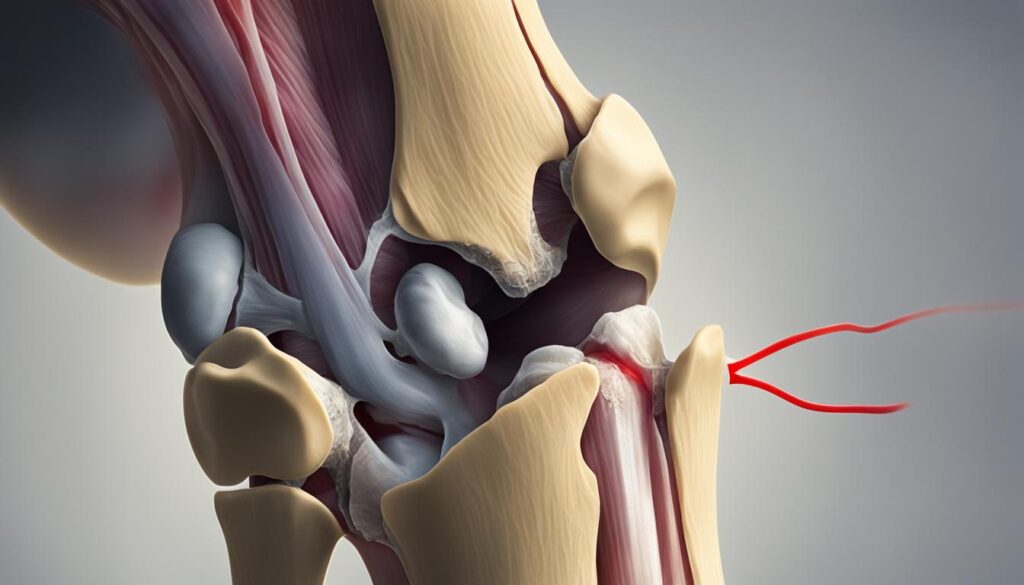
Welcome to our comprehensive guide on knee osteoarthritis. If you’re experiencing knee arthritis symptoms and wondering when to see a rheumatologist, you’ve come to the right place. Knee osteoarthritis can range from mild discomfort to severe pain, hindering your daily activities and overall quality of life. As experts in knee joint care, we understand the importance of timely intervention and effective management.
Osteoarthritis often develops years after an injury and can progress gradually. While your primary care doctor can make an initial assessment based on your symptoms, medical history, and physical examination, they may recommend further diagnostic tests like X-rays or blood tests to confirm the diagnosis. If your condition is not responding to standard treatment, they may refer you to a rheumatologist.
A rheumatologist specializes in treating inflammatory and joint diseases, including osteoarthritis. They can provide expert evaluation, diagnosis, and prescribe medications to relieve pain and other symptoms. When it comes to knee osteoarthritis, we are your trusted partners in providing comprehensive care, tailored to your specific needs. But when exactly should you consider consulting a rheumatologist?
Whether you need to see a rheumatologist for knee osteoarthritis depends on the stage of your disease and the severity of your symptoms. If you experience unrelenting pain, persistent or worsening symptoms despite treatment, an unclear diagnosis or underlying cause, or a significant impact on your quality of life, it’s time to seek specialized care. A rheumatologist can provide a comprehensive evaluation, perform diagnostic tests, and prescribe effective medications to manage your symptoms.
Stay tuned for the next sections of our guide, where we delve deeper into how a rheumatologist can help with knee osteoarthritis, other specialists involved in knee osteoarthritis management, and the importance of comprehensive care for optimal results. Don’t let knee osteoarthritis hold you back from enjoying life to the fullest. Consult with our experienced team today for personalized knee joint care.
When to See a Rheumatologist for Knee Osteoarthritis
Whether or not you need to see a rheumatologist for knee osteoarthritis depends on the stage of your disease and the severity of your symptoms. You may need to consult a rheumatologist if:
- Your pain is unrelenting: If you are experiencing persistent and unmanageable knee pain, a rheumatology specialist can provide expert evaluation and treatment options to help alleviate your discomfort.
- Your symptoms are persistent or worsening despite treatment: If your current treatment plan is not effectively managing your symptoms, a rheumatologist can assess your condition and recommend alternative approaches for knee osteoarthritis management.
- The diagnosis or underlying cause is unclear: If the cause of your knee pain or the specific type of knee osteoarthritis is unknown, a rheumatologist can conduct a comprehensive examination and diagnostic testing to determine the best course of action.
- Your condition is lowering your quality of life: If knee osteoarthritis is significantly impacting your daily activities, mobility, and overall well-being, seeking the expertise of a rheumatology specialist can help improve your knee pain relief and overall quality of life.
A rheumatologist can provide a comprehensive history and physical examination, perform diagnostic testing and imaging tests, and prescribe effective medications for knee pain treatment and relief. Their specialized knowledge in rheumatology and joint diseases enables them to tailor a treatment plan for your specific needs, helping you manage knee osteoarthritis and improve your knee joint care.
How a Rheumatologist Can Help with Knee Osteoarthritis
A rheumatologist plays a vital role in the management of knee osteoarthritis. With their expertise in inflammatory and joint diseases, they offer comprehensive evaluation, diagnosis, and treatment options tailored to your specific needs. Here’s how a rheumatologist can assist you in your knee osteoarthritis journey:
- Comprehensive Evaluation: By carefully examining your medical history, symptoms, and previous treatments, a rheumatologist can gain a thorough understanding of your condition. This evaluation helps them to determine the most appropriate management plan for your knee osteoarthritis.
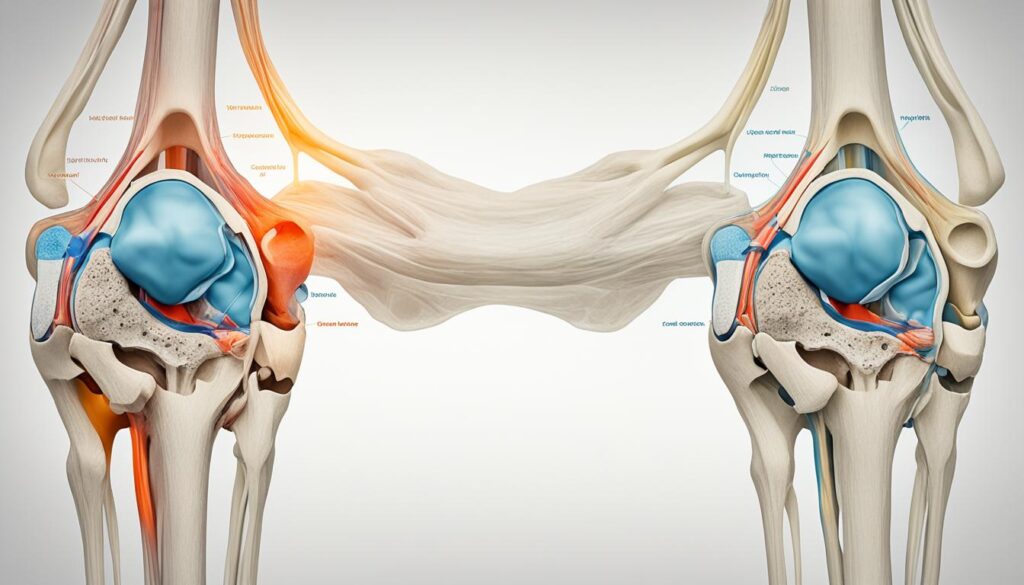
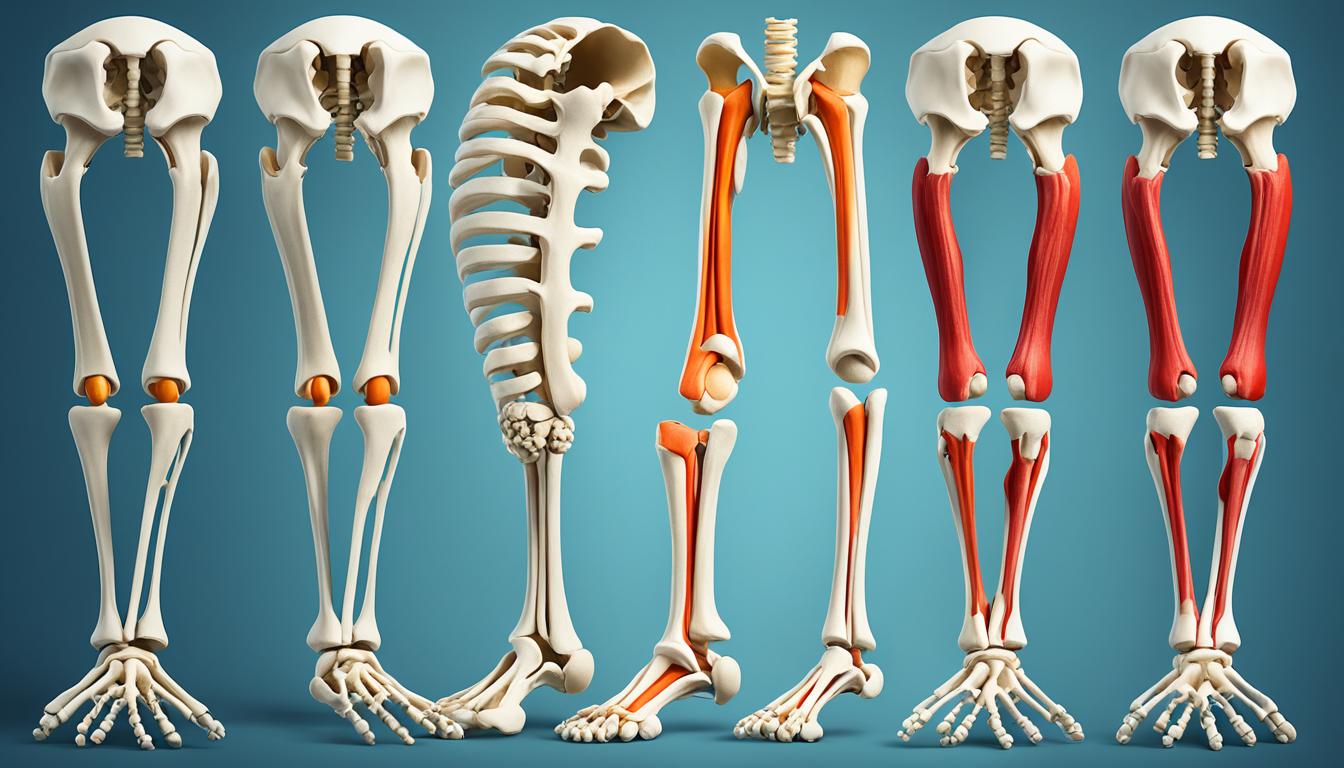
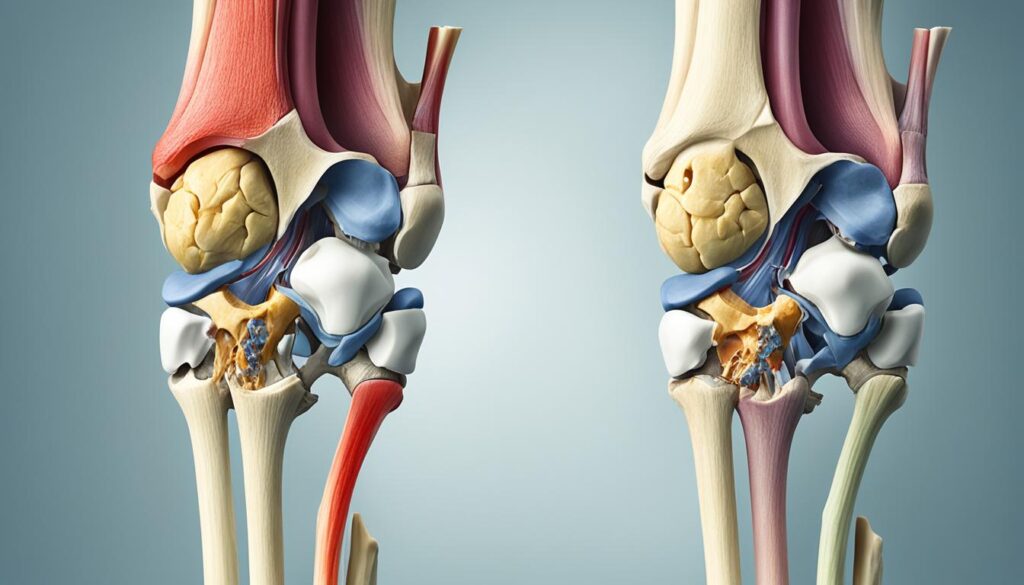
- Physical Exams: An essential part of the evaluation process involves conducting physical exams to assess your joint movement and stability. These exams enable the rheumatologist to evaluate the extent of the osteoarthritis, identify any joint deformities, and monitor the progression of the disease.
- Diagnostic Tests: To confirm the diagnosis of knee osteoarthritis and rule out other potential conditions, a rheumatologist may order diagnostic tests such as X-rays, MRI scans, or blood tests. These tests provide valuable insights into the severity of your osteoarthritis and guide the treatment approach.
- Pain and Inflammation Management: Rheumatologists have extensive knowledge of medications specific to managing knee osteoarthritis. They can prescribe pain relievers and anti-inflammatory drugs to help reduce pain, inflammation, and swelling in the knee joints.
- Lifestyle Guidance: In addition to medication, a rheumatologist can provide valuable guidance on lifestyle changes that can support knee joint care. This may include recommendations on exercise routines, weight management strategies, and modifications to daily activities to reduce stress on the knee joints.
- Physical Therapy Referrals: Recognizing the benefits of physical therapy in improving joint function and relieving pain, a rheumatologist can refer you to a physical therapist. These professionals can guide you through personalized exercises and therapies to strengthen the muscles around the knee joints and improve overall mobility.
- Collaboration with Other Specialists: If necessary, a rheumatologist can collaborate with other healthcare specialists to ensure comprehensive care for your knee osteoarthritis management. This may involve referring you to an orthopedic surgeon for further evaluation of surgical options or consultation with a pain management specialist for additional pain relief therapies.
By seeking the expertise of a rheumatologist, you gain access to a multidimensional approach to knee osteoarthritis management. Their in-depth knowledge, combined with personalized treatment plans, can help alleviate pain, improve joint function, and enhance your overall knee joint care.
Other Specialists for Knee Osteoarthritis Management
In addition to a rheumatologist, there are other specialists who can help with knee osteoarthritis management. Your primary care physician may recommend over-the-counter pain medication or prescribe pain treatment. A physical therapist can provide exercises for strength and pain relief. A pain management physician can offer pain therapies such as injections. If surgery is indicated, an orthopedic surgeon would be the best option. It’s important to work with a healthcare team that includes a primary care provider and specialists to ensure comprehensive and optimal care for your knee osteoarthritis.
By consulting different specialists, you can benefit from a tailored treatment plan that addresses your specific needs. Here’s an overview of the key specialists who may be involved in managing knee osteoarthritis:
| Healthcare Specialist | Role |
|---|---|
| Primary Care Physician | Initiates the diagnosis, prescribes initial treatments, and coordinates overall care. |
| Rheumatologist | Specializes in treating inflammatory and joint diseases, including osteoarthritis. Provides expert management and prescribes medications to relieve pain and other symptoms. |
| Physical Therapist | Designs exercise programs to improve strength, flexibility, and mobility, reducing pain and enhancing overall joint health. |
| Pain Management Physician | Offers interventional pain therapies such as injections or nerve blocks to provide targeted pain relief. |
| Orthopedic Surgeon | Performs surgical interventions, such as knee replacement or arthroscopy, when conservative treatments have been exhausted. |
Collaborating with these specialists and following their recommendations can significantly improve your knee pain treatment and overall quality of life. Together, they can provide comprehensive and optimal care to manage your knee osteoarthritis.
Conclusion
Knee osteoarthritis is a common condition that can cause significant discomfort and impact your quality of life. However, with the help of a rheumatologist and other healthcare specialists, you can effectively manage the symptoms and improve your knee joint care.
When you experience persistent or worsening knee arthritis symptoms, seeking medical assistance is crucial. A rheumatologist can provide expert evaluation, diagnosis, and personalized treatment options based on your specific condition. They can design a comprehensive treatment plan that may include medication, physical therapy, and lifestyle modifications.
By following the recommended treatment plan, you can find relief from knee pain and improve your overall knee osteoarthritis management. It is important to consult with your healthcare team regularly for ongoing management and follow-up appointments to ensure that your treatment remains effective and tailored to your needs.
Remember, the journey to managing knee osteoarthritis begins with seeking the help of a rheumatologist and taking proactive steps for your knee joint care. With their expertise and the support of other healthcare professionals, you can live a more comfortable and active life with this condition.
FAQ
What are the symptoms of knee arthritis?
Symptoms of knee arthritis include pain, stiffness, swelling, and decreased range of motion in the affected knee.
When should I see a rheumatologist for knee osteoarthritis?
You should consider seeing a rheumatologist for knee osteoarthritis if your symptoms are persistent or worsening despite treatment, if your pain is unrelenting, if the diagnosis or underlying cause is unclear, or if your condition is lowering your quality of life.
How can a rheumatologist help with knee osteoarthritis?
A rheumatologist can provide a comprehensive evaluation of your medical history and symptoms, perform physical exams and diagnostic tests, prescribe medications to reduce pain and inflammation, recommend lifestyle changes, and provide guidance on physical therapy exercises to improve joint function.
Besides a rheumatologist, are there other specialists who can help with knee osteoarthritis management?
Yes, other specialists who can help with knee osteoarthritis management include primary care physicians who can prescribe pain treatment, physical therapists who can provide exercises for strength and pain relief, pain management physicians who can offer pain therapies such as injections, and orthopedic surgeons who can perform necessary surgeries.
How can I effectively manage knee osteoarthritis?
Knee osteoarthritis can be effectively managed by consulting with a rheumatologist or other specialists, following a comprehensive treatment plan that may include medication, physical therapy, and lifestyle modifications, and regular communication and follow-up with your healthcare team.