Knee pain can be a debilitating condition that affects many individuals. Whether it’s due to an injury, arthritis, or other underlying causes, finding the right doctor is crucial for effective treatment. In this article, we will explore the key aspects of understanding knee pain, choosing the right doctor, diagnostic procedures, and treatment options.
Key Takeaways
- Understanding the anatomy of the knee is essential in identifying the source of knee pain.
- Common causes of knee pain include injuries, arthritis, and overuse.
- Finding a knee pain specialist who is experienced in treating your specific condition is important for effective care.
- Imaging tests such as X-rays and MRIs can help diagnose the cause of knee pain.
- Rehabilitation and physical therapy play a crucial role in the recovery process after knee surgery.
Understanding Knee Pain

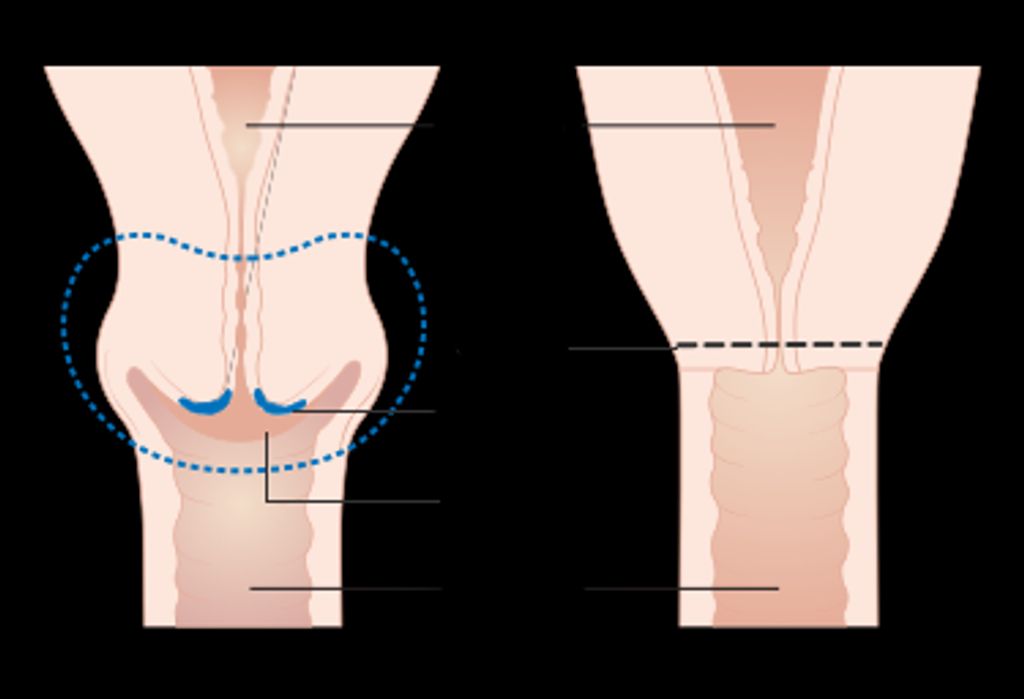
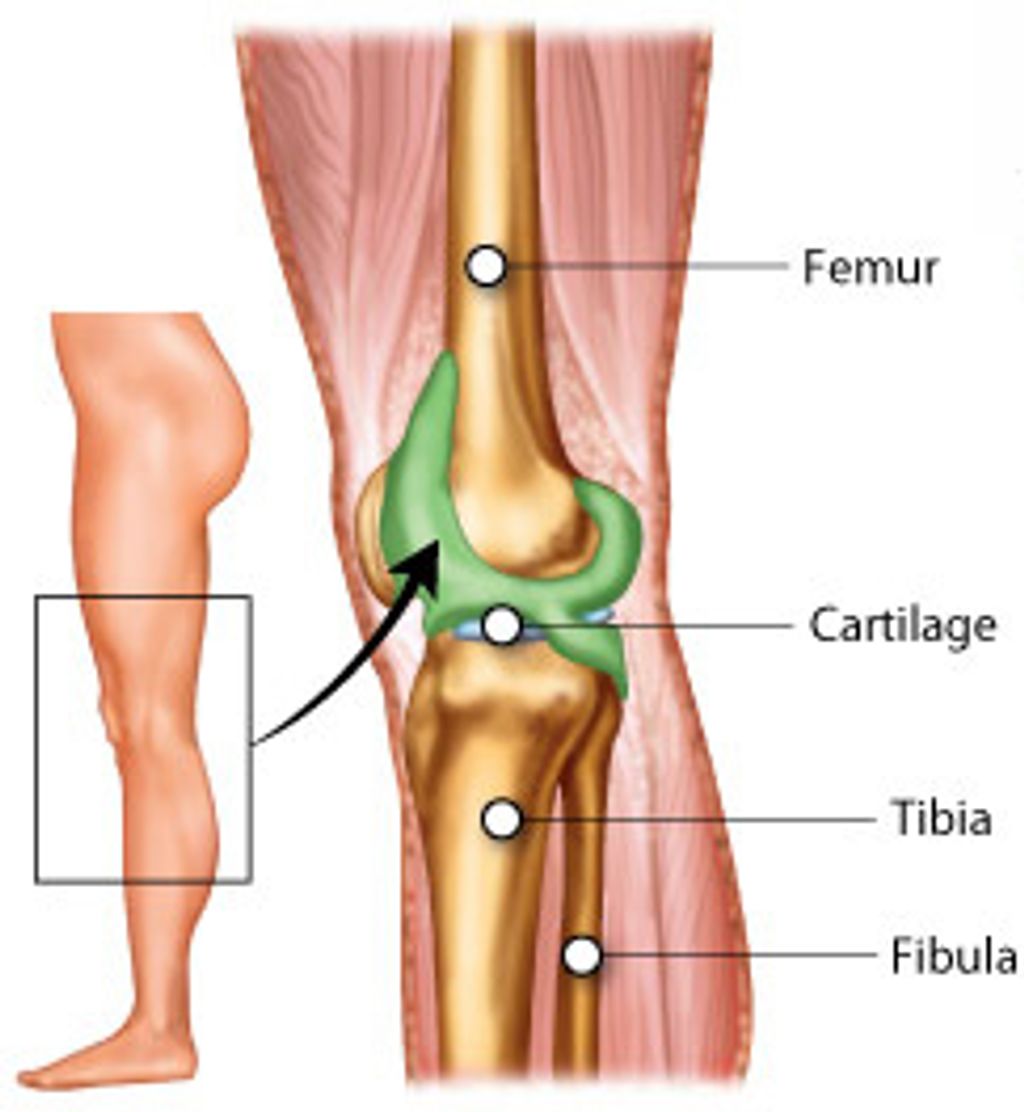
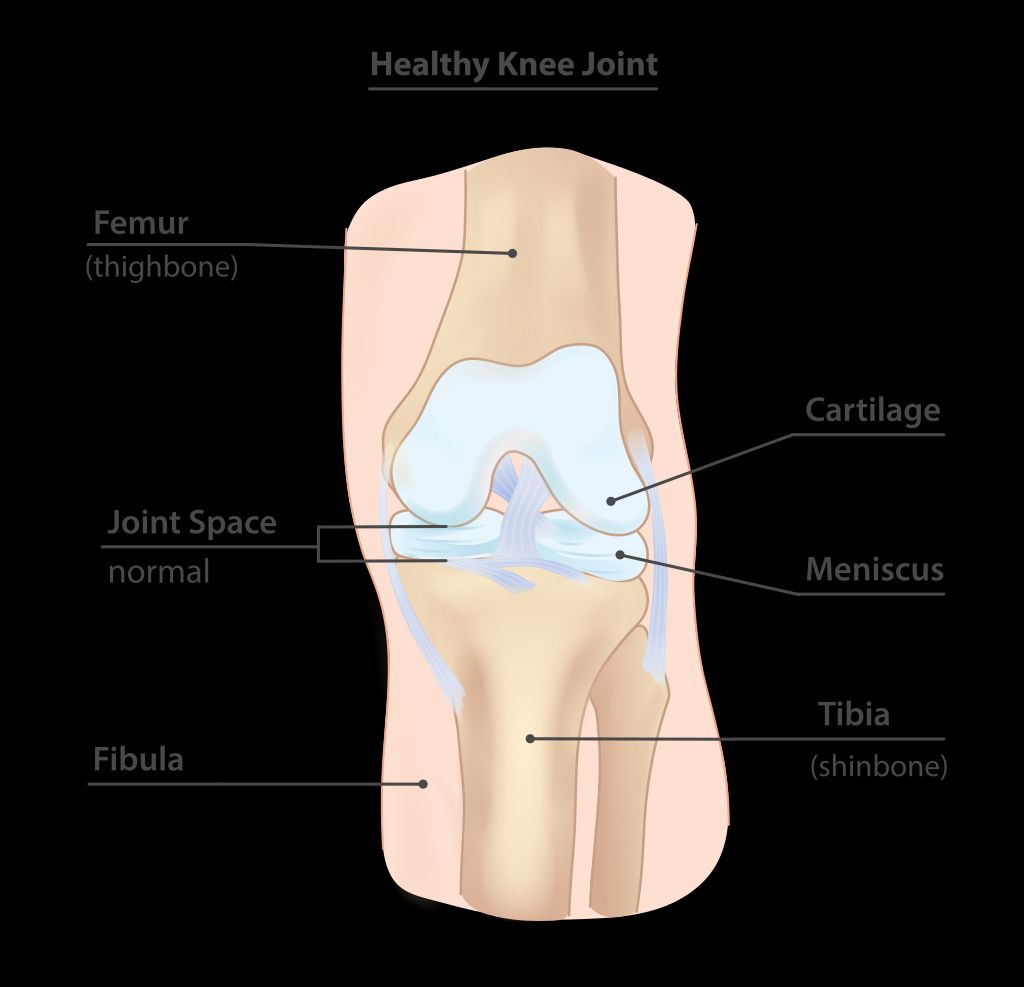
Anatomy of the Knee
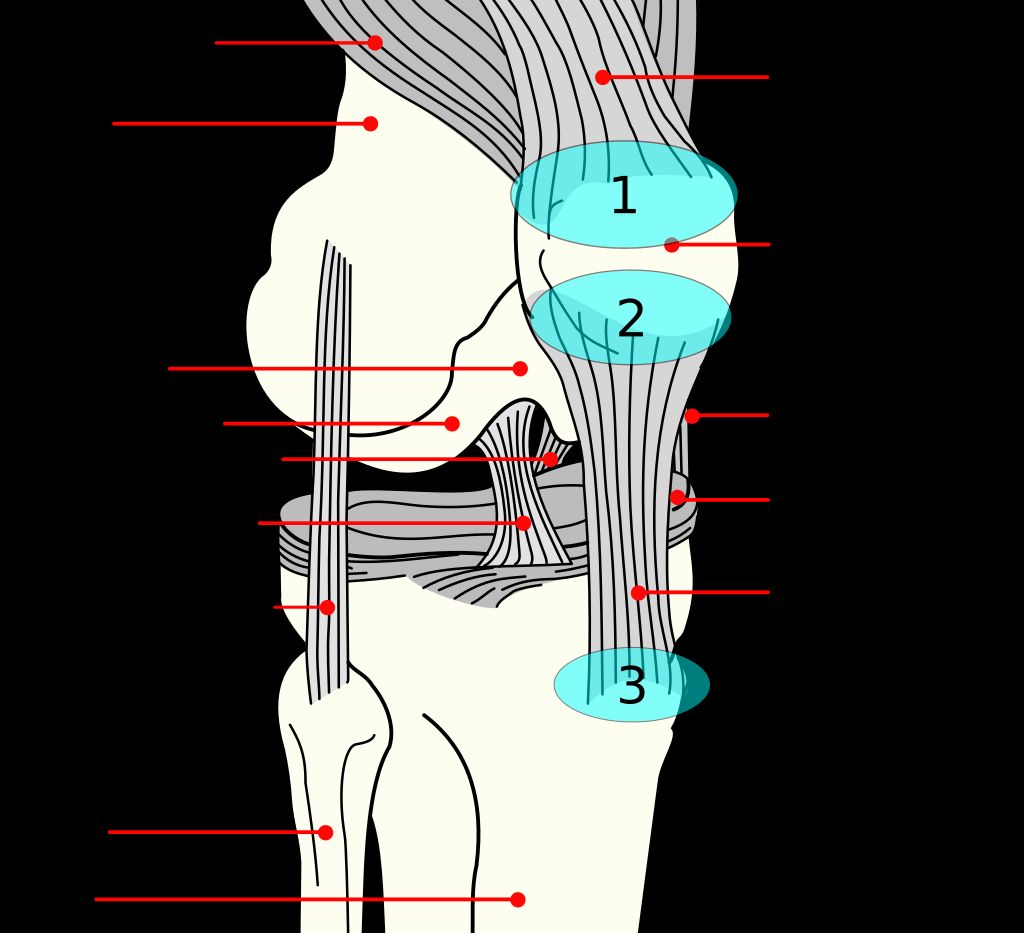
When we consider the complexity of the human body, the knee is a remarkable structure. It’s not just a simple hinge joint; it’s a sophisticated system that allows for a wide range of motion while supporting the body’s weight. The knee comprises four main components: bones, cartilage, ligaments, and tendons.
The bones form the framework and include the femur (thigh bone), tibia (shin bone), and patella (kneecap). The cartilage, particularly the meniscus, acts as a cushion and helps the bones glide smoothly over each other. Ligaments connect bones to bones, providing stability, while tendons connect muscles to bones, allowing us to move our legs with ease.
Understanding the anatomy of the knee is crucial for identifying the source of pain and determining the appropriate treatment. Here’s a quick overview of the key structures:
- Femur: The upper leg bone that articulates with the knee.
- Tibia: The lower leg bone forming the lower part of the knee joint.
- Patella: Also known as the kneecap, it protects the knee joint.
- Meniscus: Two crescent-shaped cartilage pieces that cushion and stabilize the knee.
- Ligaments: Including the ACL, PCL, MCL, and LCL, they provide knee stability.
- Tendons: Such as the patellar tendon, they connect muscles to the bones.
Remember, maintaining knee health is essential for mobility and overall well-being. Regular exercise and avoiding excessive strain can help preserve knee function.
Common Causes of Knee Pain
Understanding the common causes of knee pain is crucial in identifying the underlying issues. In many cases, overuse or injury to the knee can lead to pain and discomfort. Additionally, conditions such as osteoarthritis and rheumatoid arthritis are known to contribute to knee pain. It’s important to note that factors like age, weight, and activity level can also play a significant role in the development of knee pain. Understanding these causes can help us make informed decisions about seeking medical attention and treatment for our knee pain.
Types of Knee Pain
We recognize that knee pain can manifest in various forms, each with its own set of challenges and implications for treatment. Broadly, knee pain can be categorized into acute, subacute, and chronic, depending on the duration and onset of symptoms. Acute knee pain often results from injuries such as ligament tears or fractures, and typically demands immediate attention.
- Acute Knee Pain
- Subacute Knee Pain
- Chronic Knee Pain
For instance, chronic knee pain may develop over time due to conditions like osteoarthritis or tendinitis, and may require a different approach to management. It’s essential to identify the type of knee pain as it guides the subsequent diagnostic and therapeutic strategies.
Tip: Always consult with a healthcare professional to accurately diagnose the type of knee pain you’re experiencing, as this will significantly influence the effectiveness of your treatment plan.
Choosing the Right Doctor

Qualities to Look for in a Knee Pain Doctor
When we seek medical attention for knee pain, it’s crucial to find a doctor who not only has the expertise but also possesses certain qualities that can make a significant difference in our treatment experience. One of the primary qualities to look for is empathy. An empathetic doctor can provide a level of comfort and understanding that is invaluable during treatment. Additionally, we should look for a doctor who is communicative and transparent about diagnoses and treatment plans.
Another key quality is the doctor’s commitment to staying abreast of the latest medical advancements in knee pain treatment. This ensures that we have access to the most current and effective treatment options. Moreover, a good knee pain doctor should have a proven track record of success with patients suffering from similar conditions.
Here’s a list of qualities that are important when choosing a knee pain doctor:
- Empathy and patient comfort
- Clear communication and transparency
- Up-to-date with medical research
- Successful patient outcomes
Remember, the relationship with your knee pain doctor is a partnership. It’s essential to choose someone who you feel comfortable with and who supports your journey to recovery.
Finding a Specialist
When we embark on the journey to find the best knee pain specialist, it’s crucial to consider the type of doctor that will best suit our needs. Orthopedic surgeons are often the go-to specialists for knee pain, as they focus on the musculoskeletal system. However, depending on the cause and severity of the knee pain, we might also consider seeing a rheumatologist for inflammatory conditions, or a physiatrist for rehabilitation and pain management.
To streamline our search, we can create a list of potential specialists based on referrals, insurance coverage, and proximity. Here’s a simple process we can follow:
- Gather referrals from primary care physicians, friends, or family members.
- Verify the doctor’s credentials and specialization through medical boards or professional directories.
- Check if the specialist is covered by our insurance plan.
- Consider the location of the clinic for convenience and accessibility.
Tip: Always verify the specialist’s experience with your specific knee condition before scheduling an appointment.
Once we have a list of potential specialists, we can further narrow down our choices by considering factors such as the doctor’s communication style, patient reviews, and the range of treatments they offer. It’s important to feel confident in our choice, as the right specialist will not only provide expert care but also guide us through the recovery process with compassion and understanding.
Evaluating Doctor’s Experience
When evaluating a doctor’s experience, we prioritize patient outcomes as a key metric. Our focus is on understanding the success rates of previous treatments and the overall satisfaction of patients under the doctor’s care. This data is crucial in making informed decisions about the doctor’s expertise and ability to deliver effective treatments.
In addition, we consider the number of procedures performed by the doctor, as it provides insight into their level of experience and proficiency in handling various knee pain conditions. This quantitative measure offers valuable information about the doctor’s familiarity with different treatment modalities and their capability to address complex cases.
Furthermore, it is important to note that the length of practice is a significant factor in evaluating a doctor’s experience. A doctor with extensive experience is likely to have encountered a wide range of knee pain scenarios, thereby honing their diagnostic and treatment skills over time.
It is advisable to inquire about the doctor’s experience with specific knee pain conditions, as specialized expertise can greatly impact the quality of care and treatment outcomes.
Diagnostic Procedures
Physical Examination
When we seek medical attention for knee pain, the initial step is often a thorough physical examination. During this assessment, the doctor will evaluate the knee’s range of motion, stability, strength, and overall alignment. They may also check for signs of swelling, tenderness, or redness which can indicate inflammation or injury.
Palpation is a key component of the physical examination, where the doctor applies gentle pressure to different parts of the knee to identify any abnormalities or pinpoint the source of pain. It’s important to provide accurate feedback during this process to help the doctor make a correct diagnosis.
Here’s a brief overview of what to expect during a physical examination:
- Observation of gait and posture
- Assessment of joint mobility
- Palpation of the knee structure
- Evaluation of ligament integrity
- Testing for meniscal damage
Tip: Be prepared to discuss the history of your knee pain, including any specific movements or activities that exacerbate the discomfort. This information is crucial for a comprehensive evaluation.
Imaging Tests for Knee Pain
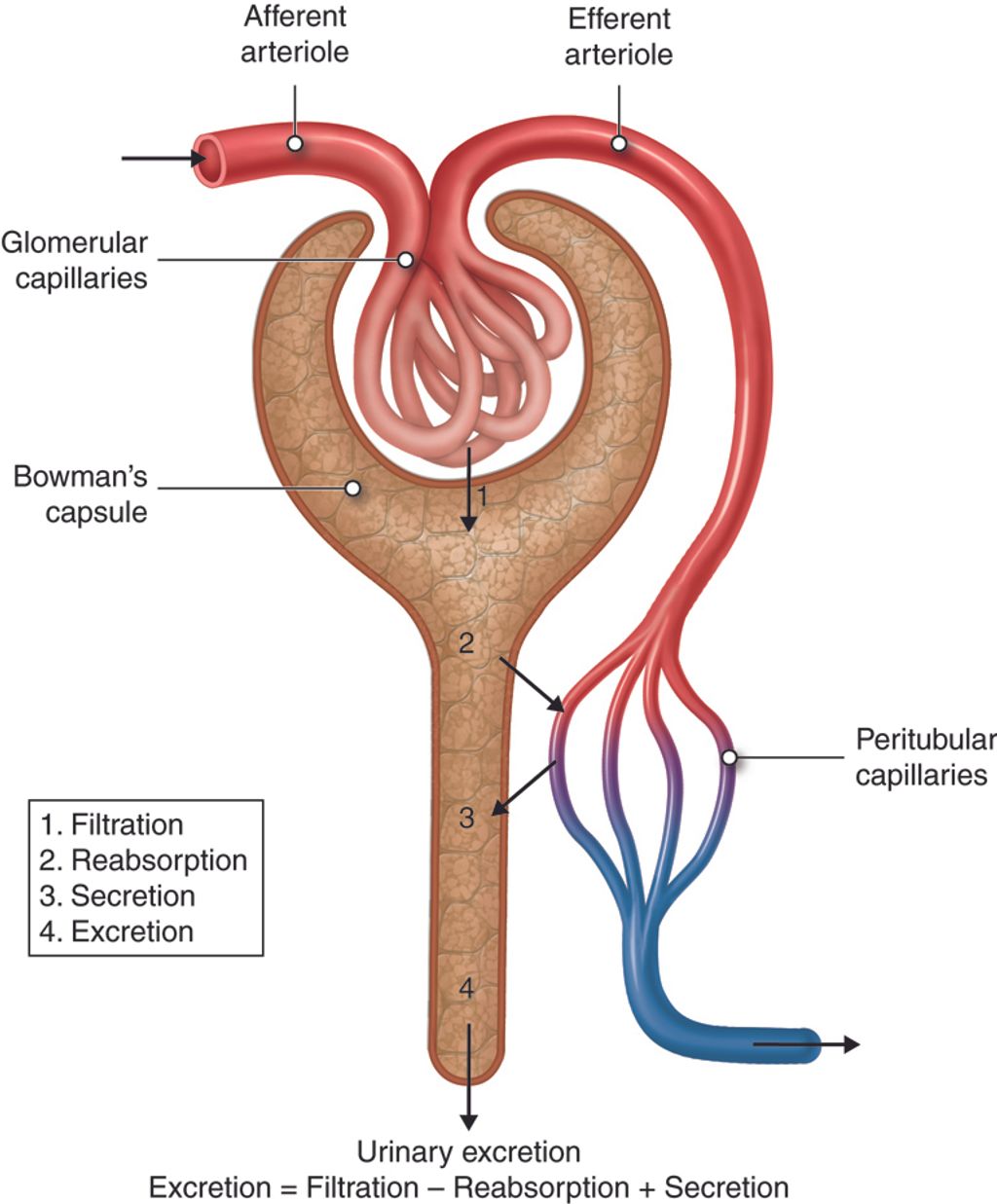
After undergoing imaging tests for knee pain, we will receive a comprehensive report detailing the condition of our knee joint. This report will include information about any abnormalities, such as fractures, dislocations, or signs of arthritis. Additionally, the report may provide quantitative data on the extent of tissue damage, which can help guide the treatment plan. We can expect the report to be presented in a clear and organized manner, allowing us to understand the findings easily. If we have any questions or need further clarification, we should not hesitate to discuss the report with our doctor.
Laboratory Tests for Knee Pain
Laboratory tests play a crucial role in diagnosing the underlying causes of knee pain. These tests provide valuable insights into the presence of inflammatory markers, infection, and other systemic conditions that may contribute to knee discomfort. Interpreting the results of these tests requires a comprehensive understanding of the patient’s medical history and current symptoms. It is important to note that laboratory tests alone may not provide a definitive diagnosis, but they are an essential component of the diagnostic process. Collaboration between the patient, the doctor, and the laboratory professionals is key to ensuring accurate and meaningful results.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
Treatment Options

Non-Surgical Treatments
Non-surgical treatments for knee pain are often the first line of defense in managing the condition. Physical therapy plays a crucial role in strengthening the muscles around the knee and improving flexibility. Additionally, anti-inflammatory medications may be prescribed to reduce pain and swelling. It’s important to note that these treatments are most effective when combined with lifestyle modifications, such as weight management and activity modification.
- Implementing a table for presenting structured, quantitative data is not applicable in this context.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
- A personalized exercise program tailored to the individual’s needs
- Use of supportive devices such as knee braces or orthotics
- Application of ice or heat therapy to alleviate discomfort
It is essential to consult a qualified healthcare professional before starting any new treatment regimen. Each individual’s condition is unique, and personalized care is crucial for effective management of knee pain.
Surgical Interventions
When conservative treatments for knee pain do not yield the desired results, we may consider surgical interventions. These procedures are aimed at relieving pain, restoring function, and improving quality of life. The decision to proceed with surgery is made carefully, taking into account the individual’s specific condition, age, activity level, and overall health.
Surgical options vary depending on the diagnosis and severity of knee pain. Common surgeries include arthroscopy, partial or total knee replacement, and ligament reconstruction. Each procedure has its own set of indications, risks, and recovery times.
Tip: Always discuss the potential benefits and risks of surgery with your doctor to make an informed decision.
Here is a list of surgical interventions commonly performed for knee pain:
- Arthroscopic surgery to repair or remove damaged cartilage
- Partial knee replacement for cases where damage is limited to a particular area
- Total knee replacement for severe arthritis or damage
- ACL reconstruction to repair a torn anterior cruciate ligament
- Osteotomy to realign bones and relieve pressure on the knee joint
Rehabilitation and Recovery
After undergoing knee surgery, the journey towards regaining full mobility and strength is paramount. We emphasize the importance of a structured rehabilitation program, which is tailored to the individual needs of each patient. Rehabilitation is not a one-size-fits-all process; it requires careful planning and adjustment based on the patient’s progress.
Recovery times can vary, and it’s crucial to set realistic goals and milestones. A typical rehabilitation program may include the following stages:
- Initial rest and pain management
- Gradual increase in movement and weight-bearing activities
- Strength training and conditioning
- Functional exercises to restore normal knee function
Tip: Always follow the guidance of your rehabilitation professionals to avoid setbacks and ensure the best outcome.
Monitoring progress is a key component of successful recovery. Patients should expect regular evaluations with their healthcare team to ensure that the rehabilitation plan remains effective and responsive to their healing journey.
Conclusion
In conclusion, finding the best knee pain doctor near you is a crucial step in managing and treating knee pain effectively. By considering factors such as expertise, experience, and patient reviews, individuals can make informed decisions when seeking medical care for their knee pain. It is essential to prioritize one’s health and well-being by seeking out a qualified and reputable knee pain doctor who can provide personalized and effective treatment options.
Frequently Asked Questions
What are the common symptoms of knee pain?
Common symptoms of knee pain include swelling, stiffness, redness, warmth, weakness, and instability in the knee.
How can I prevent knee pain?
To prevent knee pain, it’s important to maintain a healthy weight, exercise regularly, wear proper footwear, avoid sudden increases in physical activity, and use proper techniques during sports and exercise.
What are the non-surgical treatment options for knee pain?
Non-surgical treatment options for knee pain include physical therapy, medications, injections, bracing, and lifestyle modifications such as weight management and activity modification.
What are the common imaging tests used to diagnose knee pain?
Common imaging tests for diagnosing knee pain include X-rays, MRI (Magnetic Resonance Imaging), CT (Computed Tomography) scans, and ultrasound.
How long does it take to recover from knee surgery?
Recovery time from knee surgery varies depending on the type of surgery and individual factors. It can range from a few weeks to several months, and rehabilitation plays a crucial role in the recovery process.
What should I look for in a specialist for knee pain treatment?
When looking for a specialist for knee pain treatment, consider their experience, expertise in knee-related conditions, communication style, and their approach to personalized treatment plans.