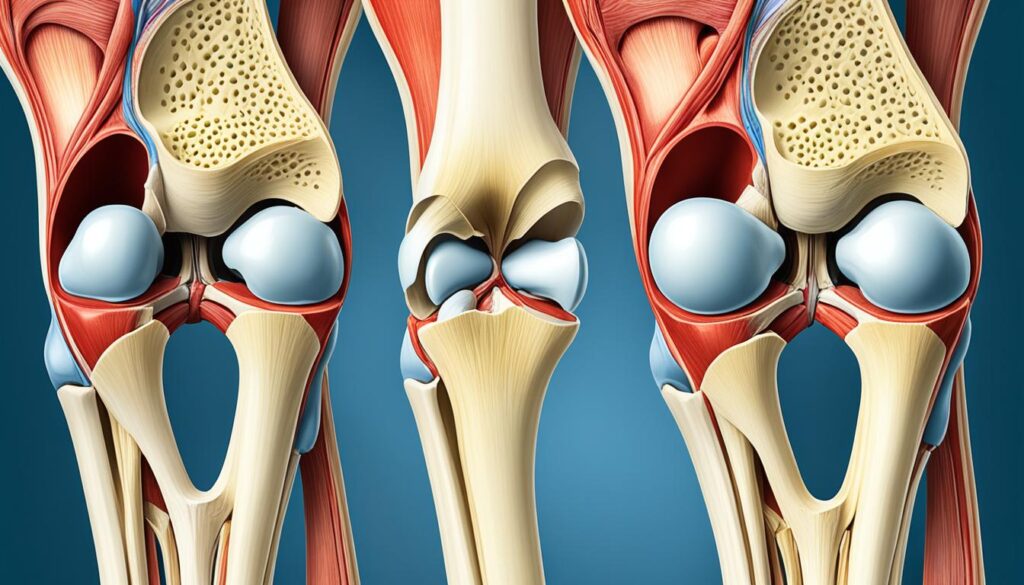
Structure and Function of the Patella
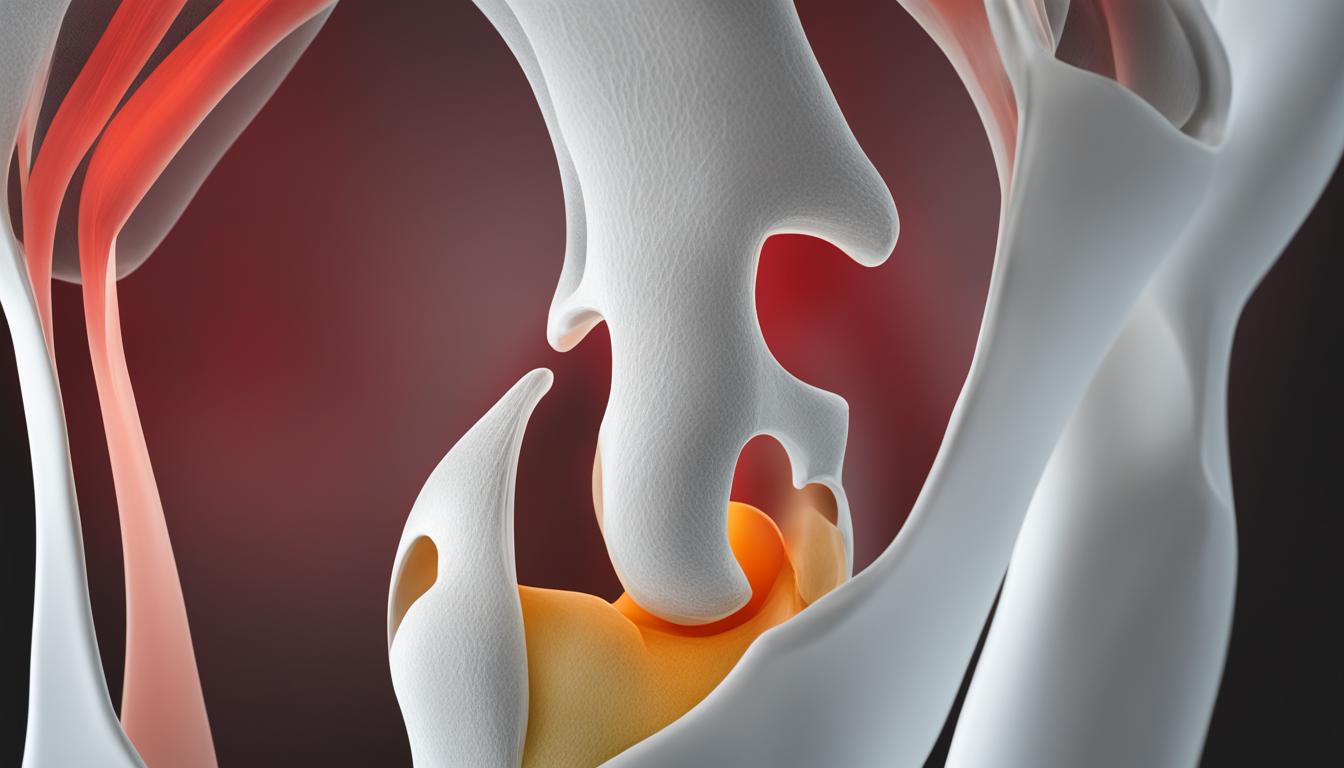
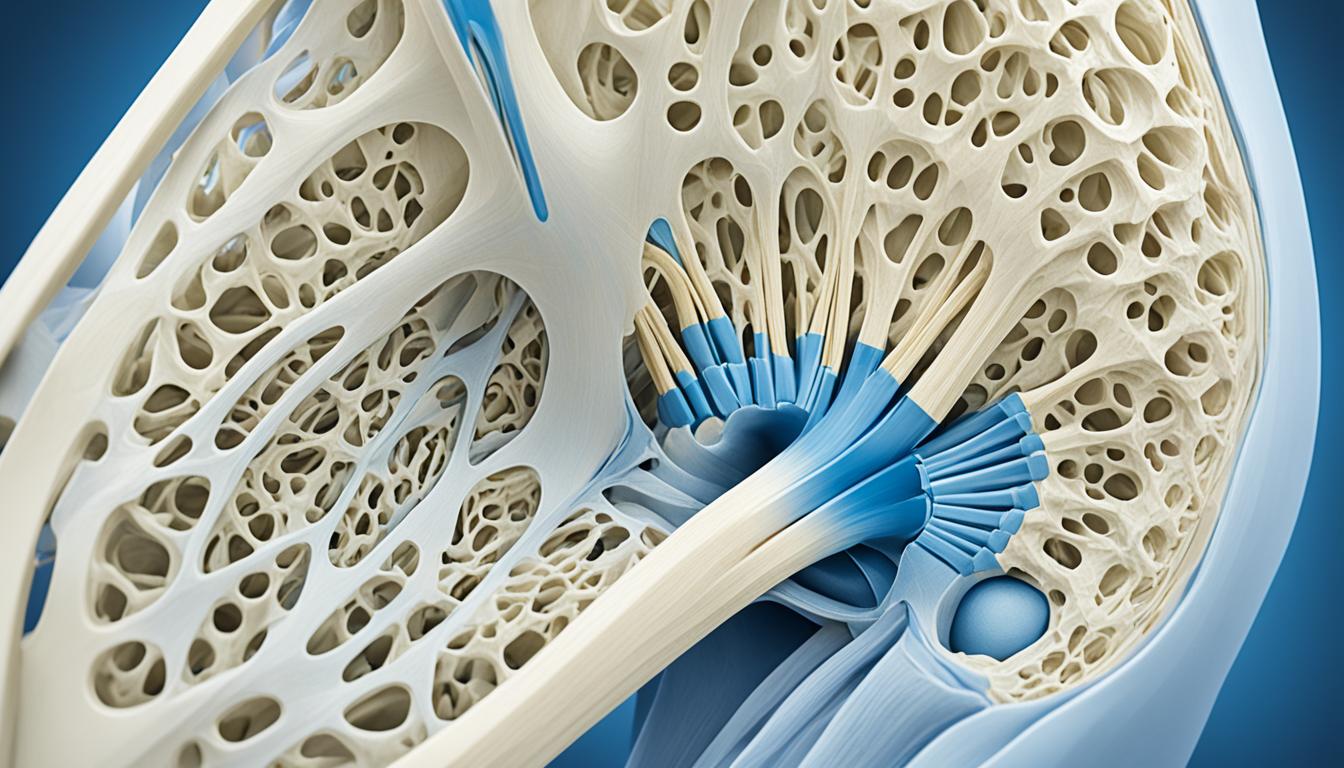
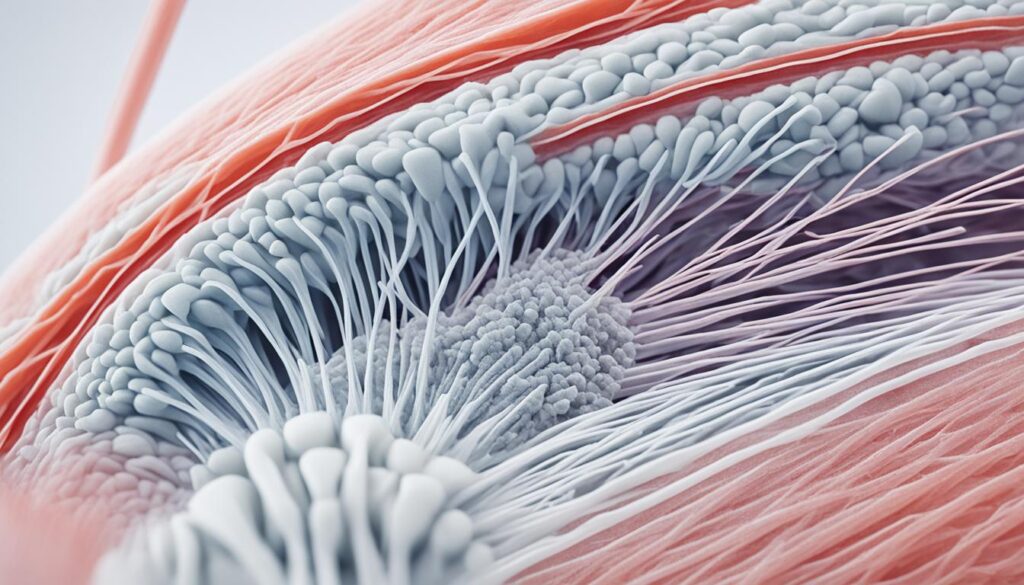
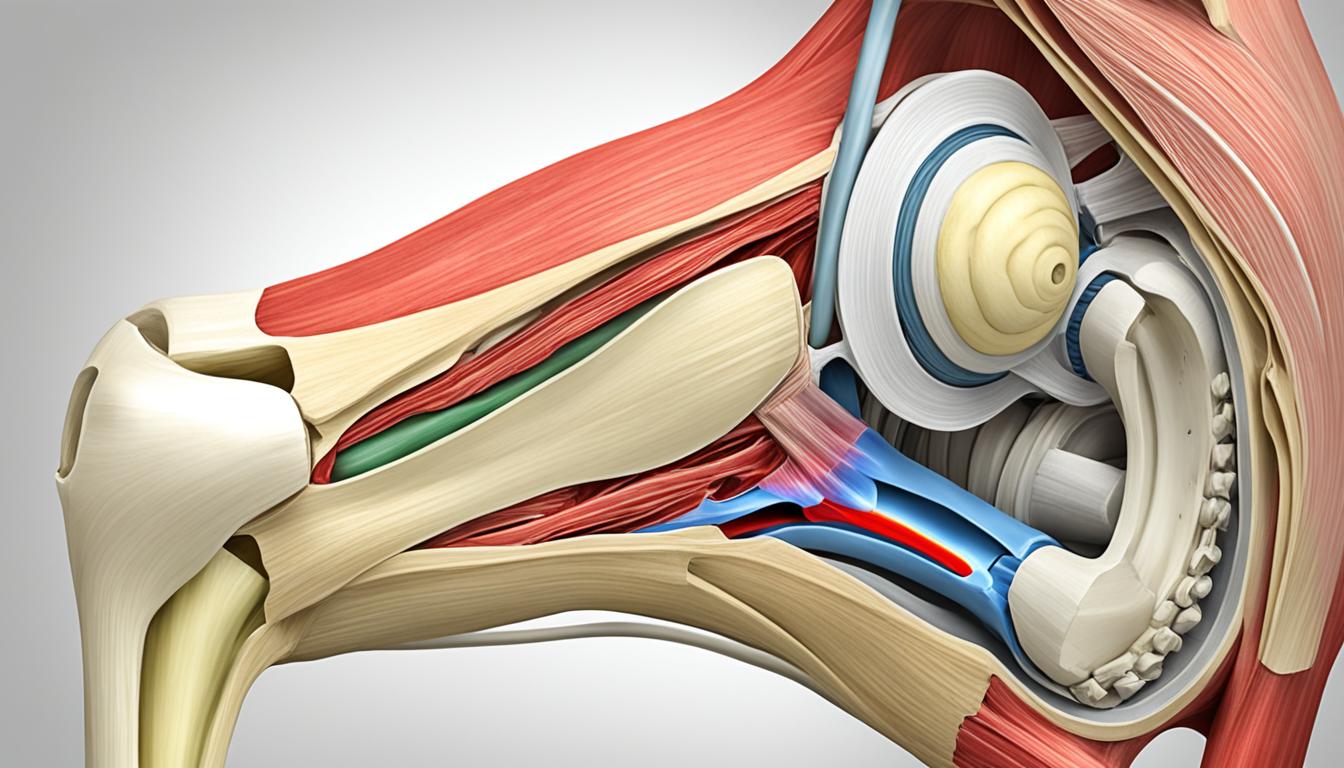
The patella, or kneecap, is a unique bone located in the anterior portion of the knee joint. It is composed of dense cancellous tissue covered by a thin compact lamina, providing it with strength and resilience. The patella has an anterior and posterior surface, as well as three borders and an apex. It is situated deep to the fascia lata and the tendon of the rectus femoris muscle, anterior to the knee joint.

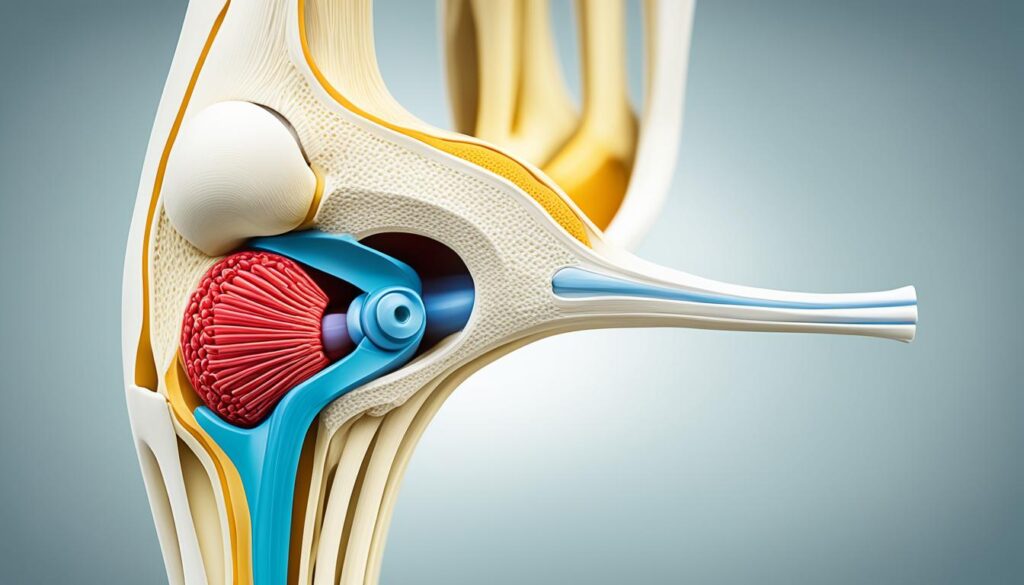
The structure of the patella is well-suited to its numerous functions. One of its primary roles is acting as an anatomic pulley for the quadriceps muscle. The quadriceps tendon attaches to the superior surface of the patella, while the patellar ligament attaches to the inferior surface. This unique arrangement allows the patella to increase the lever arm of knee extension, enhancing the strength and efficiency of the quadriceps muscle.
In addition to its pulley-like function, the patella also serves as a protective shield for deeper structures within the knee joint. It acts as a bony barrier, shielding the quadriceps tendon from frictional forces that can occur during knee movement. This protective function helps minimize wear and tear on the tendon and reduces the risk of injury.
The patella’s structure also contributes to knee torque during extension. By increasing the moment arm of the knee, the patella maximizes the rotational force generated by the quadriceps muscle, allowing for powerful knee extension. This rotational force is essential for activities such as running, jumping, and climbing stairs.
The quadriceps muscle, with its attachment to the patella, plays a crucial role in stabilizing the knee joint. It helps maintain proper alignment and tracking of the patella within the patellofemoral groove of the femur, ensuring smooth and efficient movement during knee flexion and extension.
Overall, the structure of the patella is intricately designed to support its various functions. From enhancing knee extension and quadriceps strength to providing protection and enhancing knee torque, the patella is a vital component of the knee joint’s biomechanics.
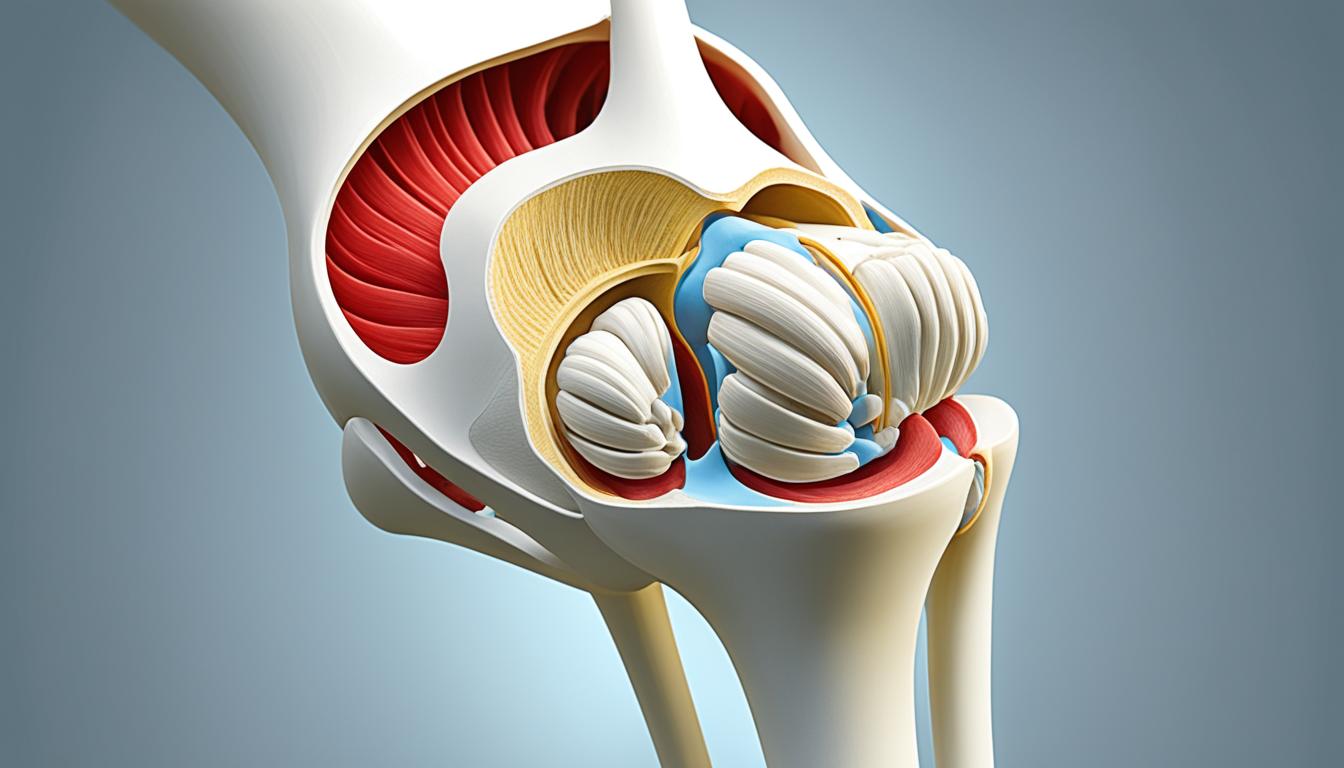
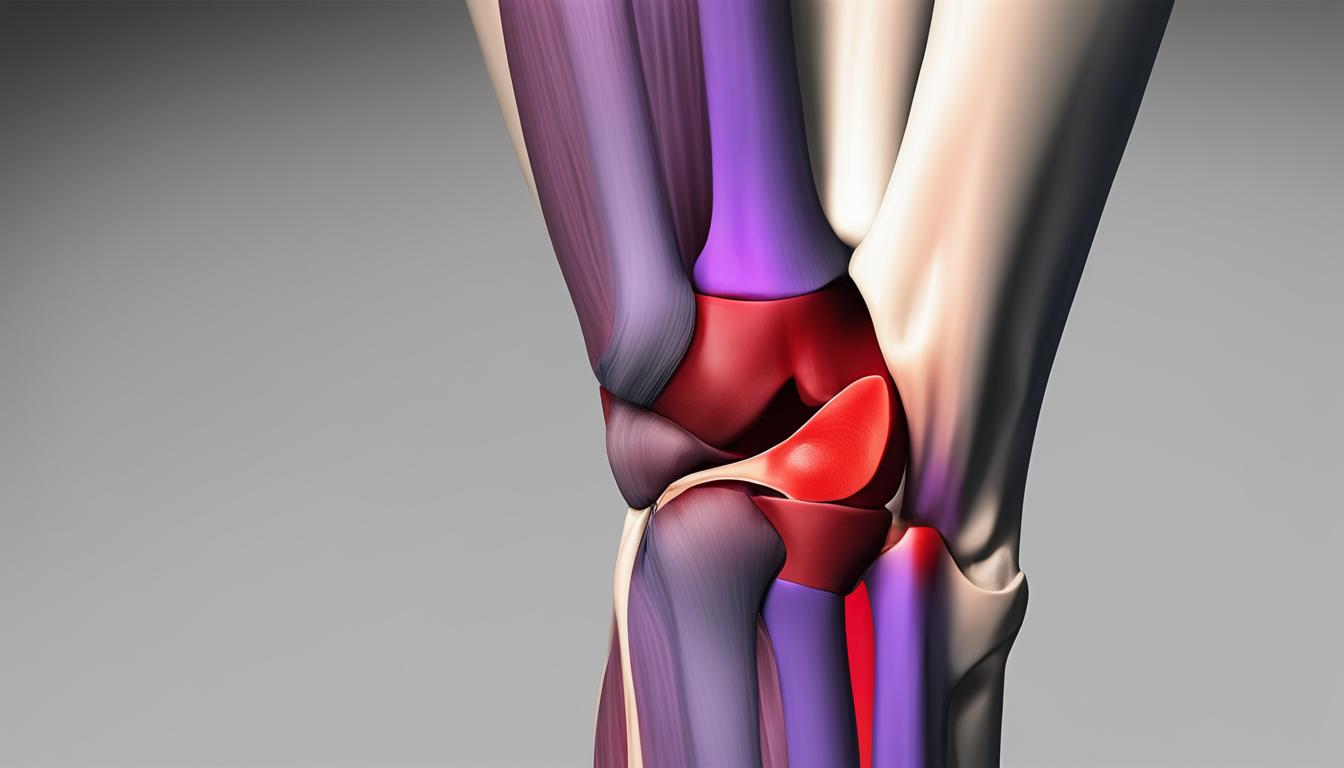
Articulation of the Patella
The patella plays a crucial role in the articulation of the knee joint. It forms the patellofemoral joint, where it articulates with the femur, specifically the femoral condyles. This joint allows for the smooth movement of the patella during knee flexion and extension.
The posterior surface of the patella is covered with a layer of articular cartilage. This cartilage serves as a cushion, dissipating the force exerted on the patellofemoral joint and reducing friction. It allows for easier gliding of the patella over the femur, ensuring smooth and pain-free movement.
The articulation surface of the patella consists of three facets on the posterior side and one facet on the anterior side. These facets interact with corresponding areas on the femur, creating a stable joint that supports various movements of the knee.
During tibiofemoral motion, the patella moves in multiple planes. It undergoes superior and inferior gliding as the knee extends and flexes. Additionally, it experiences medial and lateral gliding, accommodating the rotational component of knee movements.
As the knee flexes, the contact surface of the patella changes, distributing the joint forces over a larger area. This dynamic nature of the patellofemoral joint ensures optimal load distribution and helps prevent excessive stress on specific areas.
Clinical Relevance of the Patella
When it comes to the clinical aspects of the patella, there are two common conditions that can significantly impact this bone: patellar dislocation and patellar fractures. Patellar dislocation occurs when the patella displaces out of the patellofemoral groove, often due to a sudden twisting of the knee. This can cause intense pain and instability in the knee joint, leading to difficulties with mobility and daily activities.
On the other hand, patellar fractures can result from a sudden contraction of the quadriceps muscle or direct trauma to the bone. Fractures can vary in severity, from hairline cracks to complete breaks, and require immediate medical attention. These fractures can be incredibly painful and cause swelling, bruising, and limitations in knee movement.
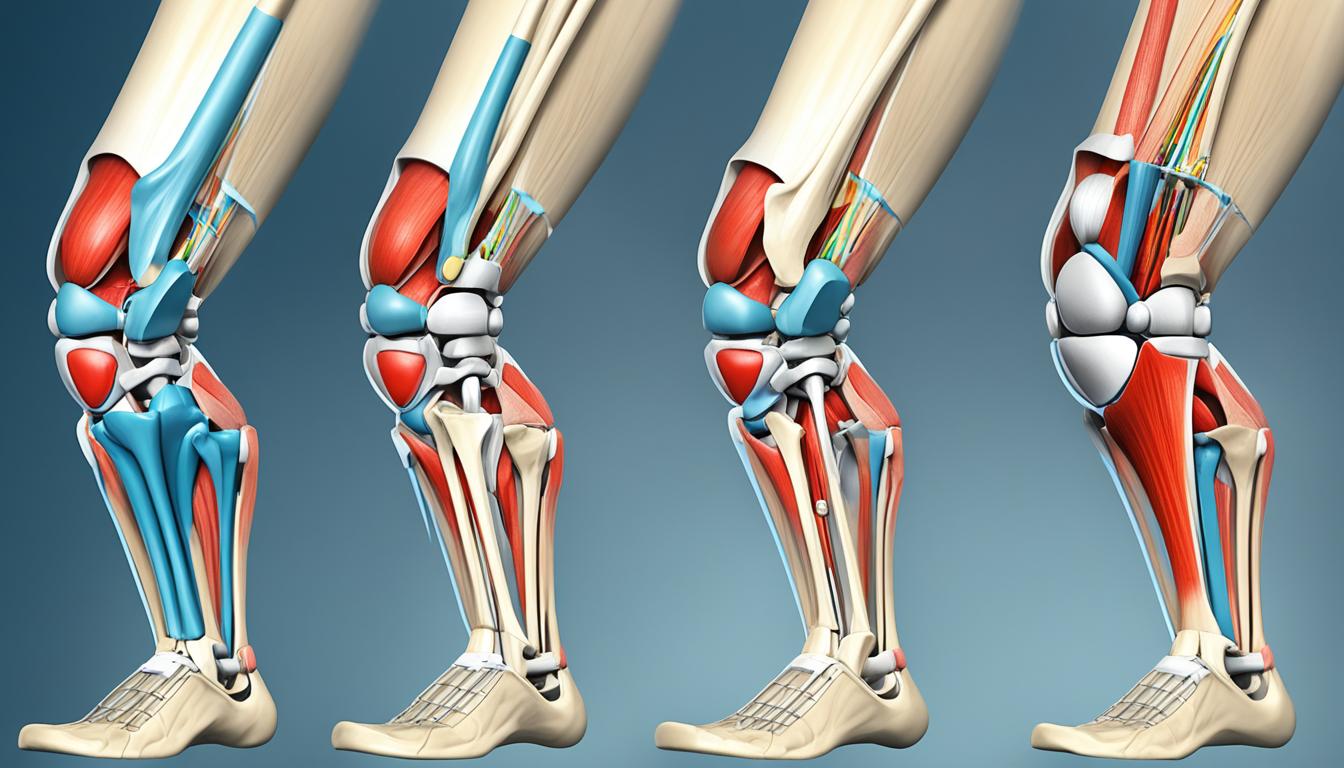
Treatment for patellar conditions depends on the specific case and may involve a combination of approaches. For less severe cases, knee-strengthening exercises can be prescribed to improve the stability and function of the patella. These exercises focus on strengthening the muscles around the knee, including the quadriceps, hamstrings, and glutes, to provide better support to the patella and reduce the risk of future dislocations or fractures.
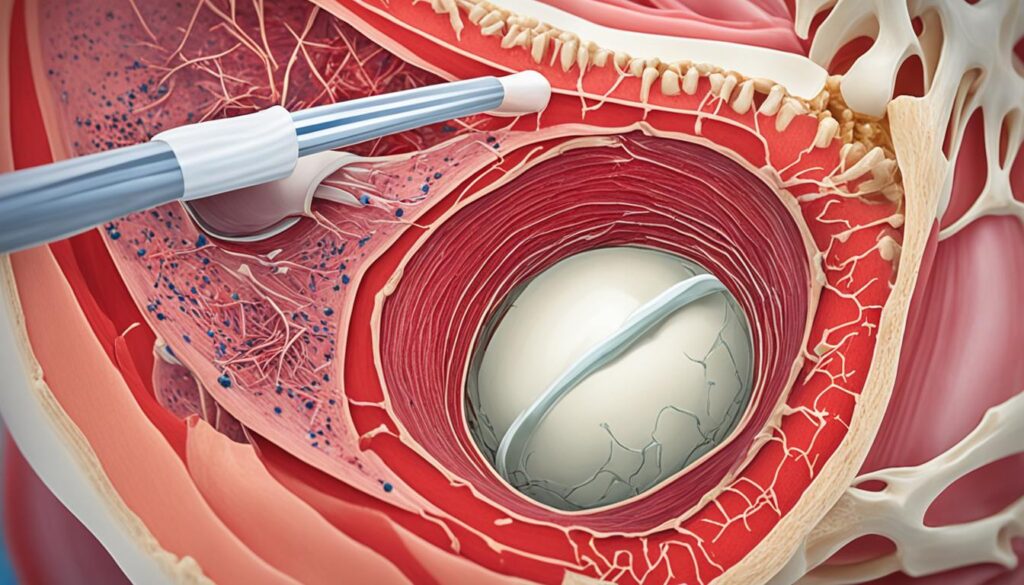
In more severe cases, medical interventions such as arthroscopy or realignment surgery may be necessary. Arthroscopy is a minimally invasive surgical procedure that uses a tiny camera and small incisions to diagnose and treat various knee conditions, including patellar dislocations and fractures. Realignment surgery, also known as patellar realignment, involves correcting the alignment of the patellar bone to restore normal movement and stability in the knee joint.
Knee-strengthening exercises play an integral role in the rehabilitation process following patellar conditions. These exercises not only help in restoring the strength and stability of the knee but also aid in preventing future injuries. Some examples of effective knee-strengthening exercises include:
- Squats: Perform squats by standing shoulder-width apart, lowering down as if sitting on a chair, and then returning to a standing position. This exercise targets the quadriceps, hamstrings, and glutes.
- Lunges: Step forward with one leg, bending both knees to lower the body. Return to the starting position and repeat with the other leg. Lunges target the quadriceps, hamstrings, glutes, and calves.
- Leg Press: Using a leg press machine, push a weighted sled away from your body until your legs are almost fully extended, and then slowly return to the starting position. This exercise primarily targets the quadriceps.
- Step-Ups: Step onto a raised platform using one leg, then step down and repeat with the other leg. Step-ups engage the quadriceps, hamstrings, glutes, and calves.
- Wall Sits: Stand with your back against the wall and lower your body until your thighs are parallel to the floor, as if sitting on an invisible chair. Hold this position for a set amount of time. Wall sits mainly work the quadriceps.
Remember to consult with a healthcare professional or a physical therapist before starting any exercise program, particularly if you have a history of patellar dislocation, fractures, or other knee-related conditions. They can provide personalized recommendations and ensure that the exercises are performed correctly and safely.
Through a combination of proper diagnosis, appropriate treatment, and targeted rehabilitation, individuals with patellar conditions can regain strength, stability, and function in their knees. It is crucial to seek timely medical attention and follow the recommended treatment plan to achieve the best possible outcomes.
Conclusion
The patella, or kneecap, holds great significance in the function of the knee joint and leg movement. As the largest sesamoid bone in the human body, it serves a vital role in enhancing the efficiency of the quadriceps muscle. By acting as an attachment point for the quadriceps tendon and the patellar ligament, the patella increases the extension capacity of the quadriceps muscle.
Furthermore, the patella plays a crucial role in knee stability. It increases the moment arm of the knee, contributing to the overall stability of the joint. This increased stability aids in leg movement and helps prevent potential injuries.
Understanding the structure and function of the patella is essential in diagnosing and treating patellar conditions. By recognizing the importance of the patella and its role in knee function, healthcare professionals can effectively manage patellar dislocations, fractures, and other related issues. Maintaining the health and integrity of the patella is crucial for overall knee health and optimal physical activity.
FAQ
What is the significance of the patella and its role in the knee joint?
The patella, also known as the kneecap, serves as an attachment point for muscles, increasing the extension capacity of the quadriceps. It acts as a bony shield, protects the quadriceps tendon, enhances quadriceps efficiency, and contributes to knee stability and leg movement.
What are some common conditions and disorders that affect the patella?
Common conditions and disorders affecting the patella include patellar dislocation, patellar subluxation, osteoporosis, knee pain (chondromalacia patella), and fractures.
What tests and imaging are used to assess the patella?
The most common test performed on the patella is the patella reflex test, which triggers an involuntary leg extension. Imaging tests, such as X-rays or MRI scans, may also be used to assess for patellar injuries or fractures.
What is the structure and function of the patella?
The patella is composed of dense cancellous tissue and serves as an anatomic pulley for the quadriceps muscle, increasing the lever arm of knee extension. It also protects the quadriceps tendon from frictional forces and contributes to knee torque during extension.
How does the patella articulate with the femur?
The patella articulates with the femur to form the patellofemoral joint. The posterior surface of the patella is covered with articular cartilage, which allows for smooth movement during knee flexion and extension.
What are some clinical conditions related to the patella?
Clinical conditions related to the patella include patellar dislocation, patellar fractures, and knee pain. Treatment may involve knee-strengthening exercises, manual techniques for improving range of motion, supportive braces or taping, or, in severe cases, arthroscopy or realignment surgery.
What is the overall significance and importance of the patella?
The patella plays a significant role in knee joint function and leg movement. Understanding its structure and function is essential for diagnosing and treating patellar conditions and maintaining overall knee health.