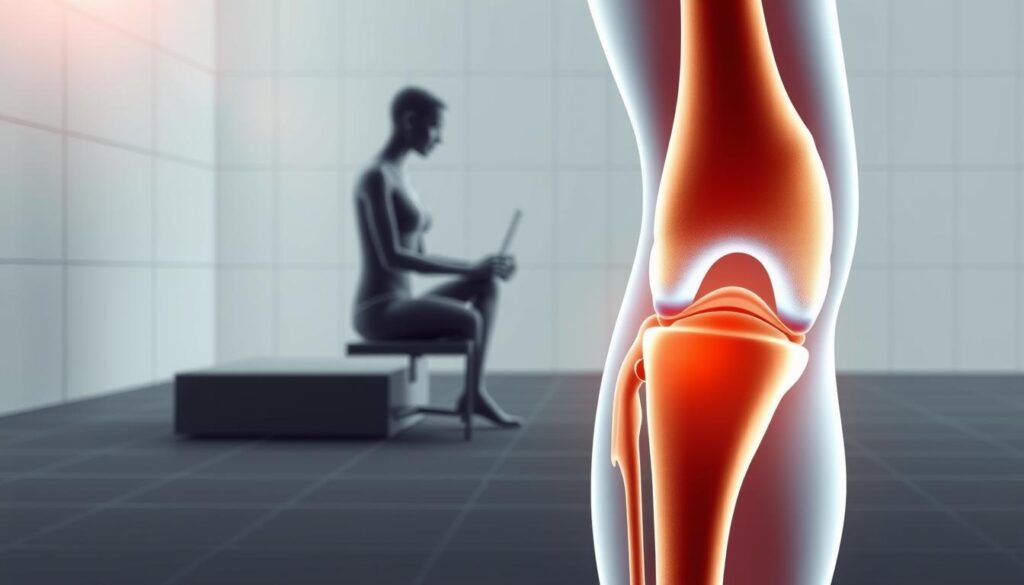
Knee pain affects millions of Americans, limiting mobility and diminishing quality of life. Whether you’re dealing with arthritis, sports injuries, or age-related wear and tear, finding effective relief can feel overwhelming amid countless products promising miraculous results. The impact goes beyond physical discomfort—it can prevent you from enjoying favorite activities, disrupt sleep, and even lead to dependency on pain medications.
The good news? Science-backed solutions do exist. This comprehensive guide cuts through marketing hype to present knee pain relief products with proven effectiveness. Drawing on clinical research and expert recommendations, we’ve identified options that deliver meaningful results for different types of knee pain. From compression sleeves to topical treatments, we’ll help you navigate the choices and find solutions that can get you back to living comfortably.
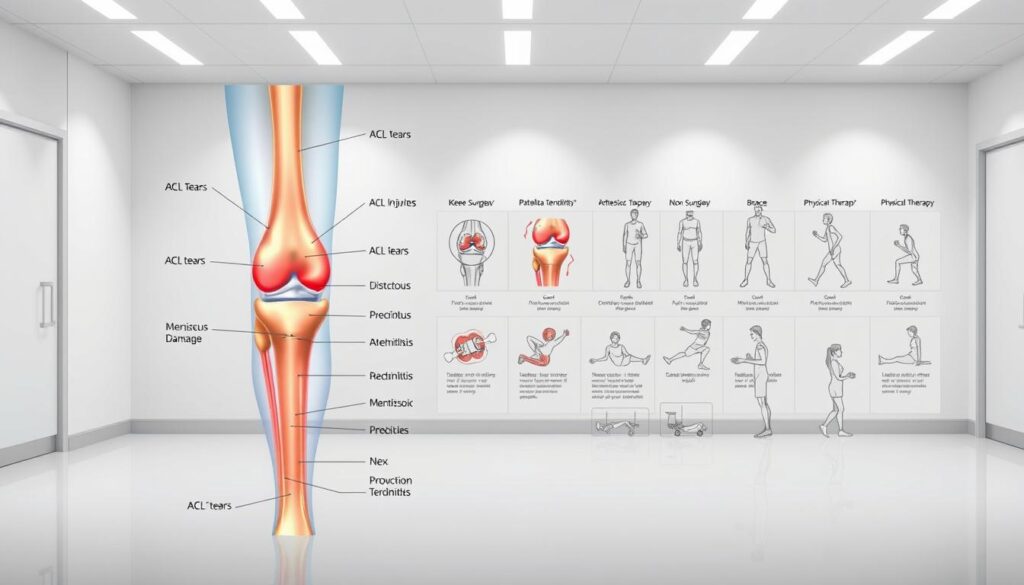
Types of Knee Pain Relief Products
Knee pain relief products come in various forms, each targeting different aspects of pain management. Understanding these categories will help you identify which solutions might work best for your specific condition and lifestyle needs.

- Compression Sleeves and Braces: These provide stability and support to the knee joint, reducing pressure and improving alignment. They range from simple elastic sleeves to more structured braces with hinges and straps.
- Topical Creams and Gels: Applied directly to the skin, these products deliver pain-relieving ingredients like menthol, capsaicin, or NSAIDs directly to the affected area, often providing quick temporary relief.
- Oral Supplements: Ingredients like glucosamine, chondroitin, turmeric, and omega-3 fatty acids may help reduce inflammation and support joint health when taken regularly.
- Cold and Heat Therapy Tools: Ice packs reduce inflammation and swelling, while heat therapy improves circulation and relaxes muscles. Specialized wraps and devices are designed specifically for knee application.
- Supportive Footwear and Insoles: Proper foot support can significantly impact knee alignment and reduce pain, especially for those with flat feet or overpronation issues.
- TENS Units: These devices use electrical stimulation to disrupt pain signals and provide temporary relief for chronic knee pain conditions.
Each category offers unique benefits, and many people find that combining approaches provides the most comprehensive relief. Let’s examine the top-performing products in each category that have demonstrated real results for knee pain sufferers.
Top 5 Knee Pain Relief Products That Deliver Results
After analyzing clinical studies, expert recommendations, and user experiences, we’ve identified five standout products that consistently deliver effective knee pain relief. These selections represent the best options across different categories.

| Product | Type | Key Features | Pros | Cons |
| Voltaren Arthritis Pain Gel | Topical NSAID | 1% diclofenac sodium, non-greasy formula, prescription-strength now available OTC | Clinically proven to reduce inflammation, targets pain directly, minimal systemic absorption | Requires multiple daily applications, may take 7+ days for maximum effect |
| Copper Fit Compression Knee Sleeve | Compression Support | Copper-infused compression fabric, contoured fit, moisture-wicking material | Provides stability while maintaining mobility, comfortable for all-day wear, machine washable | Compression level may be insufficient for severe instability, sizing can be challenging |
| Biofreeze Pain Relief Gel | Topical Analgesic | 4% menthol, cold therapy effect, available in gel, spray, and roll-on formats | Fast-acting relief, cooling sensation masks pain, doesn’t stain clothing, long-lasting effect | Temporary symptom relief rather than treating underlying causes, strong menthol scent |
| Dr. Scholl’s Knee Pain Relief Orthotics | Supportive Insoles | Shock Guard technology, arch support, designed specifically for knee pain | Improves alignment from feet up, fits in most shoes, helps with pain from walking/standing | May not fit in all footwear, requires breaking-in period, less effective for severe misalignment |
| Move Free Ultra Triple Action Joint Supplement | Oral Supplement | Glucosamine, chondroitin, hyaluronic acid, and boron combination | Supports joint structure and cartilage health, once-daily dosing, comprehensive formula | Takes weeks to notice effects, mixed scientific evidence, relatively expensive |
1. Voltaren Arthritis Pain Gel

Voltaren stands out as one of the few topical products with substantial clinical evidence supporting its effectiveness for arthritis pain. This diclofenac sodium gel works by targeting inflammation directly at the source, rather than just masking pain sensations.
What makes Voltaren particularly effective is its ability to penetrate the skin and reach the painful joint without significant systemic absorption, reducing the risk of side effects associated with oral NSAIDs. Users report noticeable improvement in knee mobility and reduced pain within days of consistent use.
Experience Targeted Knee Pain Relief
Voltaren Gel delivers prescription-strength relief without a prescription. Apply 3-4 times daily for best results.
2. Copper Fit Compression Knee Sleeve

Copper Fit has gained popularity for combining moderate compression with copper-infused fabric. The compression element helps stabilize the knee joint and improve proprioception (your awareness of joint position), which can reduce pain during movement.
The sleeve provides gentle warmth that increases blood circulation to the area, potentially accelerating healing and reducing stiffness. Many users report that the sleeve allows them to remain active while managing pain, making it ideal for those who want to maintain their exercise routines despite knee discomfort.
Stay Active With Knee Support
Copper Fit sleeves provide all-day comfort and support without restricting movement. Available in multiple sizes.
3. Biofreeze Pain Relief Gel

Biofreeze utilizes cold therapy through its active ingredient menthol to create a cooling sensation that interrupts pain signals. This approach, known as “gate control theory,” essentially distracts the nervous system from transmitting pain messages to the brain.
What distinguishes Biofreeze from other menthol products is its long-lasting formula and variety of application methods. The roll-on and spray options make it particularly convenient for targeting knee pain without messy application. Athletes and physical therapists frequently recommend Biofreeze for its ability to provide quick relief before or after physical activity.
Experience Fast-Acting Cooling Relief
Biofreeze provides immediate cooling sensation that blocks pain signals. Available in gel, spray, or roll-on formats.
4. Dr. Scholl’s Knee Pain Relief Orthotics

Many people don’t realize that knee pain often stems from improper foot alignment. Dr. Scholl’s Knee Pain Relief Orthotics address this root cause by providing arch support and shock absorption that helps align the entire leg from the ground up.
These insoles are specifically designed to reduce the load on the knees during walking and standing. The shock-absorbing technology helps minimize impact forces that can aggravate knee pain, while the arch support promotes proper biomechanical alignment. Users with mild to moderate knee osteoarthritis often report significant improvement in pain levels during daily activities.
Address Knee Pain from the Ground Up
Dr. Scholl’s orthotics improve alignment and reduce impact forces that contribute to knee pain. Fits most shoes.
5. Move Free Ultra Triple Action Joint Supplement

For those seeking a long-term approach to knee pain management, Move Free Ultra combines three key ingredients that support joint structure and function. Glucosamine and chondroitin have been studied extensively for their potential to maintain cartilage health, while hyaluronic acid helps with joint lubrication.
What sets this supplement apart is the addition of boron, which research suggests may help reduce inflammation and improve the body’s use of other nutrients important for joint health. While supplements generally take longer to show effects than topical treatments, many users report improved mobility and reduced discomfort after 4-6 weeks of consistent use.
Support Long-Term Joint Health
Move Free’s comprehensive formula supports cartilage, lubricates joints, and reduces inflammation with just one pill daily.
How to Choose the Right Knee Pain Relief Product
Selecting the most effective knee pain solution depends on several factors unique to your situation. Consider these key criteria when making your decision:

Pain Severity and Type
- Mild pain: Topical treatments like Biofreeze may be sufficient
- Moderate pain: Combination of compression and topical NSAIDs
- Severe pain: Structured braces plus multiple treatment approaches
- Inflammatory pain: Products with anti-inflammatory properties
- Mechanical pain: Support products that improve alignment
Activity Level and Goals
- Active lifestyle: Flexible support that doesn’t restrict movement
- Sports participation: Sport-specific braces with lateral support
- Daily activities: Comfortable all-day solutions
- Sedentary needs: Focus on alignment and circulation
- Recovery focus: Comprehensive approach with multiple products
Practical Considerations
- Budget: Balance cost with effectiveness and durability
- Application ease: Consider your mobility limitations
- Allergies: Check ingredients for potential sensitivities
- Clothing compatibility: Will it work with your wardrobe?
- Lifestyle fit: Choose products you’ll actually use consistently
Always consult with a healthcare provider before starting any new treatment regimen, especially if you have underlying health conditions or take other medications. Your doctor can help identify the source of your knee pain and recommend appropriate products based on your specific diagnosis.
“The most effective approach to knee pain relief often involves combining multiple strategies. For example, using a topical anti-inflammatory during the day, wearing a supportive brace during activity, and applying cold therapy after exertion.”
Lifestyle Tips to Enhance Knee Pain Relief
While the right products can significantly reduce knee pain, combining them with appropriate lifestyle modifications can maximize your results and promote long-term joint health.

- Low-impact exercises: Activities like swimming, cycling, and elliptical training strengthen muscles around the knee without excessive impact. Strong quadriceps and hamstrings provide better support for the knee joint.
- Weight management: Every pound of excess weight adds 4 pounds of pressure to your knees when walking. Even modest weight loss can significantly reduce knee pain and slow osteoarthritis progression.
- Proper stretching routines: Regular stretching improves flexibility and range of motion. Focus on quadriceps, hamstrings, and calf muscles to maintain proper knee alignment.
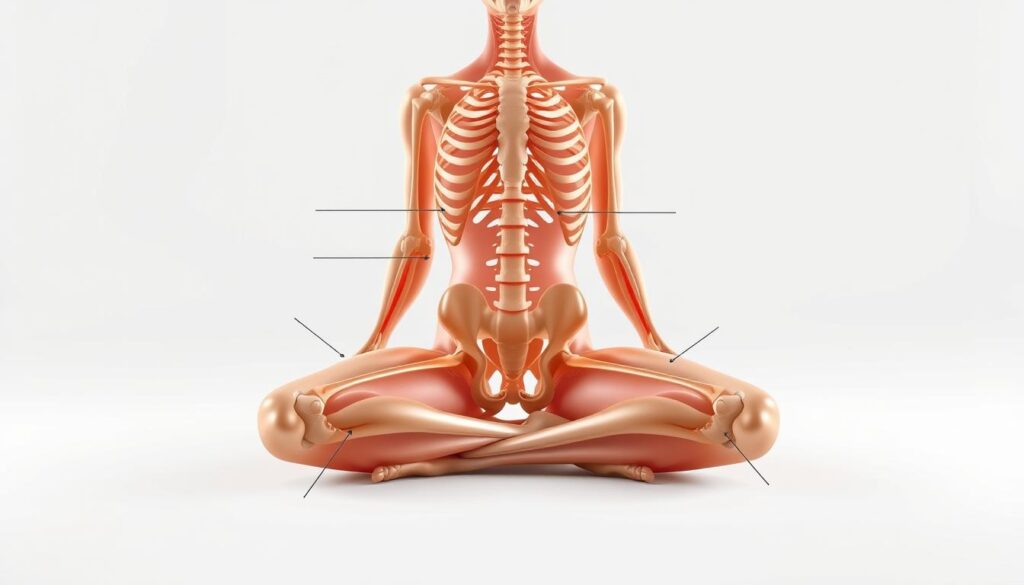
- Posture awareness: Poor posture can contribute to knee misalignment. Practice proper sitting, standing, and walking techniques to reduce unnecessary strain.
- Adequate hydration: Well-hydrated joints have better shock-absorbing capabilities. Aim for at least 8 glasses of water daily to support cartilage health.
Pro Tip: Create a consistent routine that combines your knee pain relief products with these lifestyle practices. For example, apply a topical treatment after your stretching routine, or wear your compression sleeve during low-impact exercise sessions.
Frequently Asked Questions About Knee Pain Relief

Do knee braces actually work for arthritis pain?
Yes, studies show that properly fitted knee braces can reduce pain and improve function in people with knee osteoarthritis. Braces work by offloading pressure from the damaged part of the joint, improving alignment, and providing proprioceptive feedback that helps with stability. The effectiveness depends on the type of brace and the specific arthritis condition. Unloader braces are particularly helpful for unicompartmental osteoarthritis (affecting just one side of the knee).
How long should I use ice versus heat for knee pain?
Ice is most effective for acute pain, swelling, and inflammation, typically within 48-72 hours after an injury or flare-up. Apply cold therapy for 15-20 minutes at a time, several times daily. Heat works better for chronic, stiff joints and muscle tension. Use heat therapy for 15-20 minutes before activity to increase flexibility. Never sleep with heating pads, and always place a thin towel between thermal therapies and your skin to prevent damage.
Can supplements really help with knee cartilage repair?
The evidence is mixed. Glucosamine and chondroitin have shown modest benefits in some studies, particularly for moderate to severe osteoarthritis pain. These supplements may help slow cartilage degradation rather than repair existing damage. Collagen peptides and omega-3 fatty acids show promising results in reducing inflammation and supporting joint health. Results typically take 2-3 months of consistent use, and effects vary significantly between individuals.
Are prescription options better than over-the-counter products?
Not necessarily. Many effective knee pain relief products are available over the counter, including Voltaren Gel (previously prescription-only). Prescription options may offer higher strengths or specialized formulations for severe cases. The best approach often combines OTC products with proper exercise, weight management, and occasional prescription interventions when needed. Always consult your healthcare provider to determine the most appropriate treatment plan for your specific condition.
Finding Your Ideal Knee Pain Solution
Effective knee pain management typically requires a multi-faceted approach. The products highlighted in this guide represent some of the most reliable options backed by scientific evidence and real-world effectiveness. Remember that what works best varies from person to person, and finding your ideal solution may involve some trial and error.

Start with addressing the underlying cause of your knee pain whenever possible. Combine targeted products with appropriate lifestyle modifications and proper medical guidance. For chronic or severe knee pain, always work with healthcare professionals who can help develop a comprehensive treatment plan that may include physical therapy, appropriate exercise, and periodic monitoring.
By taking a proactive approach to knee pain management with evidence-based products and healthy habits, you can significantly improve your mobility, reduce discomfort, and enhance your quality of life.
Take the First Step Toward Knee Pain Relief
Don’t let knee pain limit your life any longer. Start with one of our expert-recommended products and build your personalized relief strategy.