Welcome to our comprehensive guide on understanding knees osteoarthritis. In this article, we will provide you with valuable information about knee osteoarthritis, its causes, symptoms, and available treatment options. Whether you have recently been diagnosed with knee osteoarthritis or are simply looking to expand your knowledge, we are here to help!
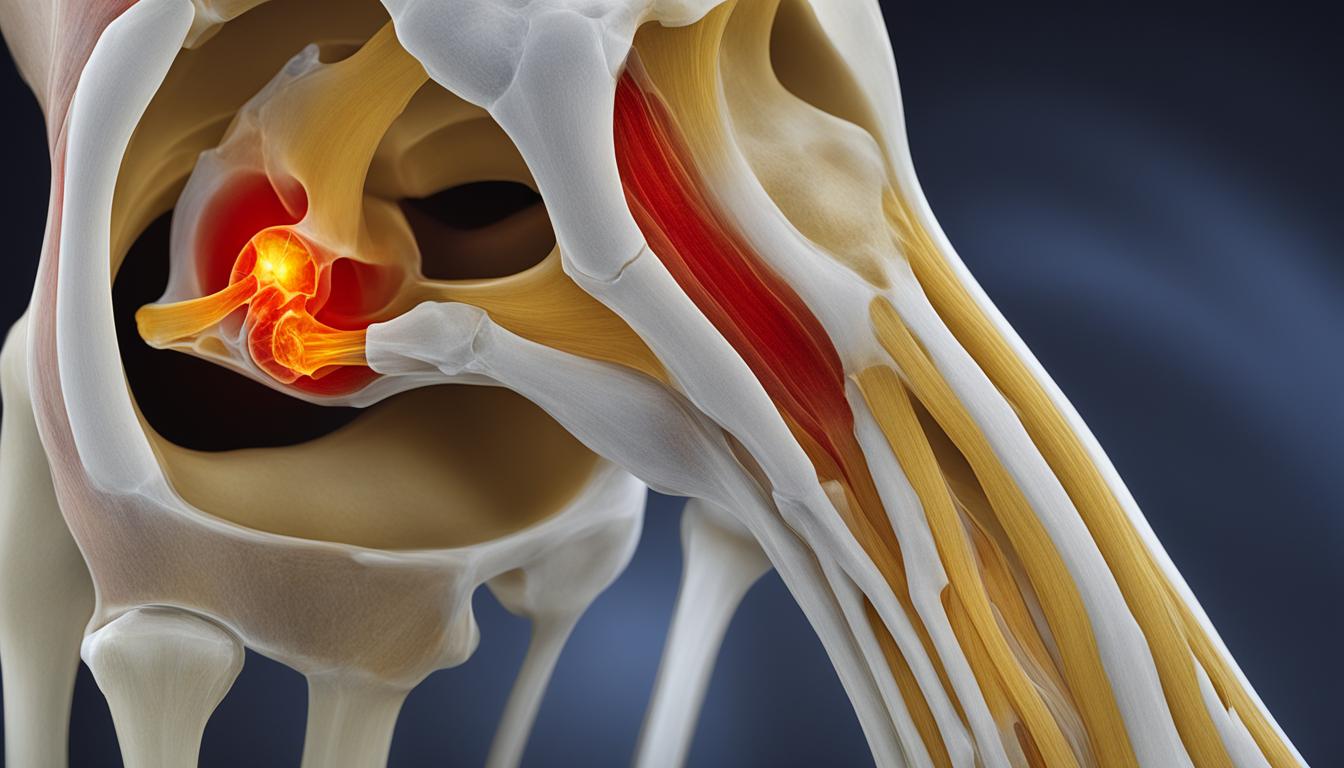
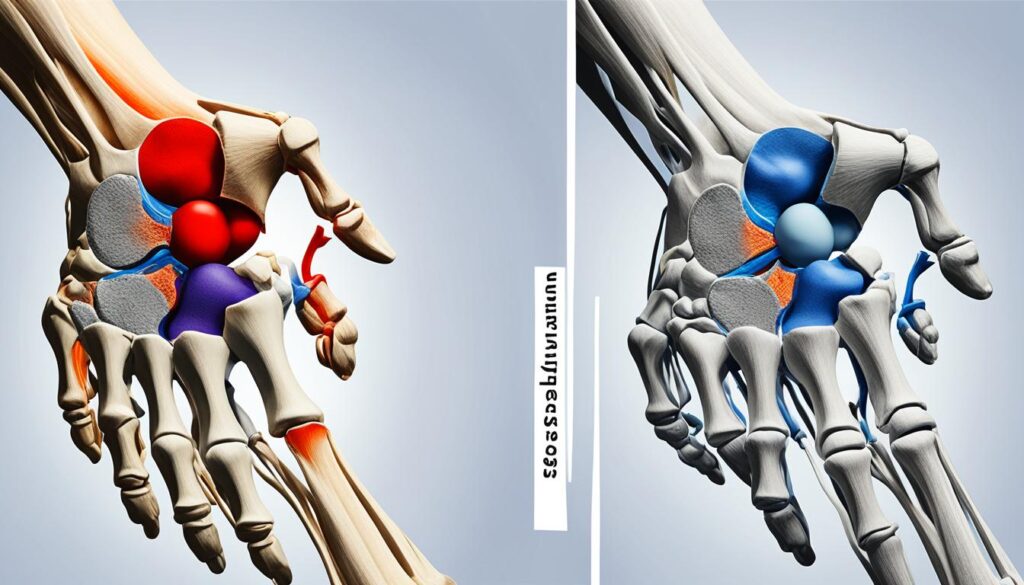
Knees osteoarthritis occurs when the cartilage in the knee joint gradually wears away, leading to joint inflammation and pain. It is a common form of arthritis that primarily affects adults over the age of 50. The exact cause of knee osteoarthritis is unknown, but several risk factors have been identified, including age, obesity, previous knee injuries, and genetic factors.
Through this guide, we aim to provide clarity and insight into this condition, so you can better understand its impact on your daily life and explore appropriate management options. Together, let us delve into the world of knee osteoarthritis and empower ourselves with the knowledge needed to navigate this condition.
Keep reading to learn more about the common causes of knee osteoarthritis and discover how it can be effectively managed.
Now, let’s dive deeper into the symptoms of knee osteoarthritis and explore how this condition manifests in individuals.
Symptoms of Knee Osteoarthritis
When it comes to knee osteoarthritis, the symptoms can vary from person to person. However, there are some common signs to look out for. The most prevalent symptoms include knee pain, stiffness, and swelling. Individuals with knee osteoarthritis often experience pain during activities like walking, climbing stairs, or getting up from a seated position.
The pain may be more pronounced in the morning or after periods of inactivity. In some cases, knee osteoarthritis can even lead to a limited range of motion, making it challenging to fully extend or bend the knee.

Dealing with knee pain can be frustrating, especially when it affects your daily activities. Understanding the symptoms of knee osteoarthritis is crucial in seeking appropriate treatment and management options. By identifying these symptoms early on, you can take proactive steps to alleviate pain, maintain mobility, and improve your overall quality of life.
Causes and Risk Factors of Knee Osteoarthritis
Knee osteoarthritis can be caused by a combination of factors. The most common causes include aging, previous knee injuries, overuse of the knee joint, and obesity.
As individuals age, the cartilage in the knee joint naturally wears down, increasing the risk of osteoarthritis. This gradual degeneration of the cartilage can lead to joint pain, inflammation, and reduced mobility.
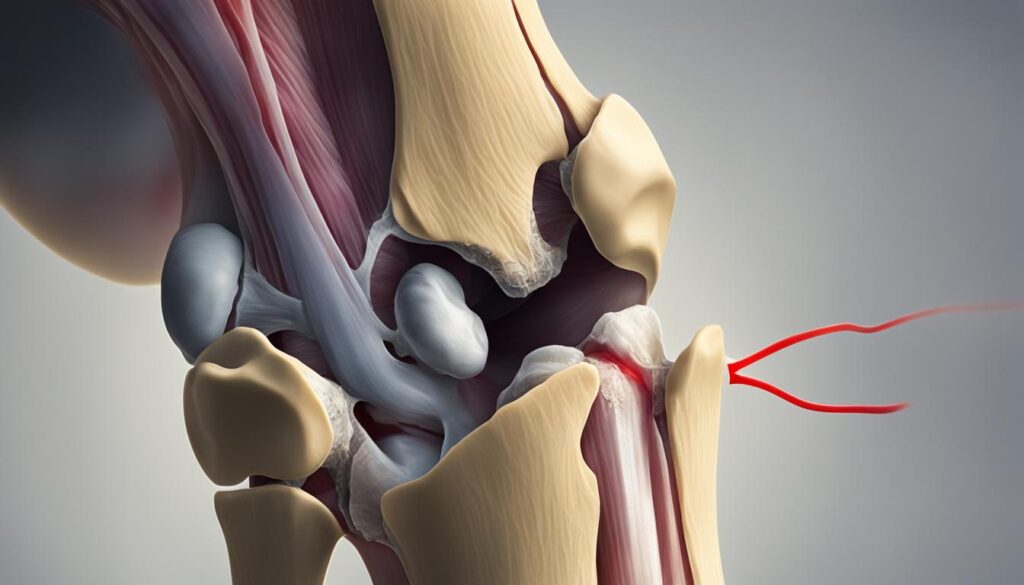
Previous knee injuries, such as fractures or ligament tears, can also contribute to the development of knee osteoarthritis. These injuries disrupt the normal structure of the knee joint, accelerating the breakdown of cartilage and leading to the onset of osteoarthritis.
Overuse of the knee joint is another common cause of knee osteoarthritis. Repetitive stress on the knee joint, often seen in occupations or sports that involve kneeling, squatting, or heavy lifting, can lead to joint degeneration over time. This repetitive motion puts strain on the cartilage, causing it to wear away more quickly.
Obesity is a significant risk factor for knee osteoarthritis. Excess body weight puts additional stress on the knee joints, increasing the wear and tear on the cartilage. This can lead to the onset and progression of osteoarthritis in overweight or obese individuals.
It’s important to note that while these factors increase the risk of knee osteoarthritis, they do not guarantee its development. Some individuals may have one or more risk factors but never develop the condition, while others may experience knee osteoarthritis without any identifiable risk factors.
Common Causes of Knee Osteoarthritis:
- Aging
- Previous knee injuries (fractures, ligament tears)
- Overuse of the knee joint
- Obesity

Understanding the causes and risk factors of knee osteoarthritis is important in preventing or managing the condition. By addressing modifiable risk factors, such as maintaining a healthy weight and avoiding excessive strain on the knee joints, individuals can reduce their chances of developing knee osteoarthritis or slow down its progression.
Treatment and Management of Knee Osteoarthritis
While there is no cure for knee osteoarthritis, there are various treatment options available to help manage the symptoms and slow the progression of the disease.
Non-surgical treatments play a crucial role in the management of knee osteoarthritis. Lifestyle modifications, such as weight management and regular exercise, can be effective in reducing pain and improving joint function. Maintaining a healthy weight helps to relieve stress on the knee joints, while exercise strengthens the muscles around the knee joint, providing added support and stability.
Physical therapy is another non-surgical treatment option that focuses on improving range of motion, reducing pain, and enhancing overall joint function. Physical therapists employ various techniques, such as manual therapy, therapeutic exercises, and modalities like heat or cold therapy, to alleviate symptoms and promote joint health.
Assistive devices, such as braces or canes, can also aid in managing knee osteoarthritis. Braces provide stability and support to the knee joint and can significantly reduce pain during weight-bearing activities. Canes help distribute weight and decrease pressure on the affected knee, relieving pain and improving mobility.
In more severe cases, medical interventions may be necessary. Corticosteroid injections help reduce inflammation and provide temporary relief from pain. These injections can be administered directly into the knee joint by a healthcare professional.
Viscosupplementation is another medical intervention used in the management of knee osteoarthritis. It involves the injection of a gel-like substance into the joint, which helps to lubricate and cushion the joint, reducing pain and improving mobility.
In cases where non-surgical treatments are not effective, surgical options may be considered. Knee arthroscopy is a minimally invasive surgical procedure that allows the healthcare professional to visualize and treat the internal structures of the knee joint. Joint replacement surgery, such as total knee replacement, is recommended for individuals with severe knee osteoarthritis where the joint has significant damage and conservative treatments have failed.
In summary, the treatment and management of knee osteoarthritis involve a combination of approaches tailored to the individual’s needs. Non-surgical options, including lifestyle modifications, physical therapy, and assistive devices, aim to alleviate symptoms and improve joint function. Medical interventions, such as corticosteroid injections or viscosupplementation, can provide additional relief. In more severe cases, surgical interventions may be necessary. Consulting with a healthcare professional is crucial in determining the most appropriate treatment plan for each individual.
Conclusion
Knee osteoarthritis is a common condition that affects many individuals, causing significant pain and mobility issues. Understanding the underlying causes, recognizing the symptoms, and exploring available treatment options are essential for effectively managing knee osteoarthritis and preventing further joint degeneration.
By making lifestyle changes, such as maintaining a healthy weight and participating in regular exercise, individuals can play an active role in managing their knee osteoarthritis. Engaging in low-impact physical activities, such as swimming or cycling, can help strengthen the muscles surrounding the knee joint and alleviate pain.
In addition to lifestyle modifications, it is crucial for individuals with knee osteoarthritis to consult with healthcare professionals. They can provide valuable guidance on non-surgical interventions, such as physical therapy, assistive devices like braces or canes, or medication to manage pain and inflammation.
For individuals with severe symptoms or advanced knee joint degeneration, surgical options like knee arthroscopy or joint replacement may be recommended. However, it is important to note that surgery is typically considered a last resort when conservative treatments have proven ineffective.
FAQ
What is knee osteoarthritis?
Knee osteoarthritis occurs when the cartilage in the knee joint gradually wears away, leading to joint inflammation and pain.
Who is most at risk for knee osteoarthritis?
Knee osteoarthritis primarily affects adults over the age of 50.
What are the symptoms of knee osteoarthritis?
Common symptoms of knee osteoarthritis include knee pain, stiffness, and swelling.
What can cause knee osteoarthritis?
Common causes of knee osteoarthritis include aging, previous knee injuries, overuse of the knee joint, and obesity.
Can knee osteoarthritis be cured?
There is no cure for knee osteoarthritis, but various treatments can help manage symptoms and slow the progression of the disease.
What are the treatment options for knee osteoarthritis?
Non-surgical treatments include lifestyle modifications, physical therapy, and the use of assistive devices. In more severe cases, medical interventions or surgical options may be recommended.
How can knee osteoarthritis be managed?
Knee osteoarthritis can be managed through lifestyle changes, non-surgical interventions, and consulting with healthcare professionals.