Knee injuries can be debilitating and may require careful rehabilitation and exercise protocols to ensure safe and effective recovery. Understanding the common types, causes, and risk factors for knee injuries is crucial in developing an appropriate exercise plan. Additionally, rehabilitation and recovery play a significant role in the healing process. In this article, we will explore the key takeaways from each section to provide valuable insights into safe and effective knee injury exercises.
Key Takeaways
- Understanding the common types, causes, and risk factors for knee injuries is essential for developing an appropriate exercise plan.
- Rehabilitation and recovery are crucial for the healing process of knee injuries, and physical therapy techniques can aid in the recovery timeline.
- Low-impact exercises are beneficial for knee injuries, while strength training and flexibility exercises contribute to knee stability and range of motion.
- Consistency and gradual progression are key principles in safe and effective knee injury exercises.
- Consulting a healthcare professional or physical therapist is important before starting any exercise program for knee injuries.
Understanding Knee Injuries
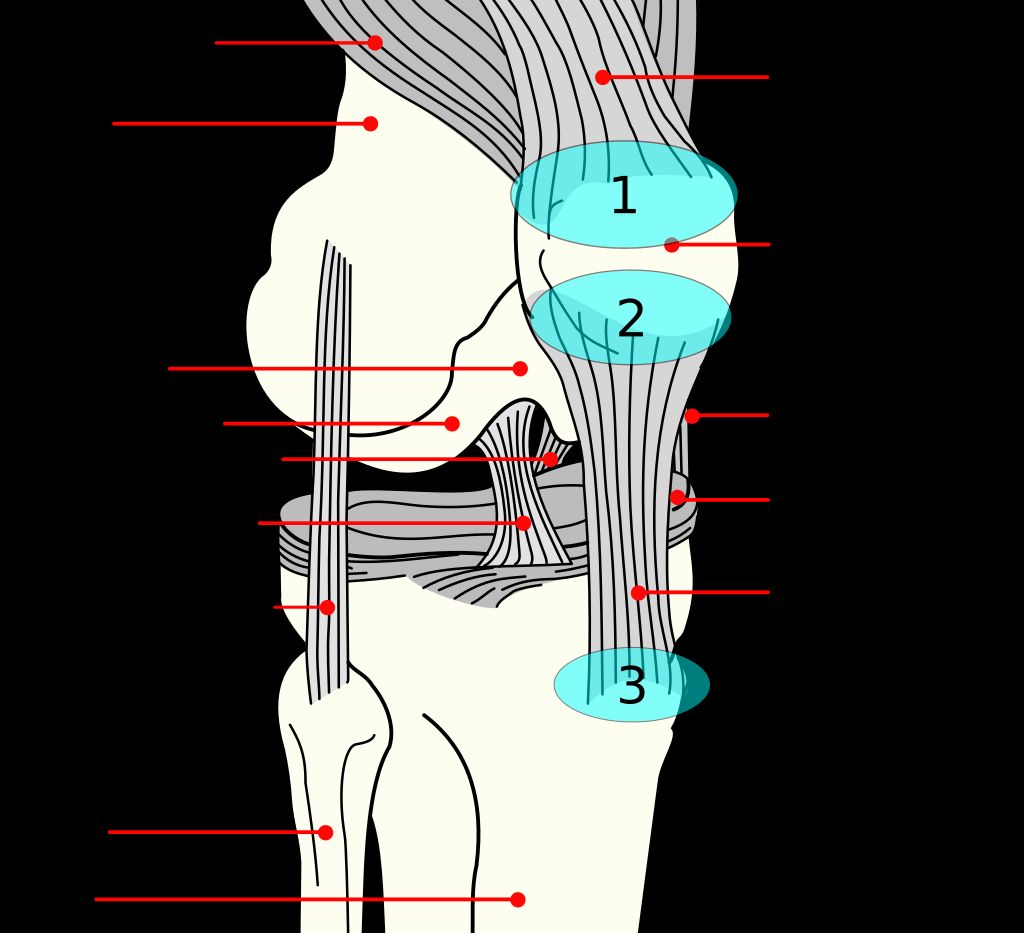
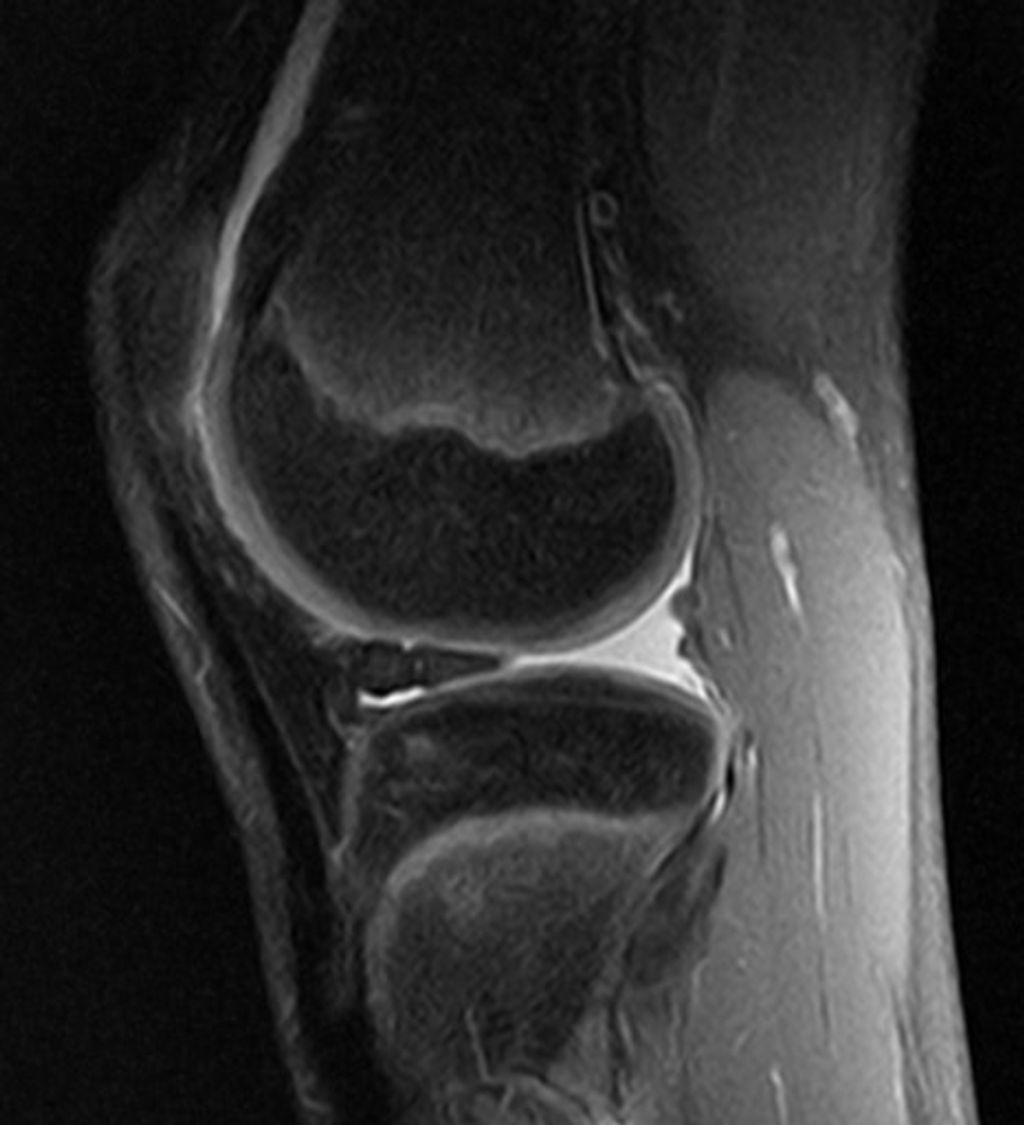
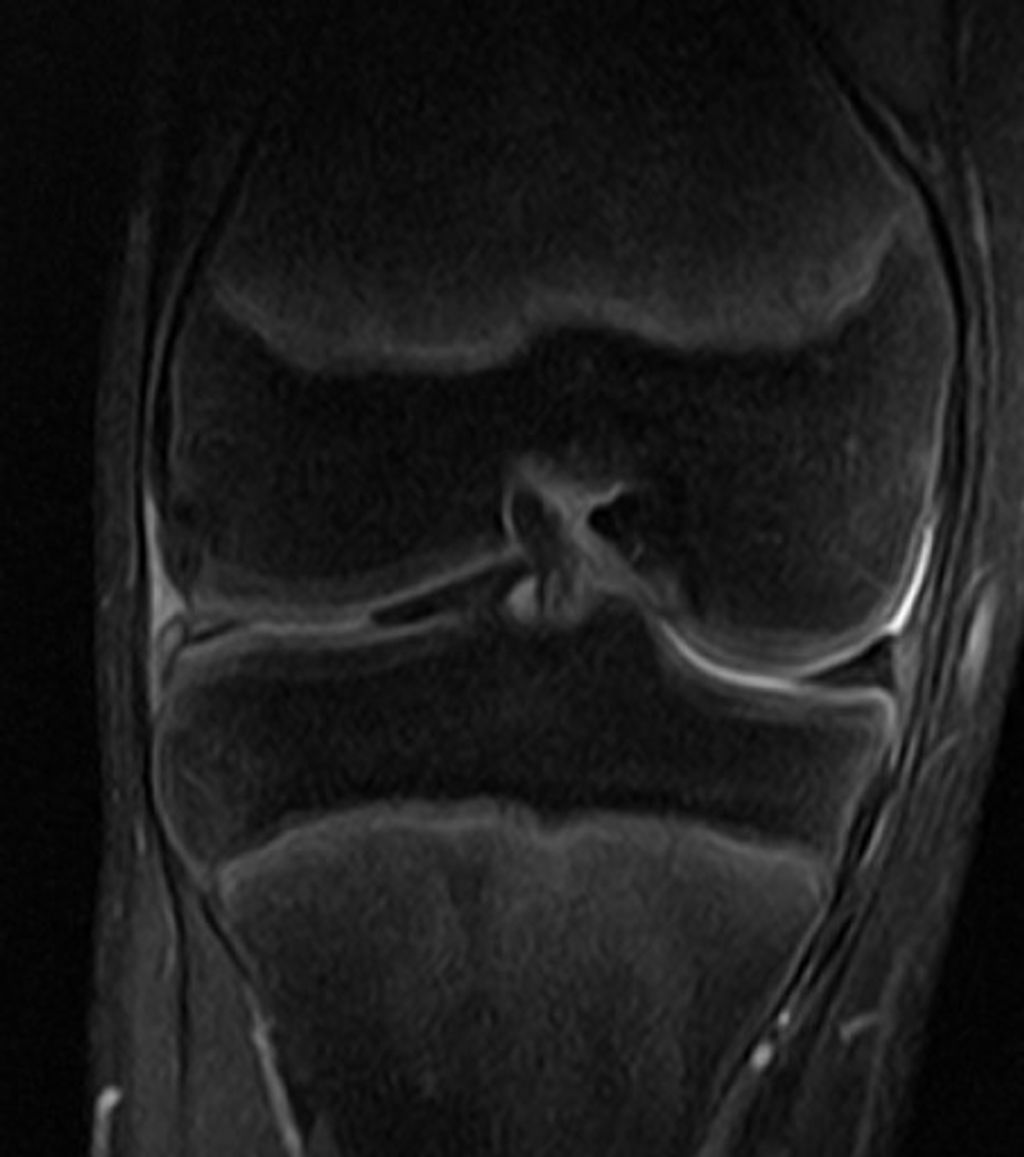
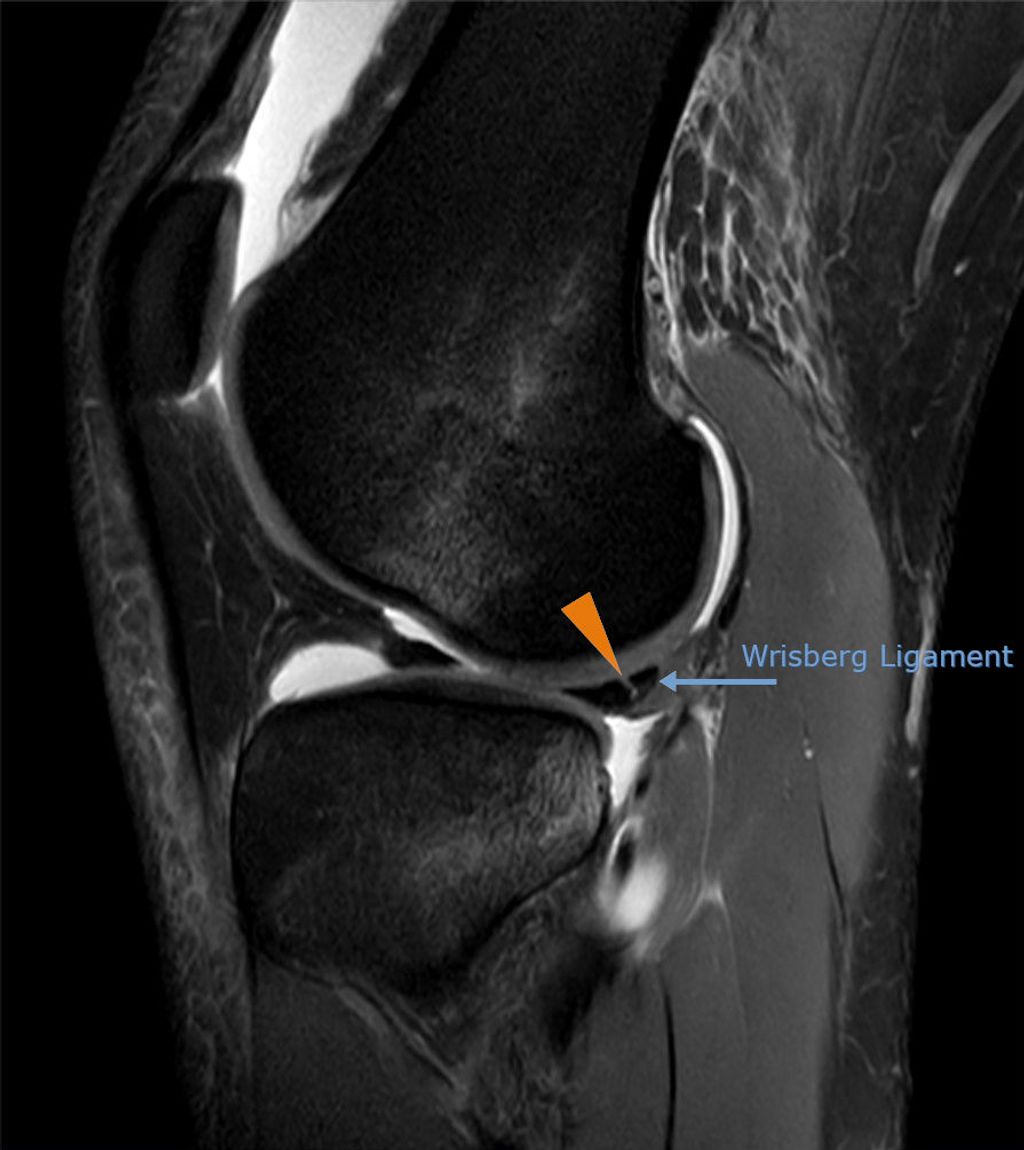
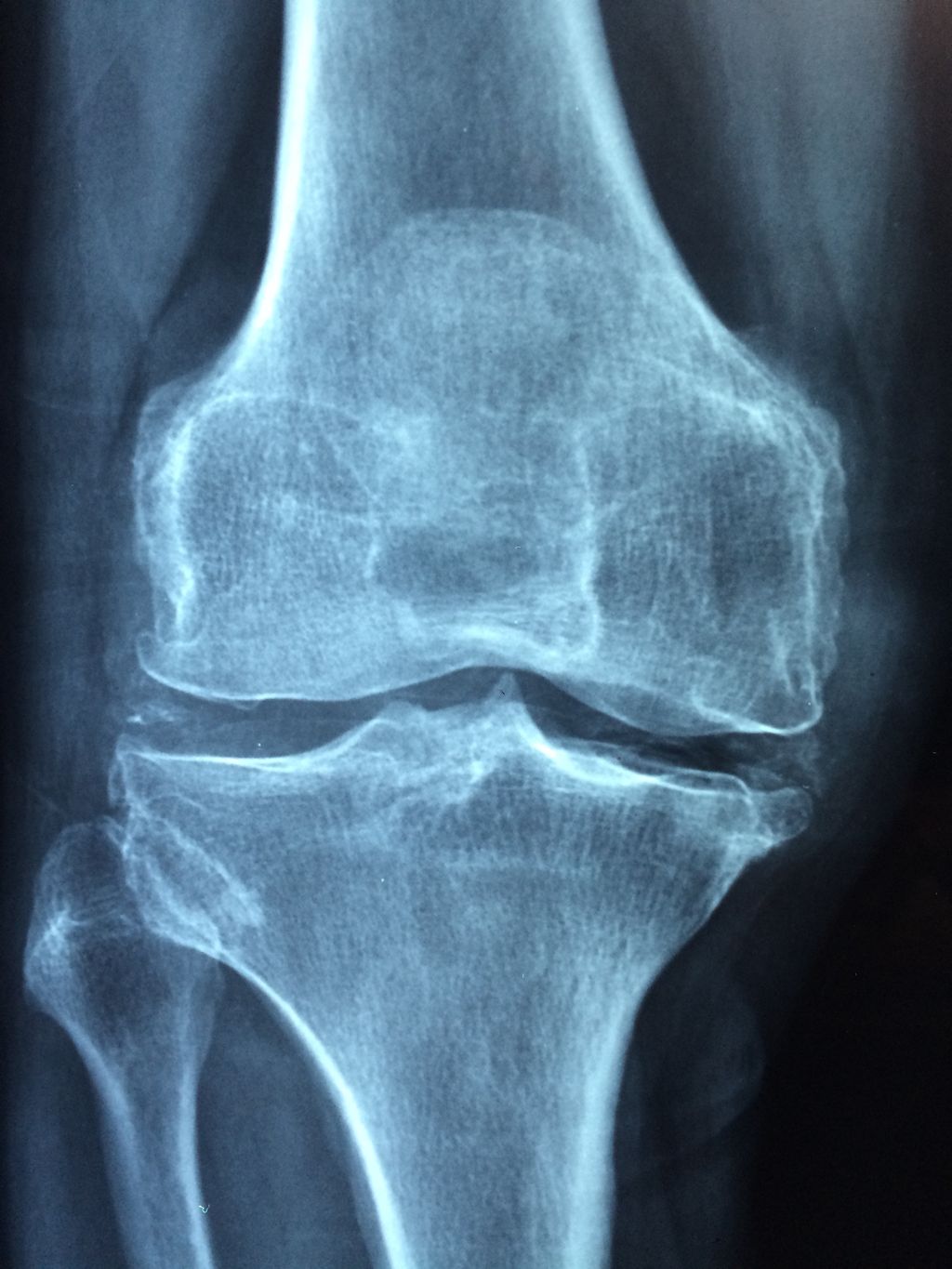
Common Types of Knee Injuries
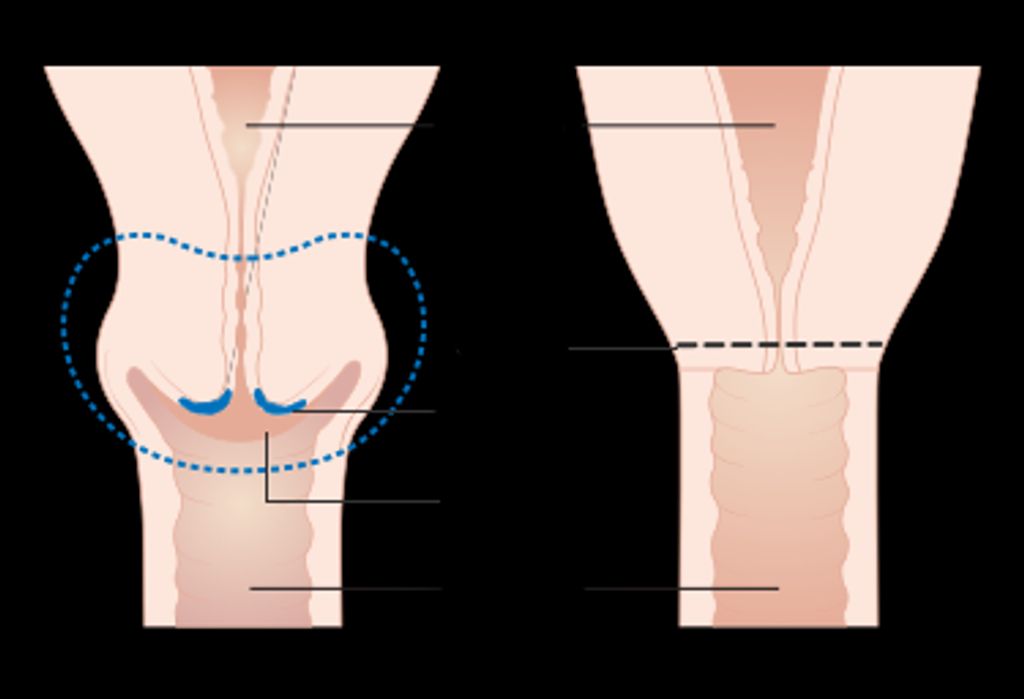
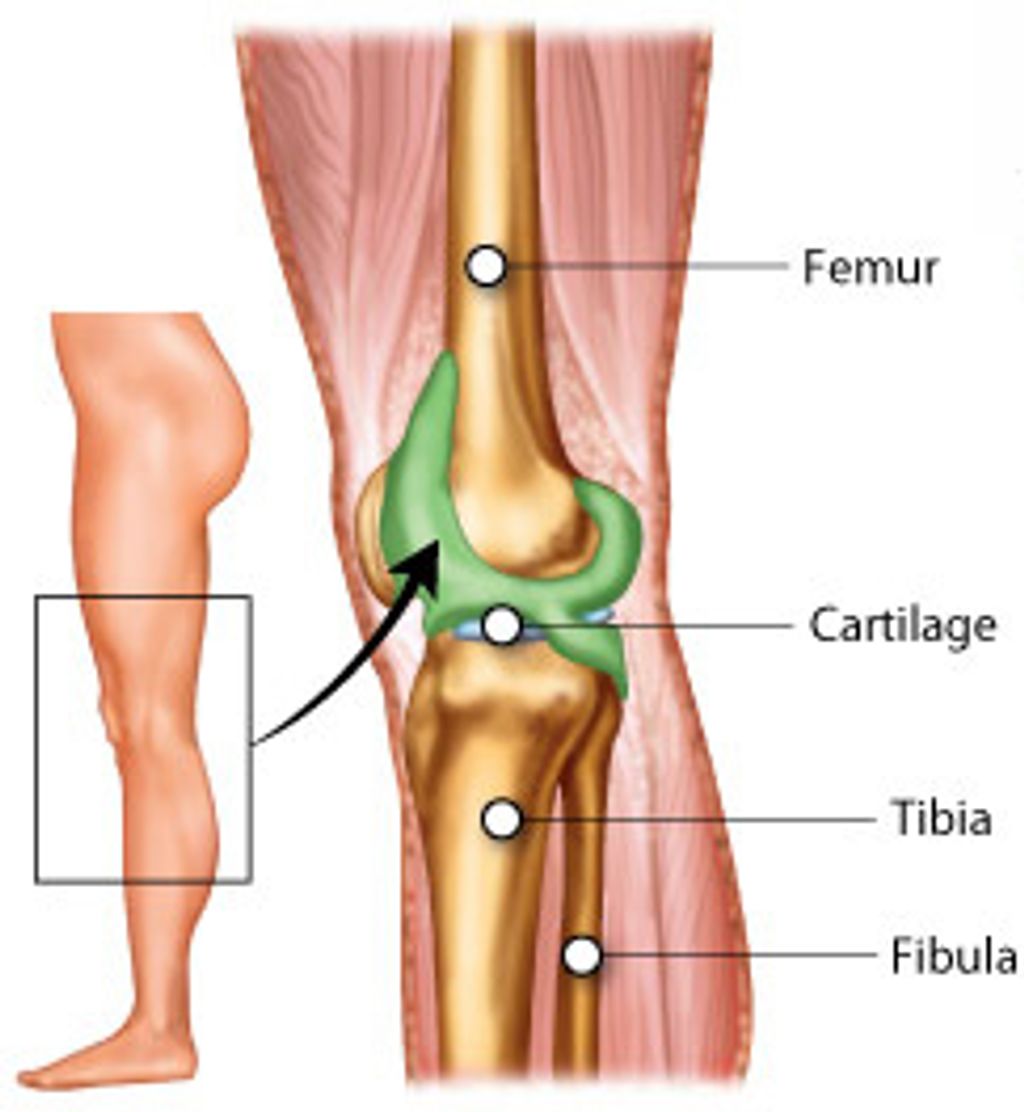
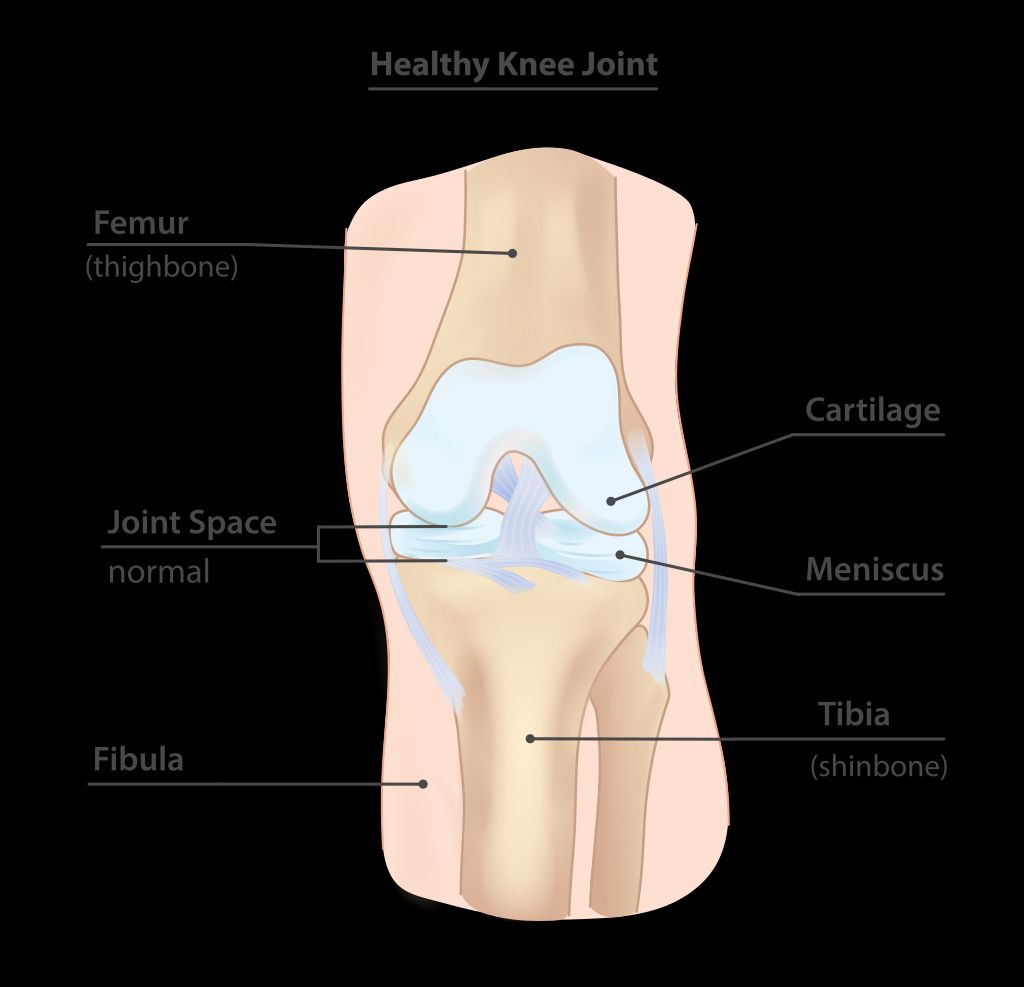
Knee injuries can be caused by a variety of factors, including overuse, trauma, and aging. It is important to understand the specific nature of the injury in order to develop an effective rehabilitation plan. For example, a study by Johns Hopkins Medicine found that the most common types of knee injuries include ligament sprains, meniscus tears, and patellar dislocations. These injuries can significantly impact an individual’s mobility and quality of life. Understanding the nuances of each injury is crucial for tailored treatment and recovery.
Causes of Knee Injuries
Knee injuries can be caused by a variety of factors, including overuse, sudden impact, and improper form during physical activities. These factors can lead to damage in the ligaments, tendons, and cartilage surrounding the knee joint. Additionally, age and pre-existing conditions such as arthritis can contribute to the vulnerability of the knee to injuries.
It’s important to note that proper warm-up and stretching routines can help reduce the risk of knee injuries. Here’s a table summarizing the key factors contributing to knee injuries:
| Factor | Impact Level |
|---|---|
| Overuse | High |
| Sudden Impact | High |
| Improper Form | Moderate |
| Age | Moderate |
| Pre-existing Conditions | Moderate |
In addition to these factors, maintaining a healthy weight and avoiding excessive stress on the knees can significantly reduce the risk of injury. Remember, prevention is key to maintaining knee health and preventing injuries.
Risk Factors for Knee Injuries
We recognize that certain factors can significantly increase the likelihood of sustaining knee injuries. These risk factors vary widely, encompassing both intrinsic and extrinsic elements. Intrinsic factors are those related to an individual’s own body, such as age, gender, and genetics. Extrinsic factors include environmental conditions and activity levels.
Age is a primary intrinsic factor, with older individuals often experiencing a higher incidence of knee injuries due to wear and tear on the joints. Gender also plays a role; for example, women are more prone to anterior cruciate ligament (ACL) injuries due to differences in muscle strength and hormonal influences. Genetics can predispose individuals to certain conditions that affect knee health, such as osteoarthritis.
When it comes to extrinsic factors, athletes, particularly those involved in high-impact sports like football or basketball, face a heightened risk. However, it’s not just athletes; occupational hazards and lifestyle choices can also contribute. For instance, jobs that require repetitive knee motions or heavy lifting can lead to chronic knee issues.
Tip: Maintaining a healthy weight and engaging in regular, balanced exercise can mitigate some of the risk factors for knee injuries.
Understanding these risk factors is crucial for both prevention and effective management of knee injuries. By acknowledging and addressing these elements, we can better tailor rehabilitation programs and exercise protocols to individual needs.
Rehabilitation and Recovery

Importance of Rehabilitation
In our journey to recovery from knee injuries, we recognize the paramount importance of rehabilitation. It is not merely a phase of recovery; it is a crucial process that demands our commitment and patience. Rehabilitation serves as the bridge between injury and returning to daily activities, ensuring that the knee regains its strength and functionality.
Rehabilitation involves a series of carefully designed exercises and therapies aimed at restoring knee stability and mobility. It is essential to adhere to the prescribed regimen to prevent the risk of re-injury and to promote optimal healing. Here’s a brief overview of the rehabilitation process:
- Initial rest and inflammation control
- Gradual reintroduction of movement
- Strengthening surrounding muscles
- Enhancing flexibility and range of motion
Tip: Always consult with a healthcare professional before starting any rehabilitation exercises to ensure they are suitable for your specific injury and recovery stage.
Recovery Timeline for Knee Injuries
Understanding the recovery timeline for knee injuries is crucial in setting realistic expectations and goals. The healing process is generally divided into phases, each characterized by specific recovery milestones and treatment objectives.
Phase 1: Acute Injury Management – This initial phase focuses on reducing pain and swelling. Rest, ice, compression, and elevation (RICE) are fundamental during this period, which typically lasts from a few days to a week.
Phase 2: Early Mobilization – As pain and swelling decrease, gentle range-of-motion exercises are introduced to prevent stiffness. This phase may last from 1 to 3 weeks.
Phase 3: Strengthening and Conditioning – Once mobility improves, strength and conditioning exercises become the focus. This phase aims to restore knee stability and can last several weeks to months, depending on the severity of the injury.
Phase 4: Functional Training – The final phase involves exercises that mimic daily activities or sport-specific movements. This stage prepares individuals for a safe return to their pre-injury level of activity.
Tip: It’s essential to progress through each phase under the guidance of a healthcare professional to avoid setbacks and ensure a complete recovery.
Physical Therapy Techniques
After completing the physical therapy techniques, our team focuses on implementing a comprehensive exercise program to further aid in the rehabilitation and recovery process. This program includes a combination of low-impact exercises, strength training, and flexibility and range of motion exercises. The goal is to gradually improve knee stability and function while minimizing the risk of re-injury. Here’s a brief overview of the exercise protocols we recommend:
- Low-Impact Exercises: These gentle exercises are designed to minimize stress on the knee joint while promoting circulation and muscle activation. Examples include stationary cycling, swimming, and gentle yoga.
- Strength Training: Building strength in the muscles surrounding the knee is crucial for providing support and stability. We emphasize exercises that target the quadriceps, hamstrings, and calf muscles.
- Flexibility and Range of Motion: Stretching and mobility exercises play a vital role in maintaining and improving the knee’s range of motion. Our program includes dynamic and static stretching routines to enhance flexibility and reduce stiffness.
It’s important to progress gradually and listen to your body throughout the exercise program. Consistency and patience are key to achieving long-term recovery and preventing future knee injuries.
Exercise Protocols for Knee Injuries
Low-Impact Exercises for Knee Injuries
In our journey to rehabilitate knee injuries, we recognize the significance of low-impact exercises. These activities are designed to minimize stress on the knee joint while still promoting movement and strength. We advocate for a gradual approach, starting with the simplest exercises and progressively increasing intensity as the knee heals.
Some of the most beneficial low-impact exercises include:
- Cycling on a stationary bike, which allows for controlled movement without excessive strain.
- Swimming and water aerobics, where the buoyancy of water supports the body and reduces impact.
- Using an elliptical machine to simulate walking or running with less force on the knees.
Tip: Always listen to your body and avoid pushing through pain. If an exercise causes discomfort, modify it or choose an alternative that feels better for your knee.
It’s essential to incorporate these exercises into a regular routine, ensuring consistency in the recovery process. By doing so, we can help the knee regain its strength and functionality without risking further injury.
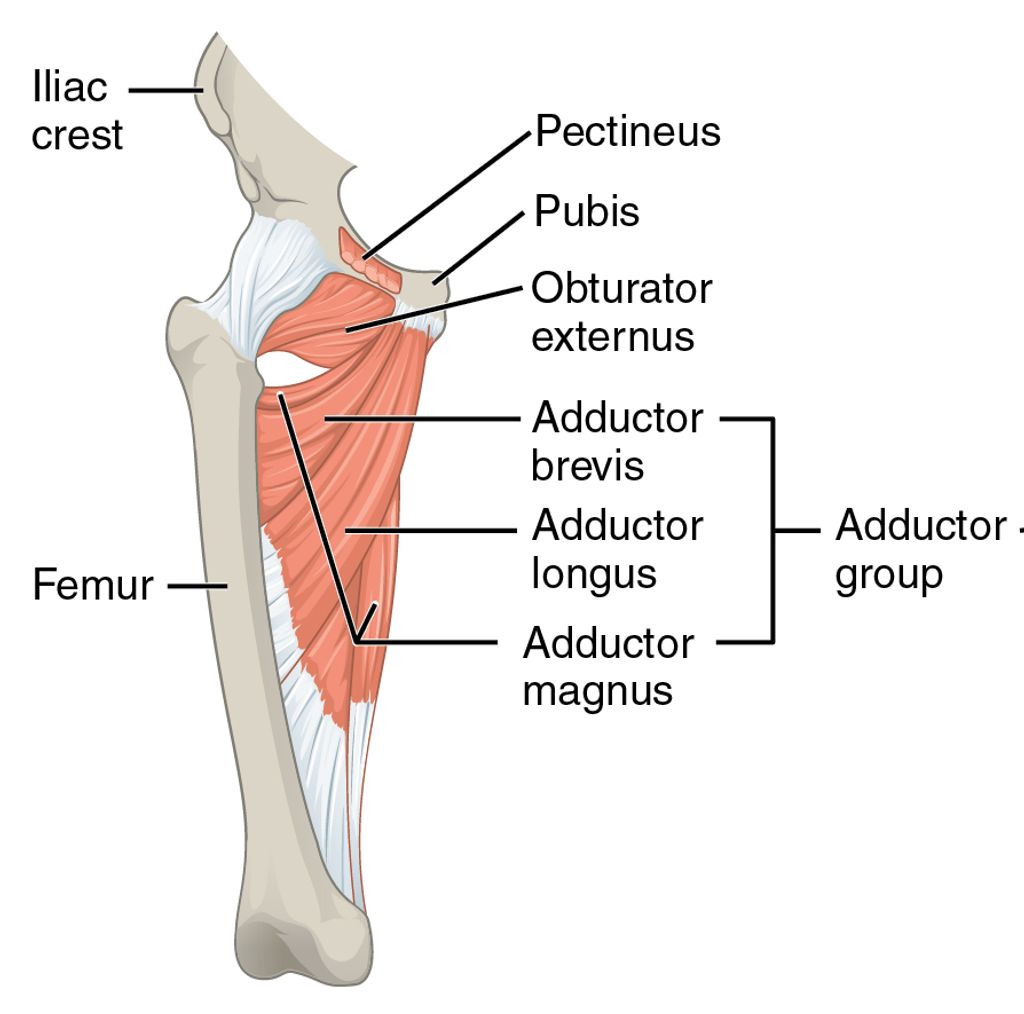
Strength Training for Knee Stability
We understand that the foundation of a strong knee is the stability provided by the surrounding muscles. Strength training is crucial for rebuilding the muscles around the knee, particularly after an injury. It’s important to focus on exercises that enhance the quadriceps and hamstrings, as these muscle groups play a pivotal role in knee stability.
Gradual progression is key in strength training. We start with low-resistance exercises and slowly increase the intensity as the knee regains strength. Here’s a simple progression we can follow:
- Isometric exercises such as quad sets and straight-leg raises
- Leg presses with light weights
- Step-ups and lunges with bodyweight
- Gradual introduction of weights to the previous exercises
Tip: Always listen to your body and avoid pushing through pain. Pain is a signal that we might be overexerting the injured knee.
It’s essential to maintain proper form throughout these exercises to prevent further injury. We encourage seeking guidance from a physical therapist to ensure that each movement is performed correctly.
Flexibility and Range of Motion Exercises
We understand the importance of maintaining flexibility and a full range of motion in the knee joint during the rehabilitation process. Flexibility exercises are essential in restoring the knee’s ability to move through its complete range without pain or stiffness. These exercises should be performed gently and within a pain-free range to ensure safety and effectiveness.
Hamstring stretches, calf stretches, and quadriceps stretches are foundational exercises that can help improve flexibility around the knee. It’s crucial to hold each stretch for at least 15-30 seconds to allow the muscles to relax and lengthen. Consistency is key, and we recommend incorporating these stretches into your daily routine.
Tip: Always warm up with light activity before stretching to increase blood flow to the muscles and reduce the risk of injury.
Below is a simple routine to enhance knee flexibility:
- Begin with a warm-up of light walking or cycling for 5-10 minutes.
- Proceed to hamstring stretches, holding each stretch for 30 seconds.
- Follow with calf stretches, ensuring you feel a gentle pull, not pain.
- Finish with quadriceps stretches, being careful not to strain the knee joint.
Remember, the goal is to improve flexibility without causing additional stress to the knee. If you experience any discomfort beyond mild stretching sensations, it is advisable to stop and consult with a healthcare professional.
Conclusion
In conclusion, the effectiveness of knee injury exercises cannot be overstated. By following a structured and safe exercise regimen, individuals can significantly improve their knee strength and stability. It is imperative to consult a qualified healthcare professional before embarking on any exercise program, especially for individuals with a history of knee injuries. With the right guidance and commitment, recovery and prevention of knee injuries are achievable goals.
Frequently Asked Questions
What are the most common types of knee injuries?
Common types of knee injuries include ACL tears, meniscus tears, and patellar tendinitis.
What are the main causes of knee injuries?
Knee injuries can be caused by sudden trauma, overuse, or degenerative conditions like arthritis.
What are the risk factors for knee injuries?
Risk factors for knee injuries include age, obesity, sports participation, and improper training techniques.
Why is rehabilitation important for knee injuries?
Rehabilitation is important for restoring strength, stability, and function to the knee after an injury, and to prevent future injuries.
How long does it take to recover from a knee injury?
The recovery timeline for knee injuries varies depending on the severity of the injury, but it can range from a few weeks to several months.
What are some effective physical therapy techniques for knee injuries?
Physical therapy techniques for knee injuries may include strengthening exercises, manual therapy, and modalities like ice and heat therapy.