Torn meniscus is a common injury, especially among individuals over the age of 50. Understanding the causes, symptoms, diagnosis, and treatment options is crucial for managing this condition effectively. In this article, we will explore the key aspects of torn meniscus and provide valuable insights into recovery and prevention strategies.
Key Takeaways
- Torn meniscus is often caused by degenerative changes in the knee, as well as sudden twisting or pivoting movements.
- Symptoms of a torn meniscus may include pain, swelling, stiffness, and difficulty fully extending the knee.
- Diagnostic tests such as MRI and physical examination are used to confirm a torn meniscus.
- Non-surgical treatment options for torn meniscus include rest, ice, compression, and elevation (RICE therapy), as well as physical therapy.
- Rehabilitation after surgical treatment involves a structured timeline, including physical therapy exercises to restore strength and flexibility in the knee.
Understanding Torn Meniscus

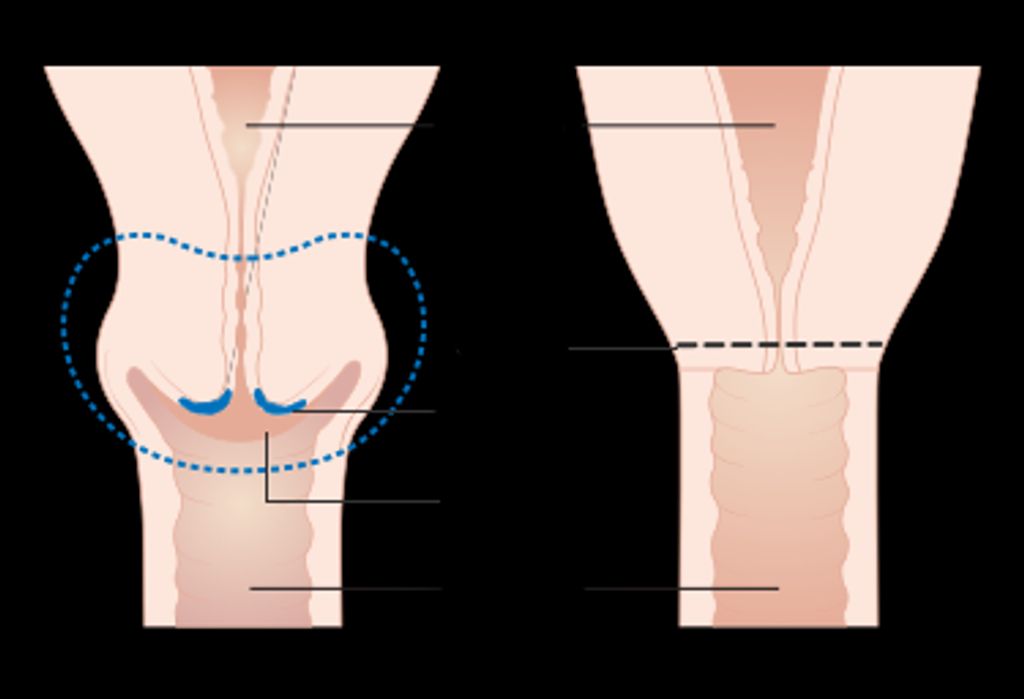
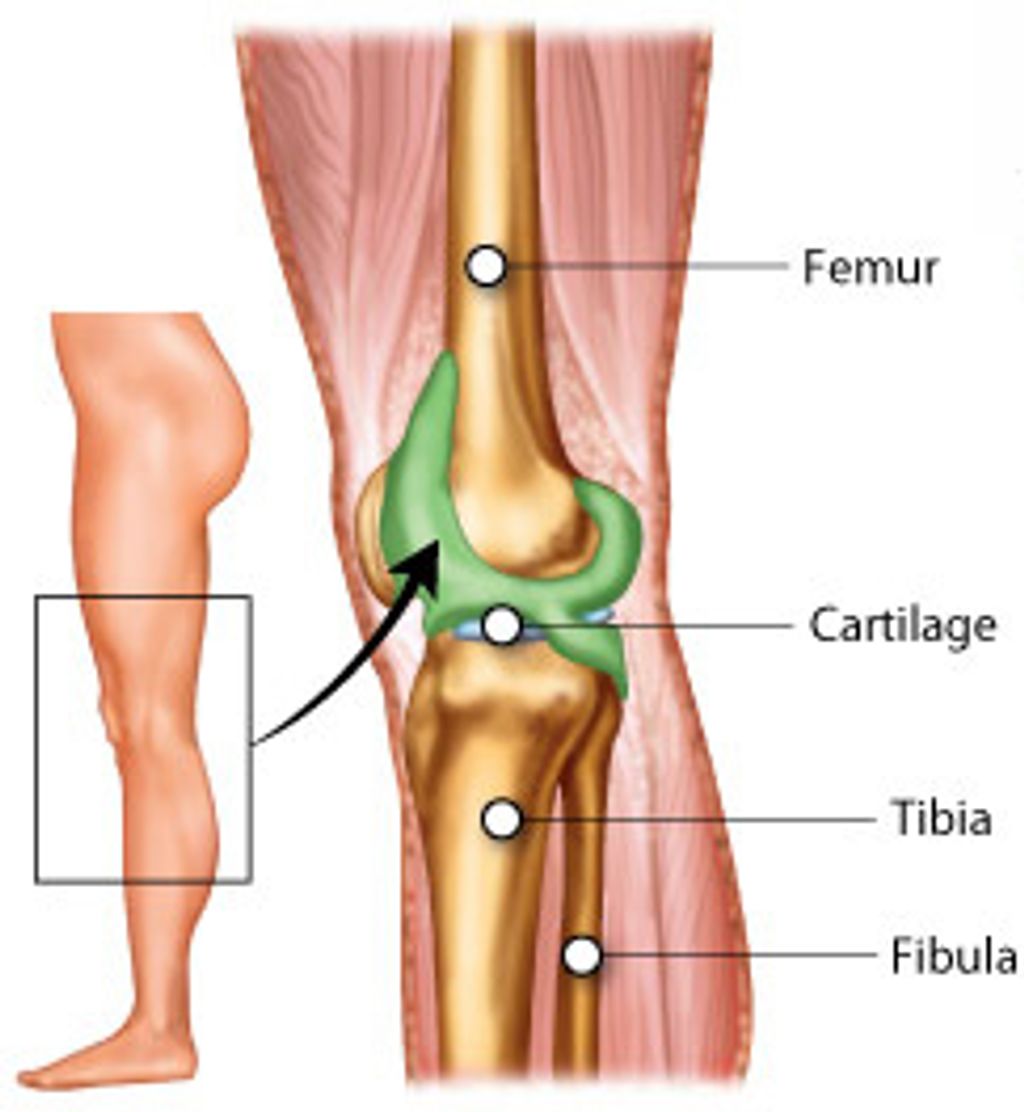
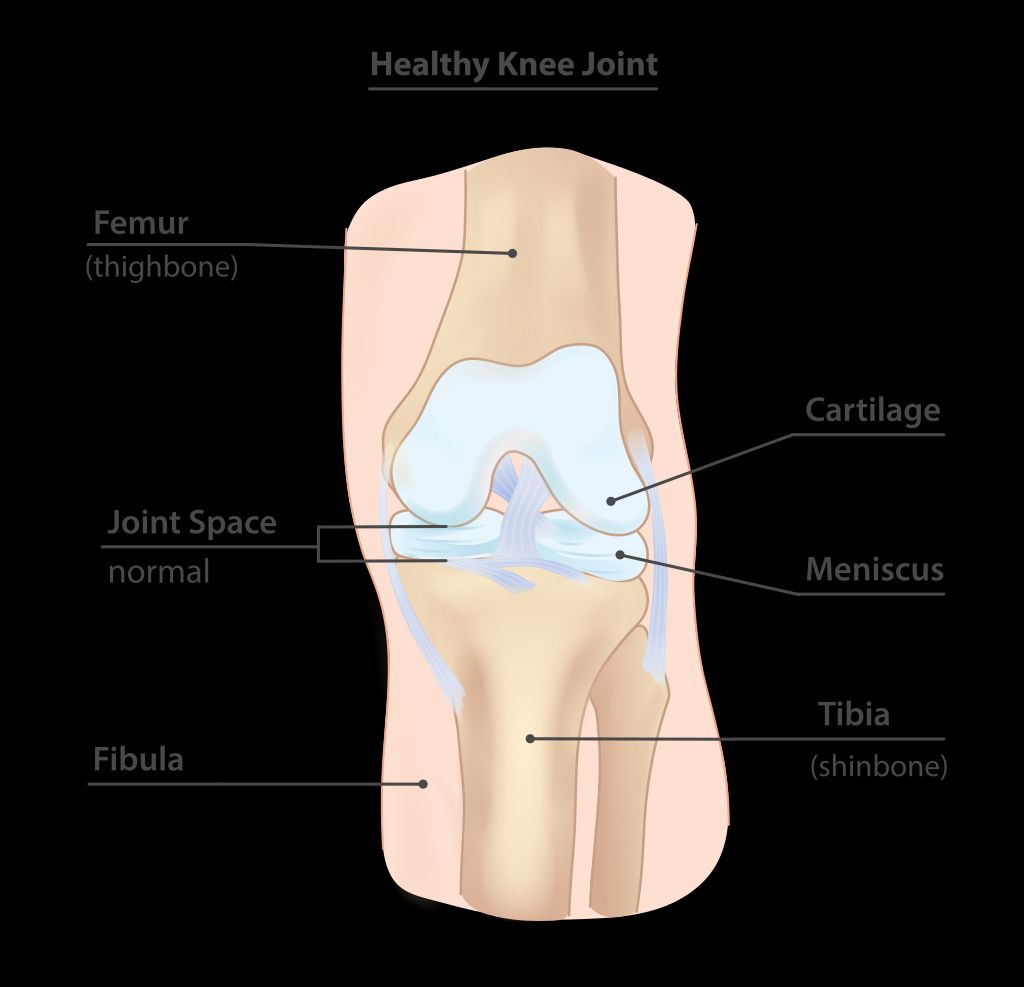
Anatomy of the Meniscus
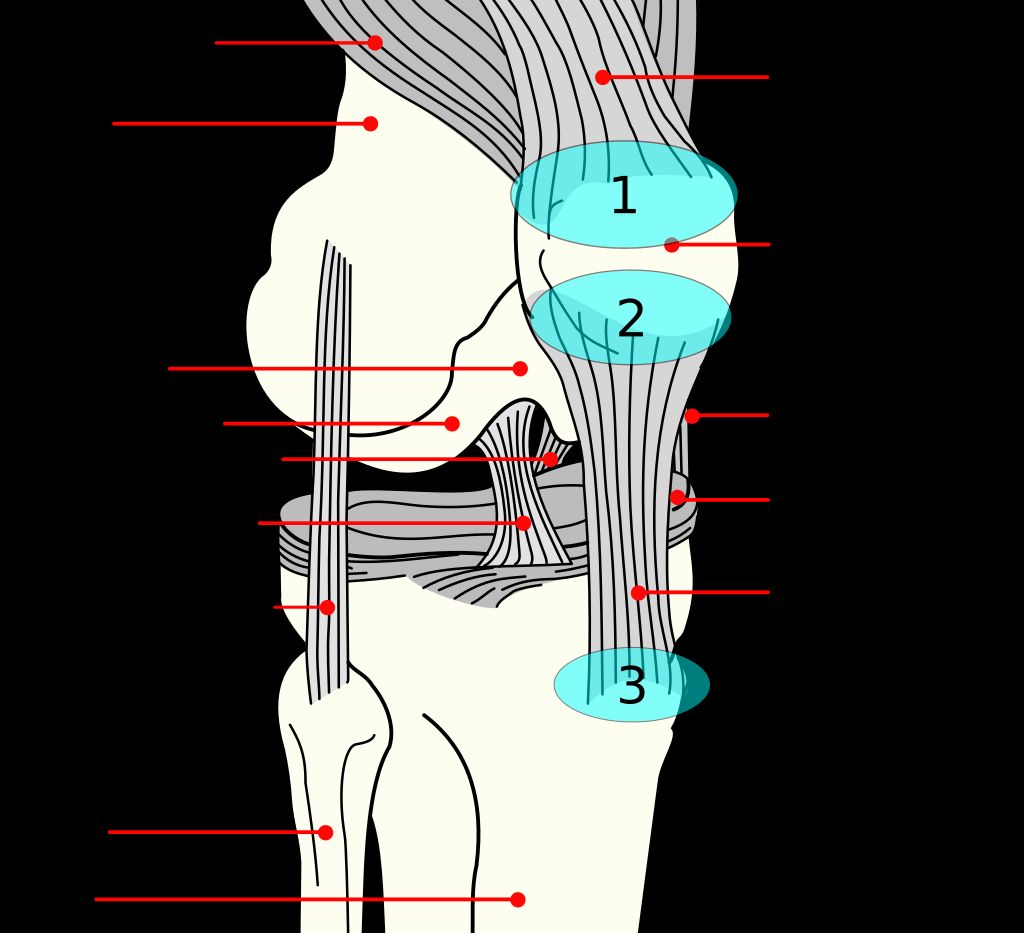
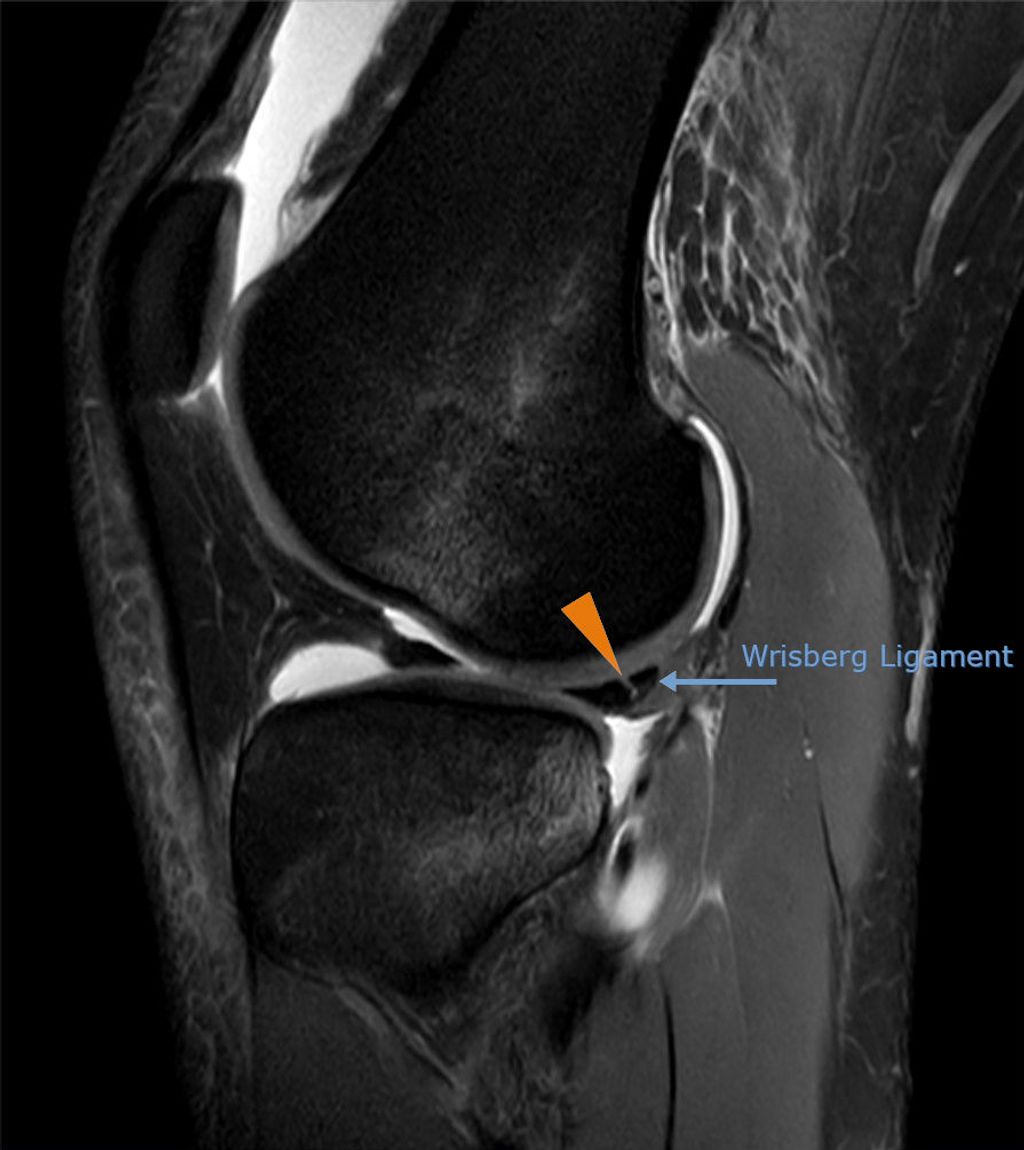
In our exploration of knee injuries, we must first understand the meniscus, a crucial component of knee stability and function. Composed of two C-shaped pieces of cartilage, the menisci (plural) sit between the femur (thigh bone) and the tibia (shin bone).
Each knee has a lateral meniscus on the outer side and a medial meniscus on the inner side. These structures act as shock absorbers, distributing the weight of the body across the knee joint. They also aid in the smooth movement of the joint, providing a gliding surface for the femur.
Tip: Maintaining strong and flexible leg muscles can help support the menisci and reduce the risk of injury.
The health of our menisci is vital, especially as we age. Over time, the meniscus can become more susceptible to injury due to degeneration and decreased elasticity. It’s important for us to recognize the signs of a torn meniscus and seek appropriate treatment to prevent further damage and maintain mobility.
Causes of Torn Meniscus
In our exploration of meniscal injuries, we recognize that the causes of a torn meniscus can be multifaceted, particularly in individuals over 50. As we age, the meniscus becomes more brittle and less elastic, making it more susceptible to tears even with minor twisting movements or squatting. This degenerative process is often exacerbated by osteoarthritis, which can further compromise the integrity of the meniscal tissue.
Degenerative meniscal tears are common in the older population and differ from the acute tears seen in younger individuals, which are usually the result of a specific traumatic event. In contrast, older adults may experience a meniscal tear as a part of the natural aging process, without a notable injury.
- Trauma: Sudden twists or turns, especially with the foot planted and the knee bent.
- Degeneration: Natural wear and tear over time, often associated with aging.
- Overuse: Repetitive activities that strain the knee joint.
Tip: Maintaining a healthy weight and regular exercise can help reduce the risk of degenerative meniscal tears by alleviating pressure on the knee joints and preserving muscle strength.
Symptoms of Torn Meniscus
Anatomy of the Meniscus, Causes of Torn Meniscus, and Symptoms of Torn Meniscus are crucial aspects of understanding this injury. We must pay close attention to the symptoms, as they often indicate the severity of the tear. In some cases, a torn meniscus may cause the knee to lock, making it difficult to fully straighten the leg. This can be a sign of a more serious tear.
- It’s important to note that not all torn menisci require surgery. In fact, studies have shown that 70% of people over 50 with a torn meniscus can successfully manage the injury with non-surgical treatment.
- However, for those who do require surgery, the recovery timeline and physical therapy are essential components of the treatment plan.
Tip: If you experience persistent knee pain or difficulty moving your knee, it’s important to seek medical attention promptly.
Diagnosis and Treatment Options

Diagnostic Tests for Torn Meniscus
When we suspect a torn meniscus in patients over 50, a thorough diagnostic process is crucial to determine the appropriate treatment plan. The first step typically involves a detailed medical history and physical examination, where we assess the knee’s range of motion and look for signs of meniscal injury.
Following the initial assessment, we often recommend imaging tests to visualize the extent of the damage. The most common diagnostic tools include:
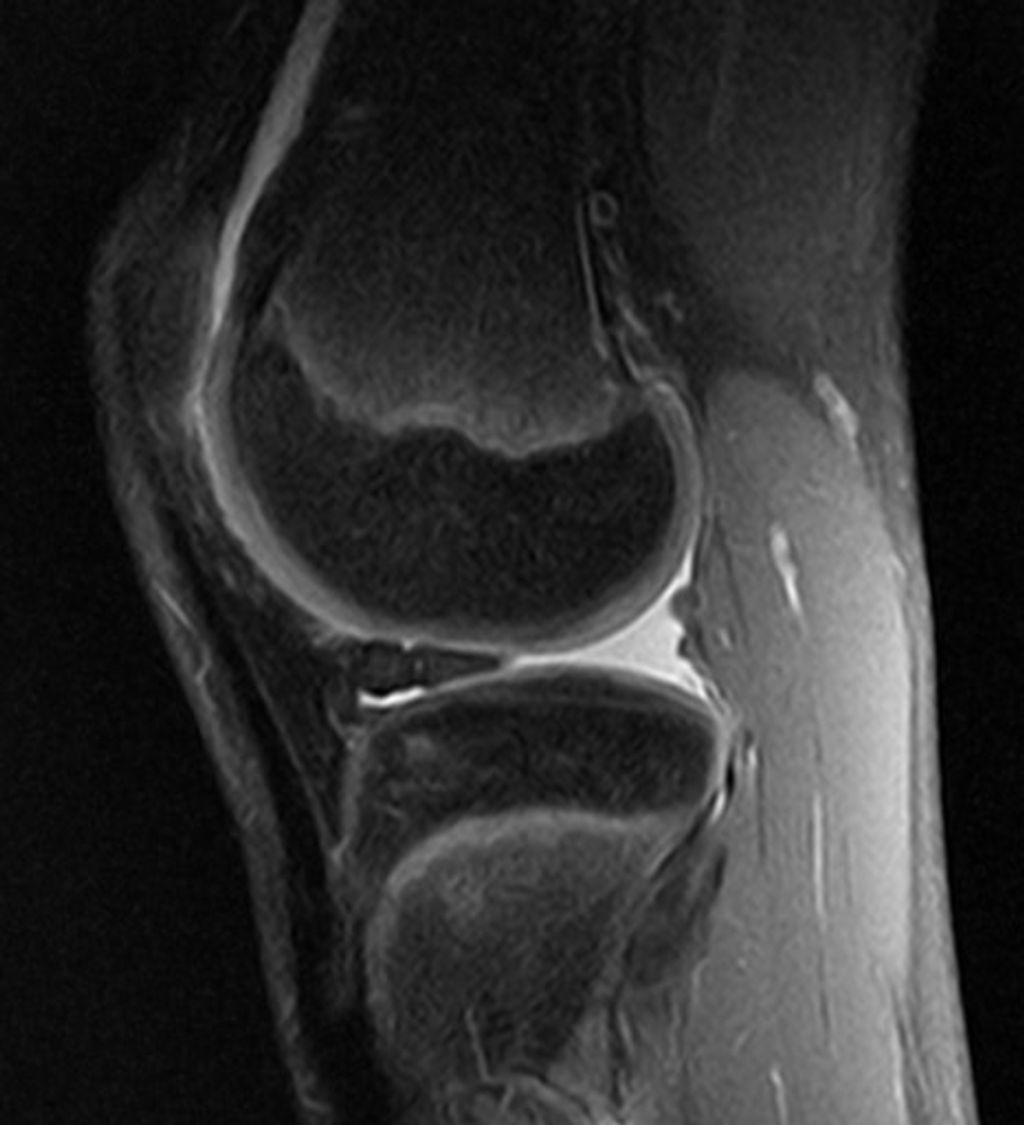
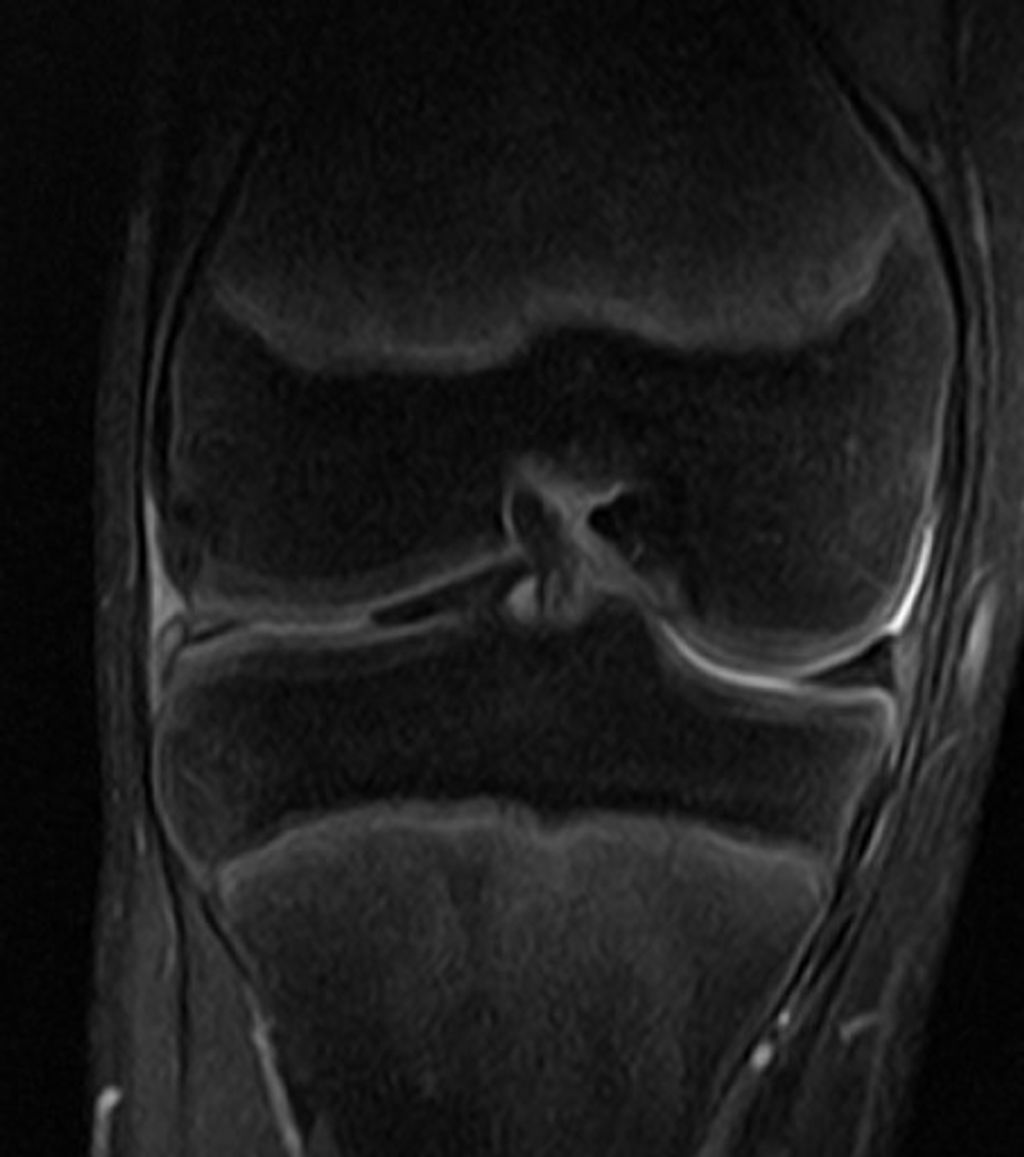
- Magnetic Resonance Imaging (MRI): This is the most sensitive test for meniscus tears, providing clear images of both hard and soft tissues within the knee joint.
- X-rays: Although X-rays do not show soft tissue like the meniscus, they can help rule out other causes of knee pain, such as fractures or osteoarthritis.
- Ultrasound: A less common test, but useful in some cases to evaluate soft tissue structures around the knee.
Tip: Early diagnosis and treatment are key to managing symptoms and preventing further joint damage.
In some cases, diagnostic arthroscopy, a minimally invasive surgical procedure, may be used when imaging results are inconclusive. This allows direct visualization of the internal structures of the knee. However, we strive to reserve this option for when non-invasive tests are insufficient.
Non-Surgical Treatment
When we manage a torn meniscus in individuals over 50, we often prioritize non-surgical treatment options. These methods focus on alleviating pain and swelling while promoting healing and mobility. The cornerstone of non-surgical treatment is physical therapy, which is tailored to each patient’s needs and abilities. Physical therapists may employ a variety of techniques, including exercises to strengthen the muscles around the knee, improve flexibility, and increase range of motion.
In addition to physical therapy, we recommend the following regimen to support recovery:
- Rest and avoidance of activities that exacerbate knee pain
- Application of ice to reduce swelling
- Compression with a knee brace or wrap to provide support
- Elevation of the leg to decrease swelling
Tip: It’s crucial to follow the guidance of your healthcare provider to ensure that activities are resumed gradually to prevent further injury.
For pain management, over-the-counter anti-inflammatory medications, such as ibuprofen or naproxen, can be effective. In some cases, corticosteroid injections may be considered to provide temporary relief. It is important to note that while these treatments can help manage symptoms, they do not repair the torn meniscus itself.
Surgical Treatment
After considering the options for surgical treatment, recovery and rehabilitation become crucial for our overall well-being. It’s important to understand the recovery timeline and the role of physical therapy in regaining strength and mobility. Additionally, preventing future injuries is a key aspect of our long-term health. Here’s a brief overview of the recovery timeline:
Recovery and Rehabilitation

Recovery Timeline
After undergoing treatment for a torn meniscus, we understand that patients are eager to know how long it will take to return to their normal activities. The recovery timeline can vary significantly depending on the severity of the tear and the type of treatment received. Generally, patients can expect a basic framework for recovery, which we outline below.
- Immediate postoperative period (0-2 weeks): Pain management and reduction of swelling are the primary goals. Use of crutches and a knee brace may be necessary.
- Early rehabilitation phase (2-6 weeks): Gradual increase in knee mobility and introduction of light exercises.
- Mid-rehabilitation phase (6-12 weeks): Continued strengthening exercises and progressive weight-bearing activities.
- Late rehabilitation phase (12 weeks and beyond): Return to more strenuous activities and sport-specific training.
It’s important to note that these timeframes are approximate and individual recovery may differ. Patients should always follow their healthcare provider’s guidance and listen to their own body’s signals during the recovery process.
Tip: Consistency in following the prescribed rehabilitation protocol is crucial for a successful recovery. Avoid overexerting the knee too early to prevent setbacks.
Physical Therapy
In our journey to recovery from a torn meniscus, we recognize the pivotal role of physical therapy. It’s not just about healing; it’s about regaining strength and mobility while ensuring the knee can handle daily activities without further injury.
Our regimen typically includes a variety of exercises tailored to individual needs. These exercises focus on improving flexibility, building strength, and enhancing coordination. For instance:
- Range-of-motion exercises to increase flexibility
- Strengthening exercises targeting the quadriceps and hamstrings
- Balance and agility drills to improve knee stability
Tip: Consistency is key in physical therapy. Adhering to the prescribed exercise routine maximizes the benefits and accelerates recovery.
We also emphasize the importance of home exercise programs. These are crucial for continued progress outside of therapy sessions. Our therapists provide guidance on how to safely perform exercises at home, ensuring that recovery continues unabated.
Preventing Future Injuries
After successfully navigating the recovery and rehabilitation process, we must focus on preventing future injuries to the meniscus. It’s crucial to maintain the strength and flexibility of the knee joint to minimize the risk of re-injury. We recommend incorporating a balanced routine that includes both aerobic exercises and strength training.
- Aerobic exercises such as swimming or cycling can improve cardiovascular health without placing excessive strain on the knees.
- Strength training should target the muscles around the knee, particularly the quadriceps and hamstrings, to provide better support to the joint.
Proper footwear is also essential in preventing meniscus injuries. Shoes that provide good support can help in maintaining proper knee alignment during physical activities.
Tip: Always warm up before engaging in any physical activity to prepare your muscles and joints, reducing the likelihood of injury.
Lastly, it’s important to listen to your body. If you experience pain or discomfort in the knee, it’s advisable to rest and consult a healthcare professional if the symptoms persist. By staying vigilant and adopting these preventive measures, we can help ensure the long-term health of our knees.
Conclusion
In conclusion, the management of torn meniscus in individuals over the age of 50 requires careful consideration of both surgical and non-surgical treatment options. It is imperative for patients to consult with a qualified orthopedic specialist to determine the most suitable course of action. With advancements in medical technology and rehabilitation techniques, the prognosis for individuals with torn meniscus remains promising, offering the potential for improved mobility and quality of life.
Frequently Asked Questions
What is a torn meniscus?
A torn meniscus is a common knee injury that involves the tearing of the cartilage in the knee joint, known as the meniscus.
How is a torn meniscus diagnosed?
A torn meniscus is usually diagnosed through a physical examination, imaging tests such as MRI, and sometimes arthroscopic surgery.
What are the non-surgical treatment options for a torn meniscus?
Non-surgical treatment options for a torn meniscus may include rest, ice, compression, elevation (RICE), physical therapy, and anti-inflammatory medications.
What is the recovery timeline for a torn meniscus?
The recovery timeline for a torn meniscus varies depending on the severity of the injury and the chosen treatment option. It can range from a few weeks to several months.
Can a torn meniscus lead to future knee injuries?
While a torn meniscus itself does not directly cause future knee injuries, it can increase the risk of developing osteoarthritis in the affected knee over time.
What can be done to prevent future knee injuries after a torn meniscus?
To prevent future knee injuries after a torn meniscus, it is important to maintain a healthy weight, engage in regular low-impact exercise, and avoid activities that put excessive strain on the knees.