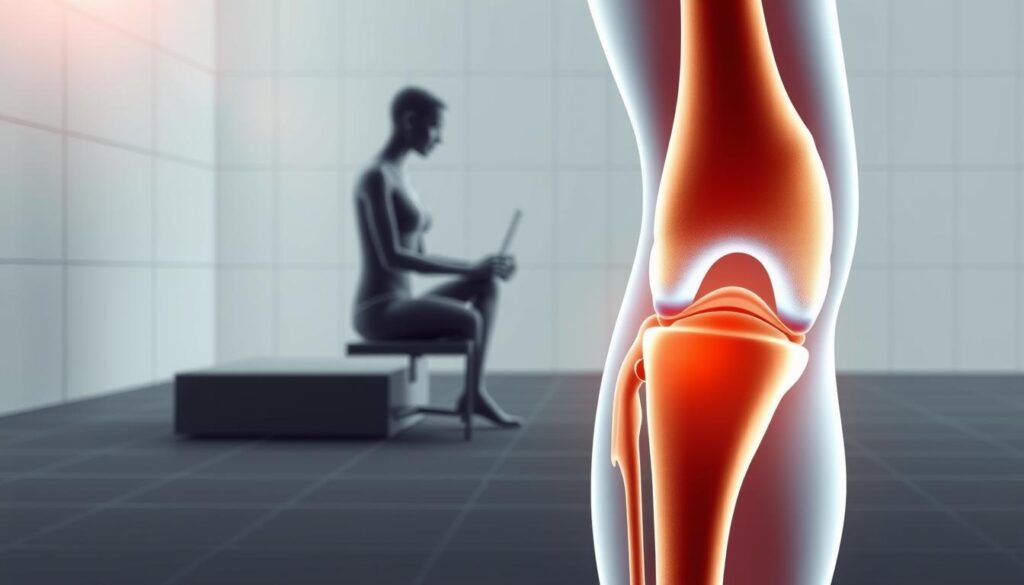
Have you ever climbed down a ladder and felt a sharp pain in your knees? You’re not alone. Many people feel knee pain when climbing down stairs or ladders. But what causes this discomfort?
It’s important to understand how our knees move. When we go down ladders, our knees take the impact of each step. This can cause pain and discomfort, especially for those who climb ladders often.
We’ll look into why knee pain happens when going down ladders. We’ll also talk about how to prevent and ease this pain.
Key Takeaways
- Understanding knee mechanics is key to addressing knee pain.
- Descending ladders puts strain on the knee joint.
- Frequent ladder climbing can lead to increased knee pain.
- Proper techniques can help alleviate knee pain when descending ladders.
- Prevention is crucial to avoiding long-term knee damage.
Common Causes of Knee Pain When Descending Ladders

Many people feel knee pain after coming down from ladders. It’s important to know why this happens to avoid it. Climbing down ladders can be hard and puts a lot of stress on our knees.
There are several reasons why knee pain happens during this activity. Let’s look at the main causes.
Pressure on the Joints
Our knees take a lot of our body weight when we go down a ladder. This can wear down the cartilage and cause pain. People with existing knee problems find this especially hard.
Muscle Fatigue
Muscle fatigue is another big reason for knee pain when coming down ladders. Tired leg muscles can’t support our knees well, leading to more strain. This can happen if we use our legs too much or don’t exercise them enough.
Poor Footwear
Wearing poor footwear can also lead to knee pain. Shoes that don’t support well or have worn-out soles can make our gait worse. It’s important to wear shoes that support and stabilize our feet.
To avoid knee pain, we need to tackle these issues. Knowing the causes helps us take steps to prevent pain and make ladder descent safer.
To lessen knee pain, we can strengthen our leg muscles, wear the right shoes, and pay attention to our ladder descent technique. By doing these things, we can lower the risk of knee pain and make our experience safer.
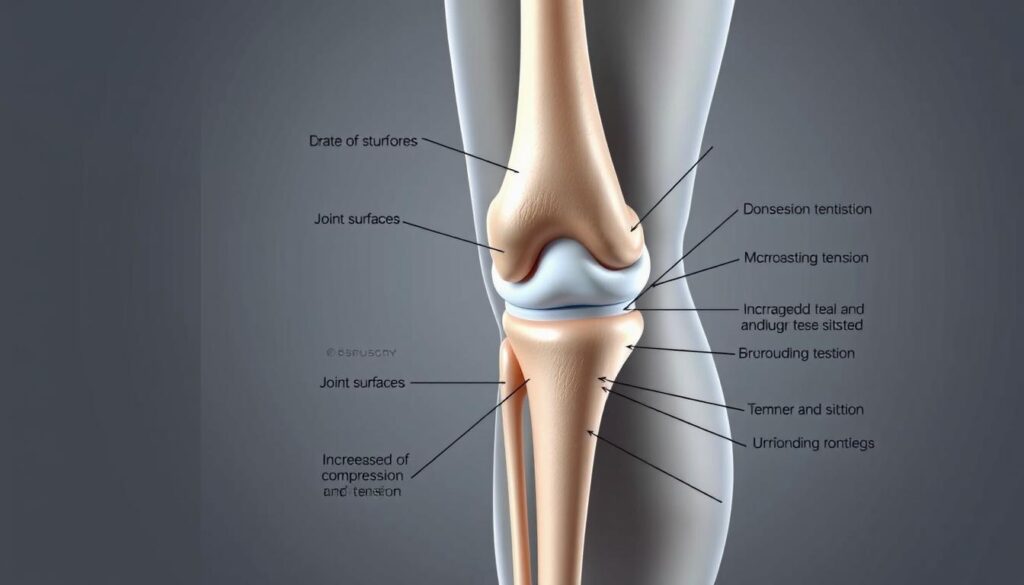
Anatomy of the Knee and Its Mechanics
When we go down ladders, our knees face a lot of stress. It’s key to know how the knee works. The knee is a complex hinge joint. It connects the lower thigh bone (femur) to the upper shin bone (tibia).
Key Components of the Knee Joint
The knee has several important parts that help it move. These parts are:
- The femur and tibia, the main bones of the knee.
- The patella (kneecap), at the front of the knee.
- Ligaments, which link bones together.
- Tendons, which connect muscles to bones.
- Cartilage, which cushions the joint.
Knowing these parts helps us understand how the knee works. This is especially true when we’re going down ladders.
How Descending Affects Knee Alignment
Going down a ladder puts a lot of stress on our knees. Keeping the knee aligned right is key for its health. But, going down ladders can sometimes mess with this alignment.
| Activity | Effect on Knee Alignment | Potential for Discomfort |
|---|---|---|
| Descending Ladders | Increased stress on knee joint | High |
| Proper Ladder Technique | Maintains optimal knee alignment | Low |
| Poor Ladder Technique | Disrupts knee alignment | High |
Knowing how ladders affect knee alignment helps us avoid pain. We can use the right techniques and keep our knees healthy.
Keeping the knee aligned right is key to avoiding pain on stairs or ladders. By focusing on knee injury prevention descending ladders, we can lower the risk of knee problems.
The Role of Technique in Preventing Pain

Using the right technique is key to avoiding knee pain when using ladders. The way we go down ladders can either help or hurt our knees. By using the best techniques, we can lower the chance of knee pain.
Proper Ladder Techniques
It’s important to use the right ladder techniques to avoid knee strain. Always face the ladder when going down, keep three points of contact, and stay centered between the side rails.
- Face the ladder when descending to maintain control and balance.
- Maintain three points of contact to reduce the risk of slipping.
- Keep your body centered between the side rails to avoid putting extra strain on your knees.
How to Position Your Feet
How you place your feet is crucial for knee safety. When going down a ladder, put your feet in a way that spreads your weight evenly. This means:
- Placing your feet in the center of the rungs to maintain balance.
- Avoid standing on the top rung, as this can cause instability.
- Keeping your knees slightly bent to absorb the impact of each step.
By following these tips, we can lessen knee strain and lower the risk of pain when using ladders. Remember, being careful with our technique can also prevent other injuries.
Strengthening Exercises for Knee Health
To avoid knee pain when going down stairs or ladders, it’s key to focus on exercises that strengthen the knee. Building muscle around the knee joint can lessen the strain during descent. This helps reduce pain.
Effective Strengthening Exercises
Doing specific exercises can make the muscles around the knee stronger. This gives better support and lowers injury risk. Some top exercises include:
- Straight Leg Raises: This targets the quadriceps, which is key for knee stability.
- Hamstring Curls: Strengthening the hamstrings helps balance muscle strength around the knee.
- Wall Squats: This strengthens the quadriceps, hamstrings, and gluteal muscles. All are crucial for knee health.
Doing these exercises often can make the knee more stable. It also reduces pain from going down stairs or ladders.
The Importance of Flexibility and Stretching
Strengthening exercises are not the only thing. Keeping flexible and stretching also supports knee health. Stretching improves range of motion, lowering stiffness and injury risk.
Some good stretches include:
- Quad Stretch: Stand with one hand on a wall for balance. Bend one knee and grab your ankle. Pull your heel towards your buttocks until you feel a stretch.
- Hamstring Stretch: Sit on the floor with legs straight out. Lean forward, reaching for your toes, and keep knees straight.
Combining strengthening exercises with flexibility and stretching can greatly improve knee health. It also reduces pain when going down stairs or ladders.
When to Seek Professional Help
Many times, knee pain from ladders can be fixed with simple steps and care. But, some cases need a doctor’s help. Knowing why your knee hurts on ladders helps decide what to do next.
Identifying Serious Injuries
Some signs mean you need to see a doctor right away. Severe pain, swelling, or feeling unstable in your knee are red flags. Knowing these signs helps avoid more harm and ensures you heal right.
Exploring Treatment Options
There are many ways to treat knee pain from ladders. Why does it hurt? Knowing this helps pick the best treatment. Options range from physical therapy to medical treatments. Understanding these choices helps you find the right care for your knee.
FAQ
Why do knees hurt when descending ladders?
Knees hurt when descending ladders because of the pressure on the joints. Muscle fatigue and poor footwear also play a role. These factors can disrupt the knee’s natural alignment and function.
What are the common causes of knee pain on ladders?
Common causes include pressure on the joints and muscle fatigue. Poor footwear is another factor. All these can lead to knee discomfort or pain when descending ladders.
How can I prevent knee pain when climbing down stairs or ladders?
To prevent knee pain, use proper ladder techniques and wear suitable footwear. Keeping muscles around the knee strong through exercises and stretching routines is also important.
What role does technique play in preventing knee pain on ladders?
Technique is crucial in preventing knee pain. It ensures a smooth and controlled descent. This minimizes strain on the knees.
Are there exercises that can help alleviate knee pain when descending ladders?
Yes, exercises that strengthen the muscles around the knee can help. Flexibility and stretching routines also play a role. They can alleviate knee pain and improve knee health.
When should I seek professional help for knee pain when descending ladders?
Seek professional help if you have severe pain, swelling, or instability. These signs may indicate a serious injury. They may need medical attention and treatment.
What are the potential treatments for knee pain caused by descending ladders?
Treatments include physical therapy and medication for pain relief. In some cases, surgery may be necessary. The choice depends on the cause and severity of the knee pain.
How can I maintain healthy knees to avoid pain when using ladders?
To keep knees healthy, exercise regularly and wear proper footwear. Using correct techniques when descending ladders is also key. These steps can help prevent knee pain and discomfort.