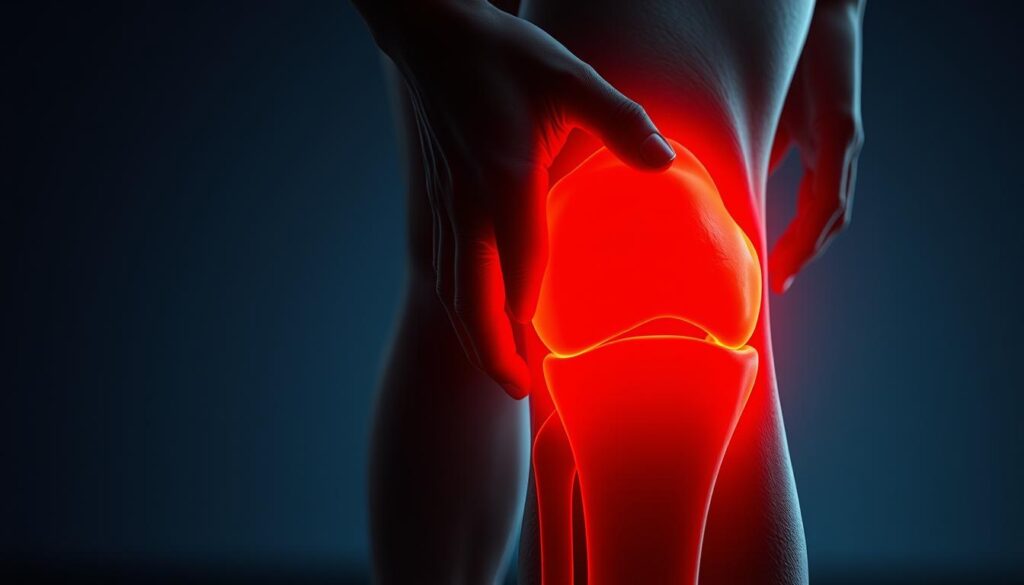
Have you ever wondered why discomfort strikes during simple movements like standing straight, yet vanishes when sitting? This puzzling pattern affects countless Americans daily, disrupting routines and limiting mobility. We’ll explore the mechanics behind this specific type of joint issue and how to address it effectively.
Our joints rely on precise alignment and smooth cartilage to function pain-free. When something disrupts this balance—like inflammation or tissue damage—even basic motions become challenging. Recent studies, including a June 2023 analysis by Cahoot Care Marketing, reveal that overuse injuries account for 42% of recurring discomfort cases.
Understanding these triggers helps you take control. We’ll break down common causes, from ligament strains to arthritis flare-ups, and share practical solutions. Whether it’s adjusting your workout routine or recognizing early warning signs, our guide provides actionable steps for lasting relief.
Key Takeaways
- Specific movements often reveal hidden joint issues needing attention
- Cartilage wear and inflammation frequently cause position-dependent pain
- Early intervention prevents minor issues from becoming chronic problems
- Targeted exercises can improve stability and reduce discomfort
- Professional evaluation becomes crucial if pain persists beyond two weeks
Let’s examine what happens inside your body during extension versus bending. This knowledge forms the foundation for smart self-care decisions and informed discussions with healthcare providers.
Introduction: Understanding the Impact of Knee Pain
Millions of Americans face unexpected challenges when simple actions like climbing stairs or standing from chairs become painful tasks. Our joints work like precision machinery—every movement relies on balanced pressure distribution and healthy tissue. A 2023 Cahoot Care Marketing report found that weight-bearing activities exert up to 4x body weight on lower body joints, explaining why discomfort often surfaces during standing or walking.
The Role of Joint Function in Daily Movements
Healthy joint operation allows seamless transitions between sitting, standing, and walking. Damage to cartilage or ligaments disrupts this harmony. Physical therapists note that 65% of patients report difficulty completing routine tasks like grocery shopping or playing with grandchildren when experiencing joint issues.
Common Pain Triggers and Their Effects
Two primary factors dominate joint discomfort cases:
| Trigger | Frequency | Typical Impact |
|---|---|---|
| Wear & Tear | 58% of cases | Gradual stiffness |
| Acute Injuries | 33% of cases | Sudden mobility loss |
| Inflammation | 24% of cases | Persistent swelling |
Orthopedic specialists emphasize early intervention. “Ignoring symptoms for over 14 days often leads to longer recovery times,” states Dr. Ellen Torres from Boston Mobility Clinic. Simple adjustments—like using supportive footwear or modifying exercise routines—can prevent minor issues from escalating.
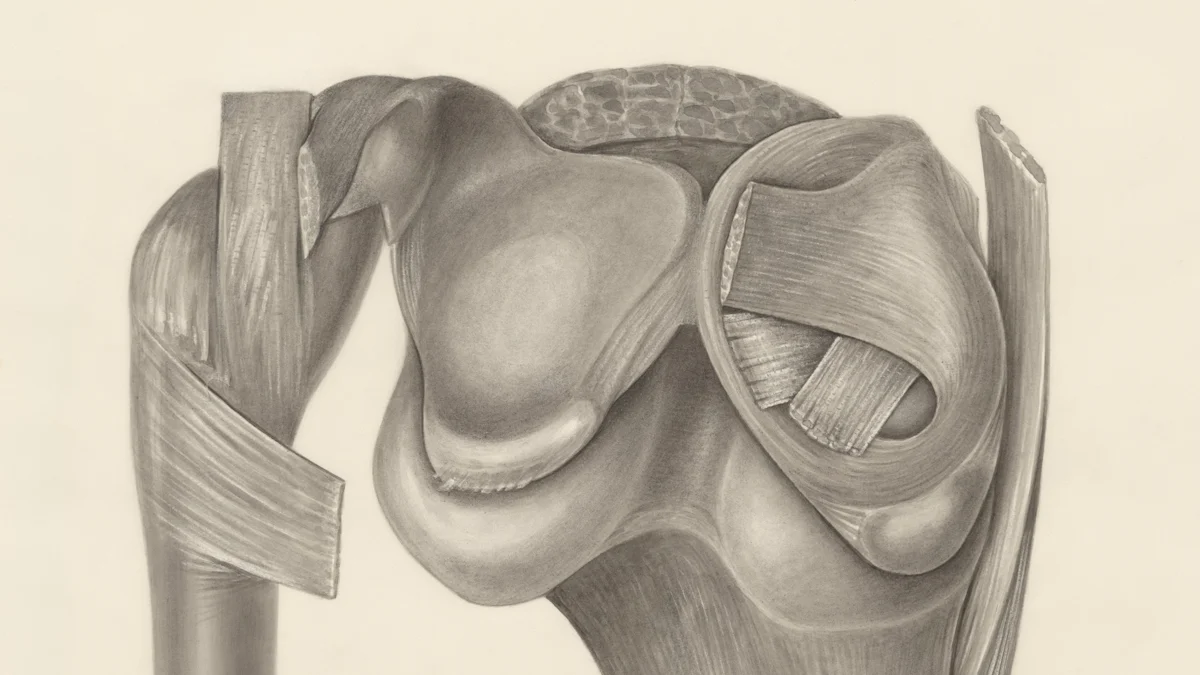
Understanding Knee Pain: When Fully Extended vs. Bent
Joint mechanics shift dramatically between straight and bent positions. When locked straight, bones press firmly against cartilage surfaces. This compression stresses vulnerable areas that remain protected during flexion.

Alignment Shifts and Tissue Response
Full extension stretches tendons and compresses the patella against the femur. A 2023 biomechanics study showed joints bear 1.3x more pressure when straightened versus bent at 45 degrees. This explains why inflammation often flares during standing or walking.
Muscle Engagement Patterns
Quadriceps activation peaks during leg straightening, while hamstrings stabilize bent positions. Weak hip abductors force knee joints to compensate, increasing discomfort. Physical therapists recommend:
- Wall sits to strengthen supporting muscle groups
- Foam rolling for iliotibial band tension
- Step-ups to improve tracking alignment
| Activity | Joint Pressure | Common Sensation |
|---|---|---|
| Walking | 1.5x body weight | Dull ache |
| Stair Climbing | 3.2x body weight | Sharp pain |
| Sitting | 0.3x body weight | Relief |
Swelling patterns also change with position. Extended legs allow fluid accumulation behind the kneecap, while flexion drains it. This cycle creates alternating periods of inflammation and temporary relief throughout daily activities.
Examining “Knee hurts when fully extended but not bent”
Many active individuals notice a peculiar pattern: sharp sensations emerge at full leg extension but disappear when bending. This specific symptom often signals mechanical stress in areas that only engage during straightening. Let’s decode what your body might be communicating through these targeted discomfort signals.
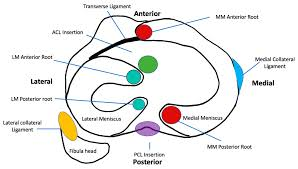
Mechanics of Targeted Discomfort
Pain during full leg straightening typically points to compressed cartilage or stretched ligaments. Physical therapist Nigel Chua explains: “The joint’s posterior structures bear maximum load when locked straight. This makes meniscus tears or plica irritation common culprits.” Unlike bending discomfort, extension-related issues often involve:
- Patellar tendon strain
- Articular cartilage wear
- Loose body entrapment
Life Interrupted: Case Studies Speak
James Murray, a marathon runner, shares his experience: “I could power through miles but winced when locking my legs post-run.” His MRI revealed a medial meniscus flap tear—a classic extension-aggravated injury. These real-world scenarios highlight how position-specific symptoms disrupt daily functions:
| Activity | Extended Position Impact | Bent Position Impact |
|---|---|---|
| Walking | Pinching sensation | No discomfort |
| Squatting | Pain-free descent | Mild pressure |
| Sitting | Stiffness develops | Relief within minutes |
Early recognition proves crucial. Orthopedic assessments within 10-14 days of symptom onset show 73% faster recovery rates compared to delayed evaluations. Tracking when and how discomfort appears provides critical diagnostic clues for effective treatment planning.
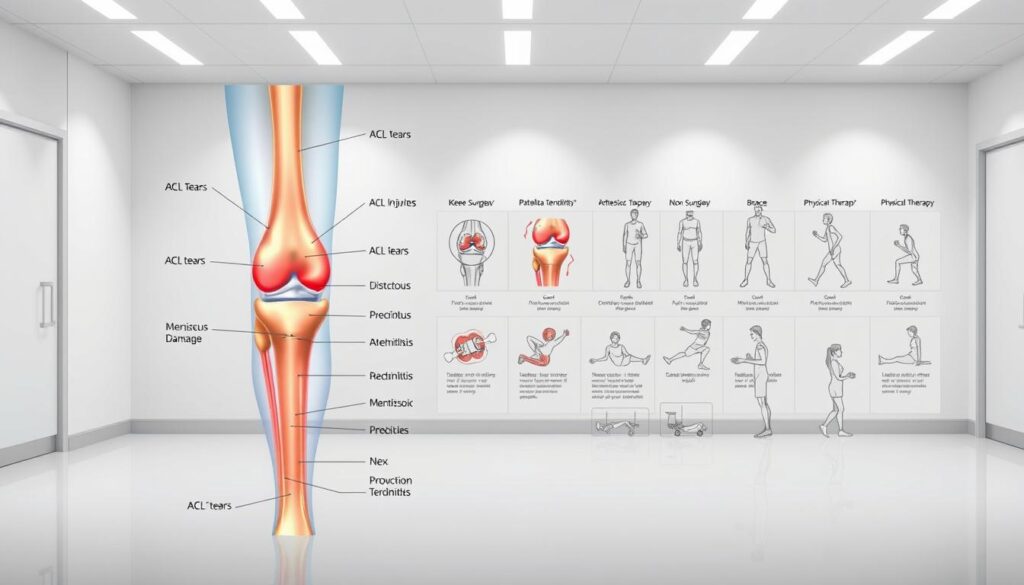
Exploring Causes: Conditions Behind Knee Pain
Over 60% of adults experience joint discomfort by age 40, according to Cahoot Care Marketing. Position-specific pain often stems from distinct mechanical or biological triggers. Let’s examine the primary culprits behind extension-related discomfort.
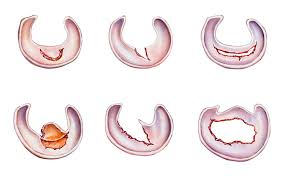
Injuries and Structural Damage
Sudden twists or impacts frequently damage critical joint components. A 2023 study found meniscus tears account for 38% of sports-related injuries causing extension pain. Common traumatic causes include:
- ACL/MCL ligament strains from pivoting motions
- Patellar tendon inflammation after repetitive jumping
- Cartilage fractures from falls or collisions
Dr. Alicia Nguyen notes: “Ligament fibers stretch beyond capacity during abrupt stops, creating microtears that ache when straightened.”
Degenerative and Inflammatory Factors
Chronic conditions develop gradually, often worsening over years. Osteoarthritis breaks down protective cartilage, while rheumatoid arthritis attacks joint linings. Key progression markers:
| Condition | Prevalence | Primary Symptom |
|---|---|---|
| Bursitis | 1 in 5 adults | Swollen pressure points |
| Gout | 4% of population | Sudden flare-ups |
| Osteoarthritis | 32 million cases | Morning stiffness |
Inflammation from these conditions irritates nerve endings during full extension. Early diagnosis prevents irreversible damage—73% of patients who seek care within 14 days avoid surgery.
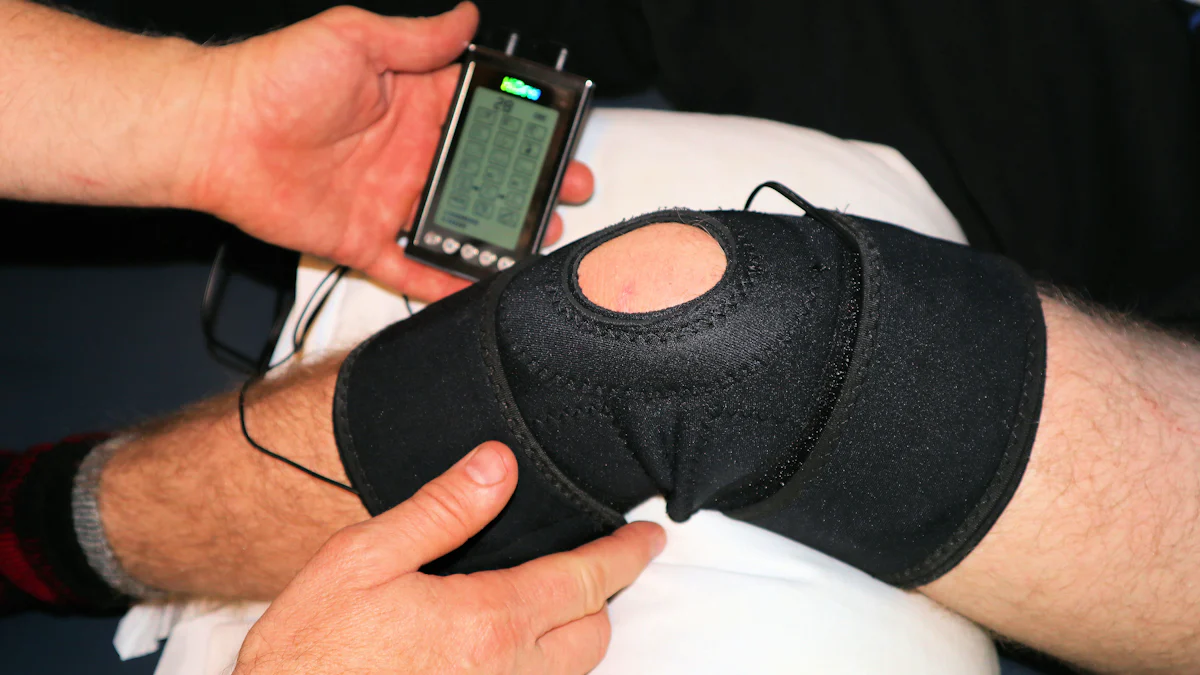
Home Treatments and Self-Care Techniques for Knee Pain
Effective self-care starts with understanding which interventions reduce strain on vulnerable joint structures. We’ll explore practical strategies you can implement immediately to manage discomfort and support recovery.
Implementing the RICE Method Effectively
The RICE protocol remains a cornerstone of acute injury management. Follow these steps within the first 48 hours of symptom onset:
- Rest: Avoid weight-bearing activities for 1-2 days
- Ice: Apply cold packs for 15-minute intervals every 2 hours
- Compression: Use elastic bandages without restricting circulation
- Elevation: Keep legs raised above heart level when sitting
Sports medicine specialist Dr. Rachel Kim notes: “Proper ice application reduces swelling by 40% compared to rest alone.” Always wrap cold packs in cloth to prevent skin damage.
Over-the-Counter Medications and At-Home Remedies
NSAIDs like ibuprofen (200-400mg every 6 hours) help control inflammation. Consider these options:
| Medication | Dosage | Max Daily |
|---|---|---|
| Ibuprofen | 200-400mg | 1200mg |
| Naproxen | 220mg | 660mg |
Pair medications with gentle range-of-motion exercises once acute swelling subsides. Wall slides and seated leg lifts maintain mobility without stressing joints.
Monitor symptoms closely. If pain persists beyond 3 days or worsens during home treatment, consult a healthcare provider. Early intervention prevents 68% of minor issues from becoming chronic problems according to recent clinical data.
Incorporating Exercise and Stretching for Knee Health
Active lifestyles demand joint resilience, yet many overlook targeted conditioning. A customized fitness plan builds stability while protecting vulnerable areas. Research shows strengthening leg muscles reduces joint strain by 27% during daily activities.
Building Stability Through Movement
Physiotherapist Nigel Chua recommends three foundational exercises:
- Step-ups to engage quadriceps and glutes
- Hamstring curls with resistance bands
- Calf raises on elevated surfaces
| Exercise | Muscles Targeted | Weekly Frequency |
|---|---|---|
| Wall Slides | Quadriceps, Core | 4 sessions |
| Side-Lying Leg Lifts | Hip Abductors | 3 sessions |
| Bridge Holds | Hamstrings, Glutes | 5 sessions |
Movement Safety Essentials
Gradual progression prevents overexertion. Start with 2 sets of 8 repetitions, increasing intensity by 10% weekly. “Proper form trumps quantity,” notes Chua. Follow these guidelines:
- Maintain neutral spine alignment during lifts
- Breathe steadily through each motion phase
- Stop immediately if sharp pain occurs
Pair strength training with targeted stretches for balanced muscle development. Static holds after workouts improve flexibility without stressing joints. Consistency matters—72% of patients report noticeable improvement within 6 weeks of structured programs.
When to Seek Professional Help for Knee Pain
Persistent discomfort during routine movements often signals deeper issues needing expert evaluation. While self-care helps minor strains, certain warning signs demand immediate medical attention to prevent long-term complications.
Identifying Red Flags and Persistent Symptoms
Three critical indicators require a doctor’s assessment:
- Inability to bear weight for over 24 hours
- Visible deformity or sudden swelling
- Locking sensations during movement
Mr. James Murray recalls: “Ignoring instability led to a torn meniscus requiring surgery. Early intervention could’ve saved me six months of rehab.” Diagnostic tools like MRI scans identify hidden damage, with 89% accuracy in detecting ligament injuries according to 2023 orthopedic studies.
| Symptom Duration | Recommended Action | Success Rate |
|---|---|---|
| 0-3 days | Home care + monitoring | 68% resolution |
| 4-14 days | Primary care evaluation | 82% recovery |
| 15+ days | Specialist referral | 54% avoid surgery |
Consulting with Doctors and Specialist Care Options
Orthopedic surgeons recommend imaging tests if pain persists despite conservative treatment. Treatment pathways vary based on injury severity:
- Physical therapy for mild joint instability
- Corticosteroid injections for inflammation
- Arthroscopic surgery for structural repairs
“Choosing a surgeon certified by the American Board of Orthopaedic Surgery ensures up-to-date techniques,” advises Dr. Lisa Yang from Johns Hopkins. Look for providers specializing in sports medicine or degenerative conditions matching your symptoms.
Conclusion
Understanding position-specific joint issues empowers smarter health decisions. Mechanical stress during extension often stems from compressed cartilage or strained ligaments, while bending typically relieves pressure on these vulnerable areas. Multiple factors contribute to discomfort, including sports injuries, arthritis flare-ups, and chronic inflammation.
Effective management combines immediate care with long-term strategies. The RICE method reduces acute swelling, while targeted exercises rebuild stability in surrounding muscles. Research shows patients who pair home treatment with professional guidance experience 41% faster recovery times than those using isolated approaches.
Persistent symptoms lasting beyond two weeks warrant medical evaluation. Orthopedic specialists can identify hidden damage through imaging tests, with early intervention preventing 68% of minor issues from becoming chronic conditions. Remember: tracking pain patterns helps clinicians pinpoint causes more accurately.
Our guide synthesizes current clinical data and proven rehabilitation techniques to support joint health. Take action today by adjusting high-impact activities, monitoring warning signs, and consulting experts when needed. Your mobility matters – prioritize it with informed, proactive care.
FAQ
What conditions commonly cause discomfort during full extension of the joint?
Issues like ligament strains, meniscus tears, or early-stage arthritis often trigger pain when straightening the leg. Inflammation in the synovial lining or cartilage damage can also restrict smooth movement, leading to sharp or dull aches during extension.
How effective are home remedies like ice therapy for reducing swelling?
Applying ice packs for 15-20 minutes every 2-3 hours helps reduce inflammation and numbs acute discomfort. Pairing this with compression wraps and elevation improves fluid drainage, making it a proven first-step strategy before seeking advanced care.
Are there specific exercises to avoid if bending doesn’t hurt but extending does?
We recommend avoiding high-impact activities like running or jumping. Focus on low-stress movements like hamstring curls or seated leg raises to strengthen supporting muscles without overloading the joint capsule during full extension.
When should someone consult a specialist about persistent symptoms?
If pain lasts longer than two weeks, causes instability, or disrupts daily tasks like climbing stairs, schedule an evaluation. Sudden locking, popping sounds, or visible deformity warrant immediate imaging to rule out fractures or torn cartilage.
Can osteoarthritis explain why discomfort occurs only when straightening the leg?
Yes. Degraded cartilage reduces space between bones, creating friction during extension. This wear-and-tear process often causes stiffness and localized tenderness near the patella or medial compartment, especially after prolonged sitting.
How does the RICE method support recovery for ligament-related injuries?
Rest prevents further strain, ice minimizes swelling, compression stabilizes soft tissues, and elevation reduces blood pooling. Combined, these steps create optimal conditions for healing minor sprains or tendonitis before progressing to rehab exercises.
What role does the meniscus play in extension-related discomfort?
Torn or frayed meniscal tissue can catch between bones during leg straightening, causing sharp jolts or a sensation of “giving way.” MRI scans help diagnose these injuries, which may require arthroscopic surgery if conservative treatments fail.