Did you know that patellofemoral pain syndrome (PFPS) affects up to 25% of the population and is a leading cause of patella pain when kneeling? If you frequently experience knee pain while kneeling or discomfort in the patella during kneeling, you’re not alone. Thankfully, there are effective strategies to alleviate this pain and regain comfort in your kneecap. In this article, we will explore the causes of patella pain when kneeling, the diagnosis process, non-surgical treatment options, surgical interventions, lifestyle modifications, and how to prepare for a medical appointment. Let’s discover ways to ease your patella woes and improve your knee health.
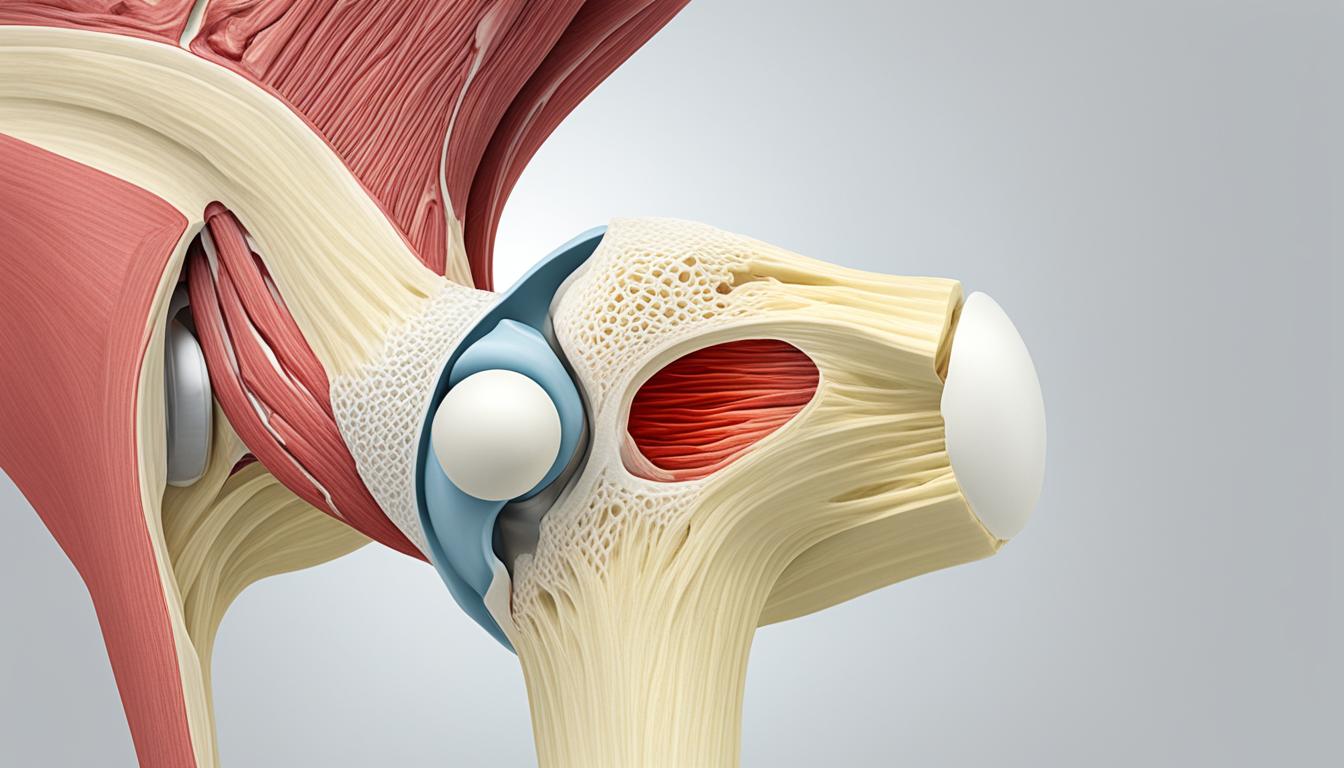
Understanding Patellofemoral Pain Syndrome
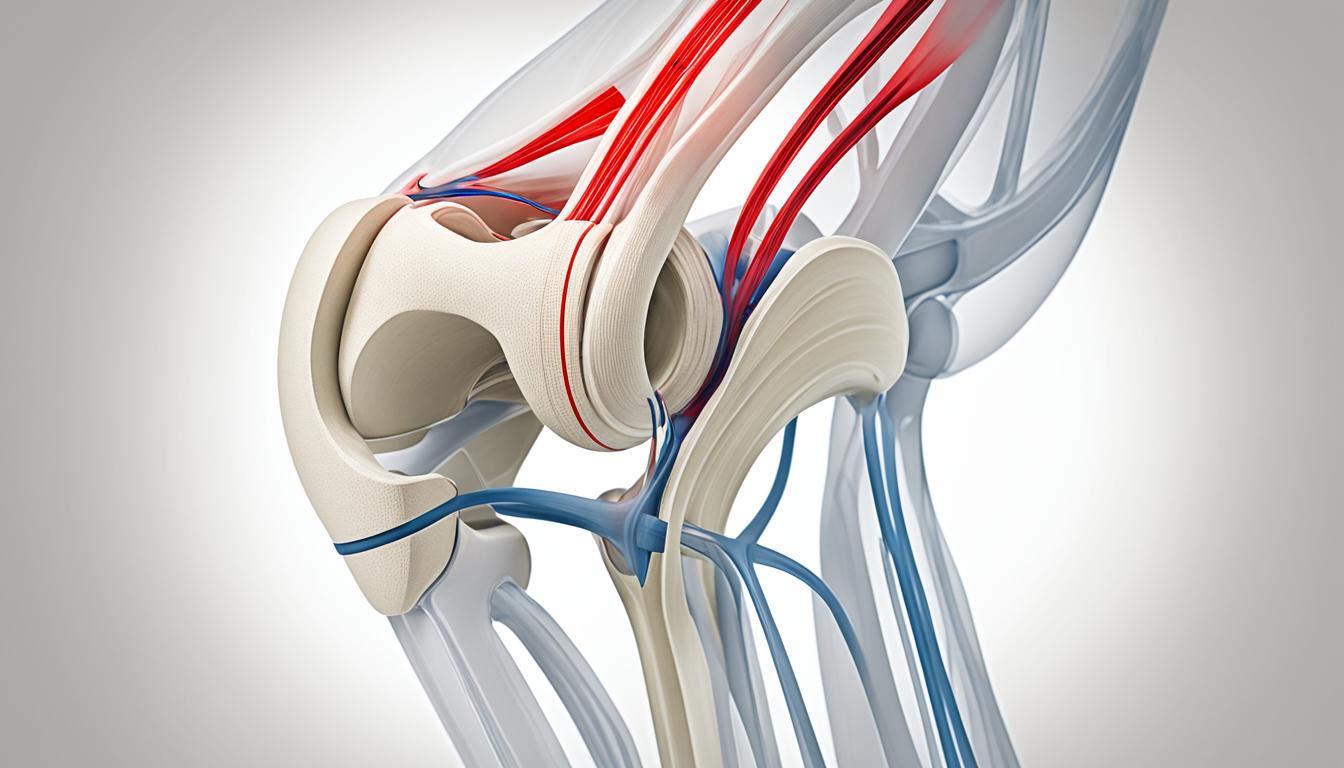
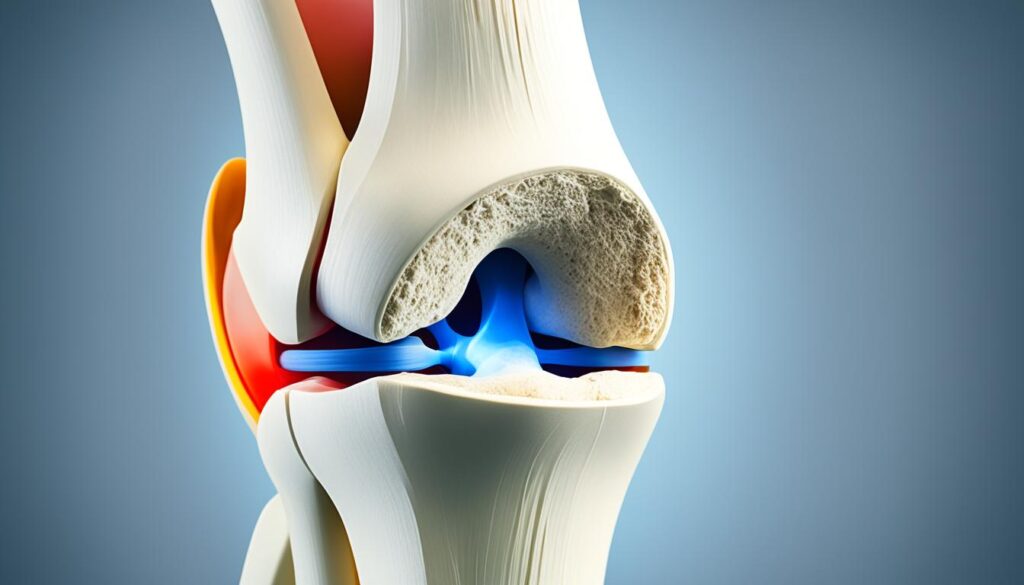
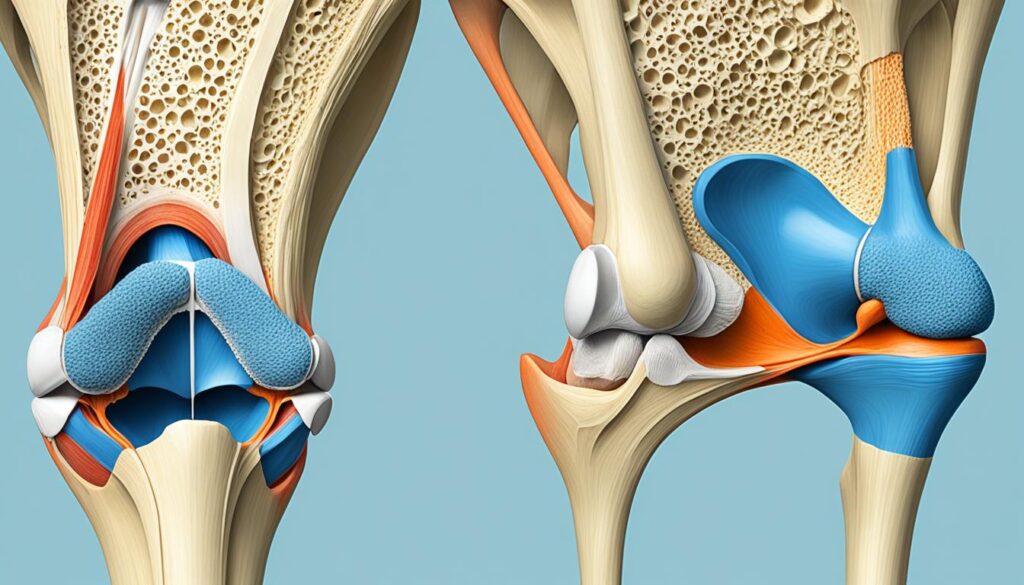
Patellofemoral pain syndrome (PFPS) is a common condition characterized by pain in the front of the knee and around the kneecap. It is often referred to as “runner’s knee” or “jumper’s knee” because it frequently affects athletes. PFPS can be caused by various factors, such as overuse, improper training techniques, changes in activity level, and alignment issues in the kneecap.
Individuals with PFPS may experience symptoms such as patella soreness when kneeling, pain in the knee when kneeling, and discomfort in the patella while kneeling. This can make simple tasks like kneeling or climbing stairs painful and challenging.
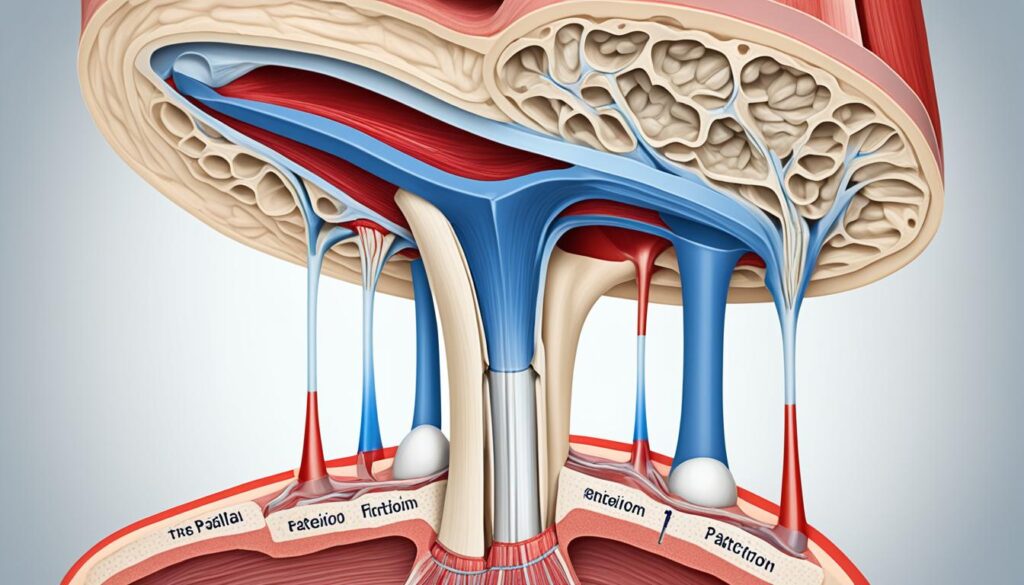
It is essential to understand the underlying causes of PFPS to effectively manage and alleviate the associated pain. Overuse and repetitive movements can lead to irritation and inflammation of the patellofemoral joint, resulting in discomfort and soreness. Inadequate biomechanics, such as poor alignment of the kneecap, can also contribute to the development of PFPS.
Correct diagnosis and identification of contributing factors are crucial for implementing appropriate treatment strategies. By addressing the root causes of patellofemoral pain syndrome and adopting targeted interventions, individuals can find relief and improve their knee health.

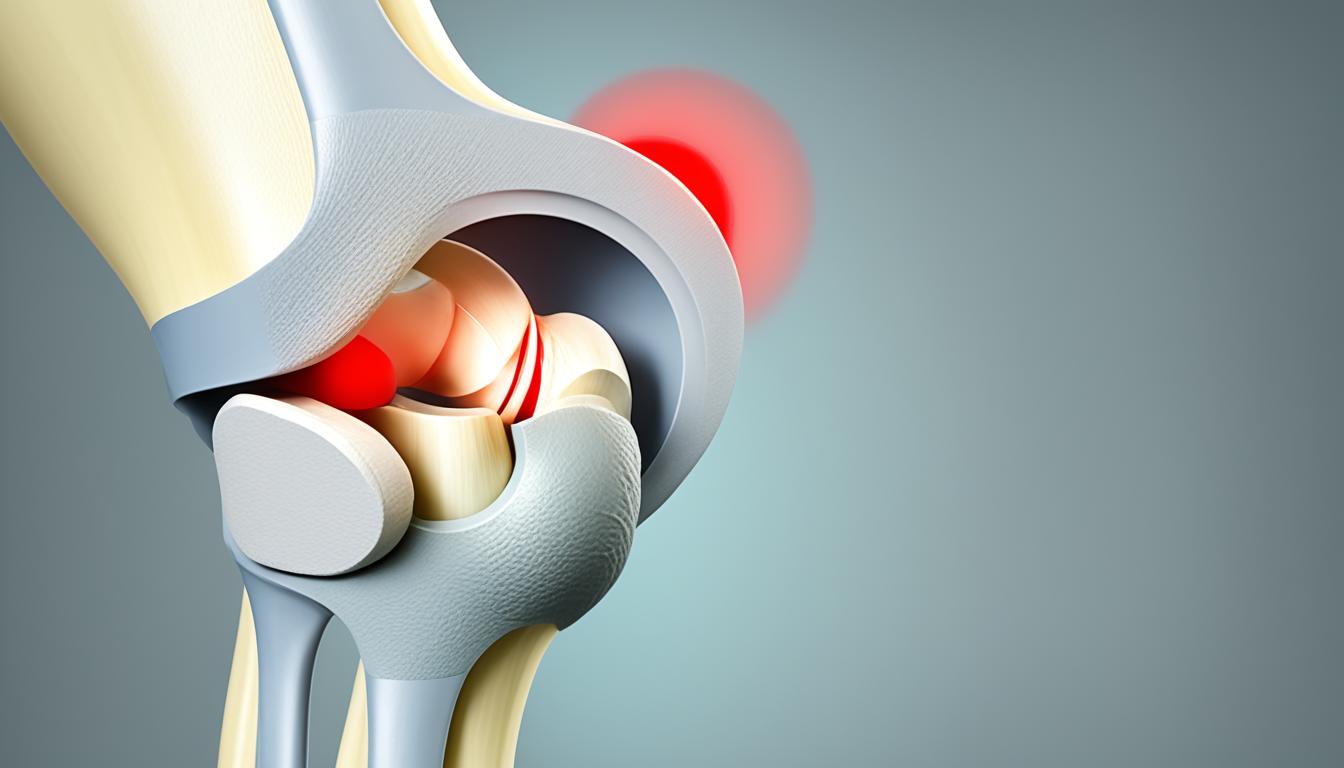
Diagnosing Patella Pain when Kneeling
When experiencing patella pain when kneeling, it is crucial to consult with healthcare providers for an accurate diagnosis. Through a comprehensive examination and consideration of the individual’s medical history, healthcare professionals can determine the underlying causes of knee discomfort. Diagnostic measures may include:
- Pressing on the knee to assess tenderness and pinpoint the source of pain
- Evaluating the range of motion to identify any limitations or restrictions
- Conducting imaging tests such as X-rays, CT scans, MRI, or ultrasound to evaluate the knee’s structure and detect potential abnormalities
These diagnostic procedures help healthcare providers understand the specific factors contributing to knee pain when bending down and soreness in the kneecap when kneeling. By identifying the root cause, healthcare professionals can develop an appropriate and effective treatment plan.
| Diagnostic Measures | Purpose |
|---|---|
| Examination and Medical History | To assess symptoms, identify risk factors, and understand the individual’s medical background |
| Compression and Palpation | To evaluate tenderness, location of pain, and potential soft tissue or ligament damage |
| Range of Motion Assessment | To identify limitations and assess the mobility of the knee joint |
| Imaging Tests (X-rays, CT scans, MRI, ultrasound) | To visualize the knee’s internal structures, identify structural abnormalities, and rule out other causes of pain |
By utilizing these diagnostic approaches, healthcare providers can accurately diagnose patella pain when kneeling and develop an appropriate treatment plan tailored to the individual’s needs.
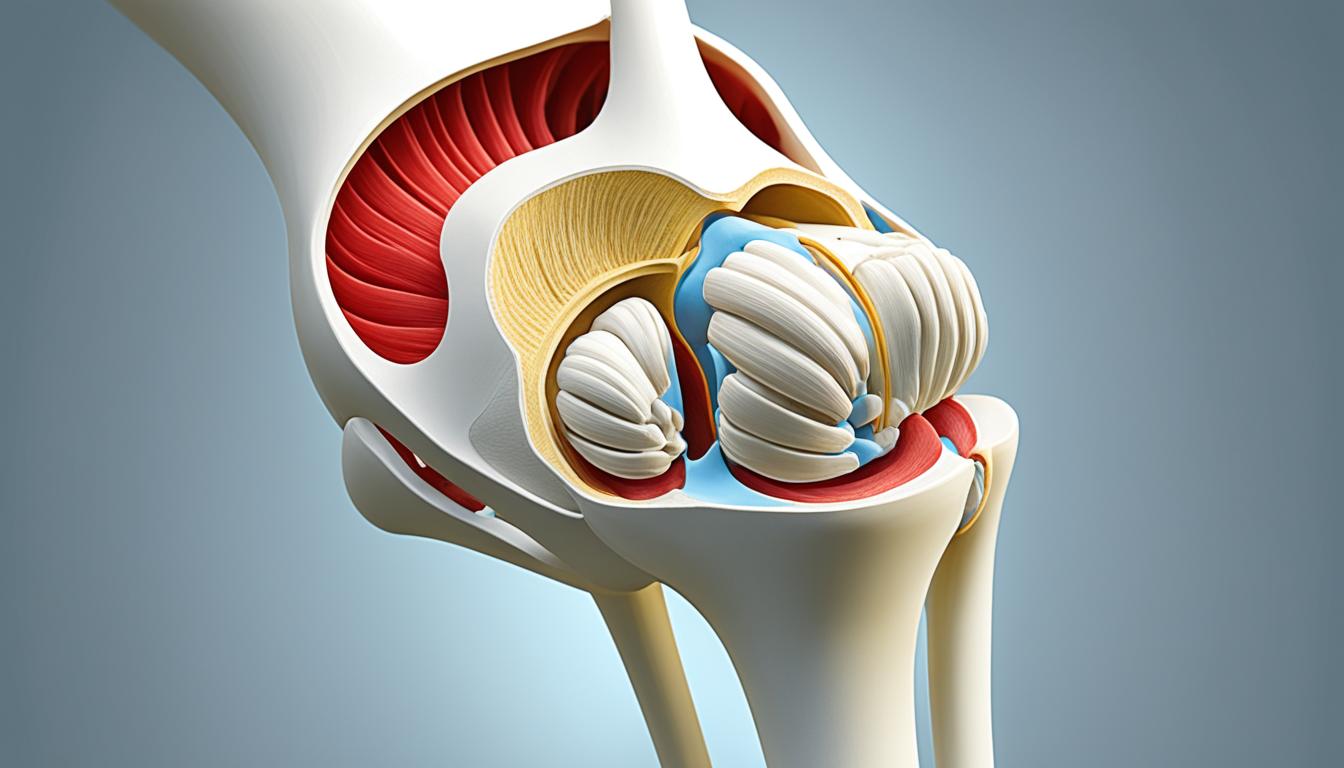
Non-surgical Treatment Options
In many cases, individuals experiencing patella pain when kneeling can find relief through non-surgical treatment options. These approaches aim to alleviate knee pain when bending down and reduce soreness in the kneecap during kneeling.
- Rest: Taking breaks from activities that worsen the pain can help the knee recover and prevent further strain.
- Pain relievers: Over-the-counter medications like acetaminophen or ibuprofen can provide temporary relief from knee discomfort.
- Rehabilitation exercises: Engaging in specific exercises to strengthen the muscles supporting the knees can help improve kneecap stability and reduce pain during activities like kneeling. It’s essential to consult a healthcare professional or a physical therapist to develop a customized exercise routine.
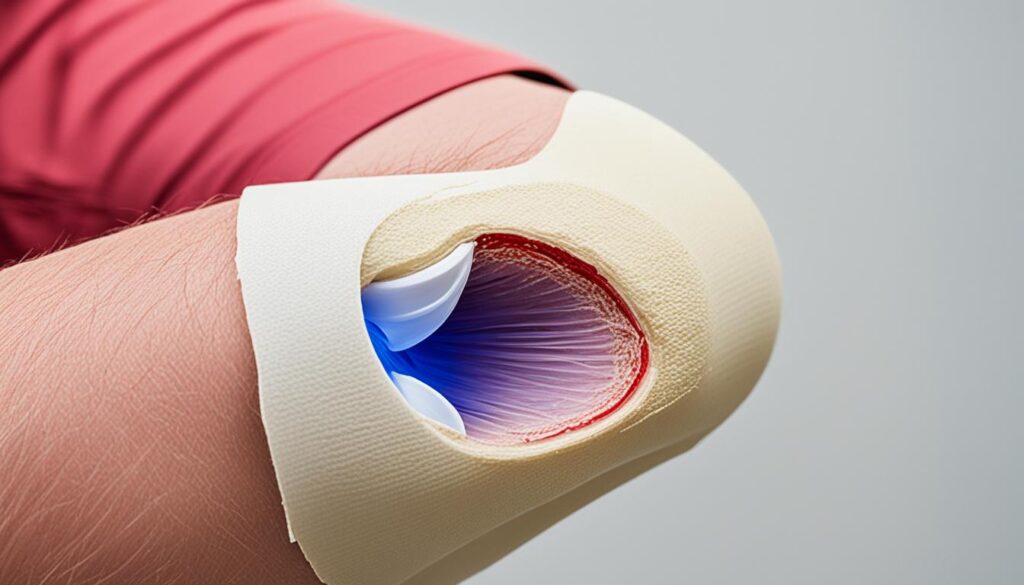
- Supportive braces and taping technique: Wearing knee braces or using taping techniques can provide additional stability to the knee joint and help reduce pain while kneeling.
- Icing: Applying ice packs to the knee for 15-20 minutes several times a day can help reduce inflammation and alleviate kneecap soreness.
- Orthotics: Using shoe inserts or orthotics designed to align and support the feet can help improve overall knee alignment and reduce strain on the kneecap.
Alongside these treatment options, engaging in knee-friendly sports can aid in the recovery process. Activities such as swimming or cycling are low-impact and place less stress on the knees, making them suitable choices to maintain fitness while minimizing strain.
“Non-surgical treatments like rest, exercises, and supportive braces can effectively relieve knee pain when bending down and alleviate soreness in the kneecap when kneeling.”
It’s important to consult with a healthcare professional to determine the most appropriate treatment approach based on individual needs and the underlying cause of patella pain. Combining these non-surgical options with proper self-care and lifestyle modifications can enhance knee health and facilitate a return to pain-free kneeling.”
Surgical and Other Procedures
If non-surgical treatments do not provide sufficient relief for patella pain when kneeling, healthcare providers may recommend surgical interventions. These procedures aim to address the underlying causes of the pain and improve knee health. Two common surgical procedures that are often utilized are arthroscopy and realignment surgeries.
Arthroscopy
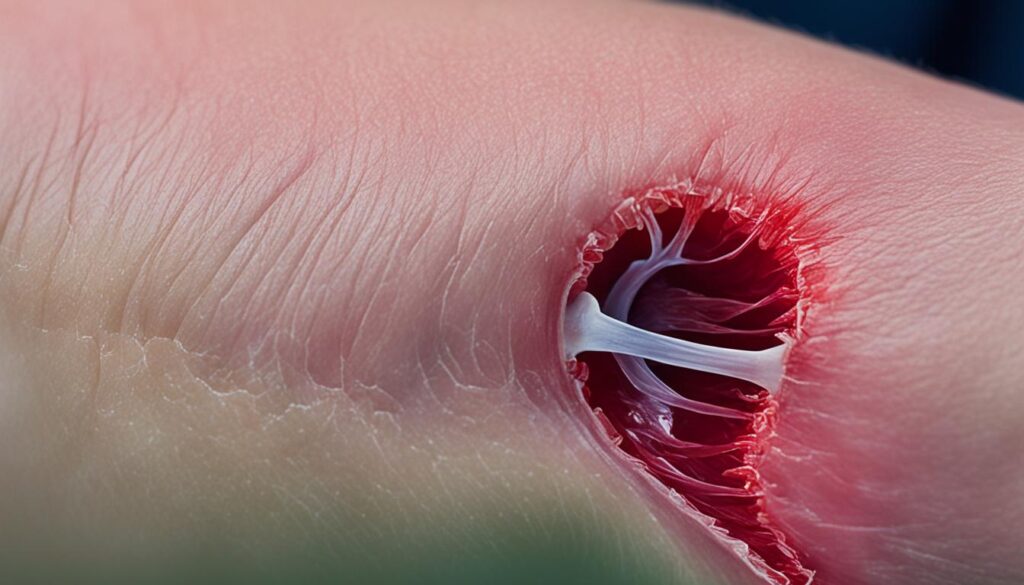
Arthroscopy is a minimally invasive procedure that allows surgeons to diagnose and treat various knee conditions. During this procedure, a surgeon inserts a camera and specialized tools into the knee joint through small incisions. The camera provides a clear view of the internal structures, allowing the surgeon to identify and repair any issues contributing to the patella pain when kneeling. Arthroscopy offers the advantage of reduced scarring, faster recovery time, and decreased postoperative pain compared to traditional open surgeries.
Realignment Surgeries
In more severe cases of patella pain when kneeling, realignment surgeries may be necessary. These procedures are designed to correct the alignment of the kneecap or alleviate pressure on the cartilage, thereby reducing pain and improving knee function. Realignment surgeries typically involve adjusting the position of the patella or altering the surrounding tissues to restore proper alignment. The specific technique used will depend on the individual’s condition and the underlying causes of their patella pain when kneeling. It is crucial to consult with a qualified healthcare provider to determine the most appropriate surgical option for addressing the specific case.
Lifestyle Modifications for Patella Pain Relief
Alongside medical interventions, individuals experiencing knee pain during kneeling or patellar pain with kneeling can make certain lifestyle modifications to find relief. By adopting these changes, you can actively manage and reduce discomfort in the patella area while performing daily activities.
Avoid activities that exacerbate the pain
Identify activities that worsen your knee pain during kneeling and try to avoid them whenever possible. This may include tasks that involve excessive bending of the knees or prolonged periods of kneeling. By recognizing and minimizing these triggers, you can help prevent further strain on the patella and alleviate discomfort.
Adopt proper techniques when kneeling or bending down
It is crucial to use proper techniques when performing tasks that require kneeling or bending down. Maintain a straight body posture, engage your core muscles, and distribute your weight evenly to minimize stress on the knees. If possible, use supportive knee pads or cushions to provide additional cushioning and support to the patella, reducing the impact and pressure on the knee joint.
Maintain a healthy weight
Excess body weight can put additional strain on the knees, leading to more pain and discomfort during activities that involve kneeling. By maintaining a healthy weight through a balanced diet and regular exercise, you can alleviate the pressure on your knees and reduce patellar pain when kneeling.
Engage in regular physical activity
Incorporating regular physical activity into your routine helps strengthen the muscles supporting the knees, providing better stability and reducing knee pain. Choose low-impact exercises such as swimming or cycling, which put less stress on the knees while offering effective cardiovascular benefits. Remember to consult with a healthcare professional before starting any new exercise program.
Preparing for a Medical Appointment
Before seeking medical advice for knee pain while kneeling or knee pain during kneeling, it is important to be prepared for the appointment. By organizing your thoughts and information, you can ensure a productive and efficient visit with your healthcare provider.
- Document your symptoms: Take note of when the knee pain occurs, the duration of each episode, and any triggers or activities that exacerbate the pain. This information will help your healthcare provider understand your specific situation.
- Provide relevant personal information: Inform your healthcare provider about any previous knee injuries or surgeries you have had. This information can shed light on potential underlying causes or predispositions to knee pain while kneeling.
- Bring copies of previous X-rays or imaging tests: If you have undergone any previous knee imaging tests, such as X-rays or MRIs, bring the copies with you to the appointment. These images can aid in the diagnosis and treatment planning process.
- Consider bringing a trusted companion: It can be beneficial to have a friend or family member accompany you to the appointment. They can help remember the information provided by the healthcare provider and provide additional support.
- Prepare a list of questions: Write down any questions or concerns you have about your knee pain while kneeling beforehand. This ensures that you address all your concerns during the appointment and have a clear understanding of your condition and treatment options.
By following these preparatory steps, you can maximize the effectiveness of your medical appointment and facilitate a thorough evaluation of your knee pain while kneeling or knee pain during kneeling.
Note: The image above depicts potential methods for knee pain relief and is for illustrative purposes only.
Conclusion
Patella pain when kneeling can have a significant impact on your daily life, making it difficult to perform simple tasks comfortably. However, there are effective strategies and treatments available to help you find relief and improve your knee health. It is crucial to consult with healthcare providers, follow their recommendations, and make necessary lifestyle modifications to alleviate the patella pain when kneeling and enhance overall knee function.
By taking proactive steps, such as engaging in rehabilitation exercises, using supportive knee pads or cushions, and maintaining a healthy weight, you can alleviate knee pain while kneeling and resume your favorite activities without experiencing discomfort in the kneecap. Remember to listen to your body, avoid activities that exacerbate the pain, and seek medical advice if the symptoms persist or worsen.
Don’t let patella pain when kneeling hold you back. With the right combination of treatments and lifestyle adjustments, you can regain comfort and enjoy a pain-free kneeling experience. Take charge of your knee health and prioritize your well-being, and soon you’ll be back on your knees with ease.
FAQ
What is patella pain when kneeling?
Patella pain when kneeling, also known as patellofemoral pain syndrome (PFPS), is discomfort or soreness in the kneecap area that occurs while kneeling.
What causes patella pain when kneeling?
Patella pain when kneeling can be caused by factors such as overuse, improper training techniques, changes in activity level, and alignment issues in the kneecap.
How is patella pain when kneeling diagnosed?
To diagnose patella pain when kneeling, healthcare providers may conduct a thorough examination, assess the range of motion, and perform imaging tests such as X-rays, CT scans, MRI, or ultrasound.
Can patella pain when kneeling be treated without surgery?
Yes, non-surgical treatment options for patella pain when kneeling include rest, avoiding activities that exacerbate the pain, taking pain relievers, engaging in rehabilitation exercises to strengthen the muscles supporting the knees, using supportive braces or orthotics, and adopting knee-friendly sports.
What surgical procedures are available for patella pain when kneeling?
Surgical interventions for patella pain when kneeling may include arthroscopy, where a camera and specialized tools are used to identify and repair issues, and realignment surgeries to correct the angle of the kneecap or alleviate pressure on the cartilage.
Are there any lifestyle modifications that can help with patella pain when kneeling?
Yes, individuals experiencing patella pain when kneeling can benefit from avoiding activities that exacerbate the pain, adopting proper techniques when kneeling or bending down, using supportive knee pads or cushions, maintaining a healthy weight, and engaging in regular physical activity to strengthen the muscles supporting the knees.
How can I prepare for a medical appointment about patella pain when kneeling?
Before the appointment, document your symptoms and their duration, provide relevant personal information such as previous knee injuries or surgeries, and bring copies of any previous X-rays or imaging tests. Having a trusted friend or family member accompany you and preparing a list of questions can also be helpful.
How can I alleviate patella pain when kneeling?
To alleviate patella pain when kneeling, it is essential to consult with healthcare providers, follow their recommendations, and make necessary lifestyle modifications. Non-surgical treatments and surgical interventions can also provide relief and improve knee health.