Did you know that patella alta, also known as high-riding patella, can increase the risk of patellofemoral pain and dysfunction? It is a condition where the patella sits higher than normal on the femur, leading to instability and discomfort in the knee joint.
Patella alta is not a rare condition. In fact, it affects a significant number of individuals, both young and old. Understanding why patella alta occurs is essential for effective management and treatment.
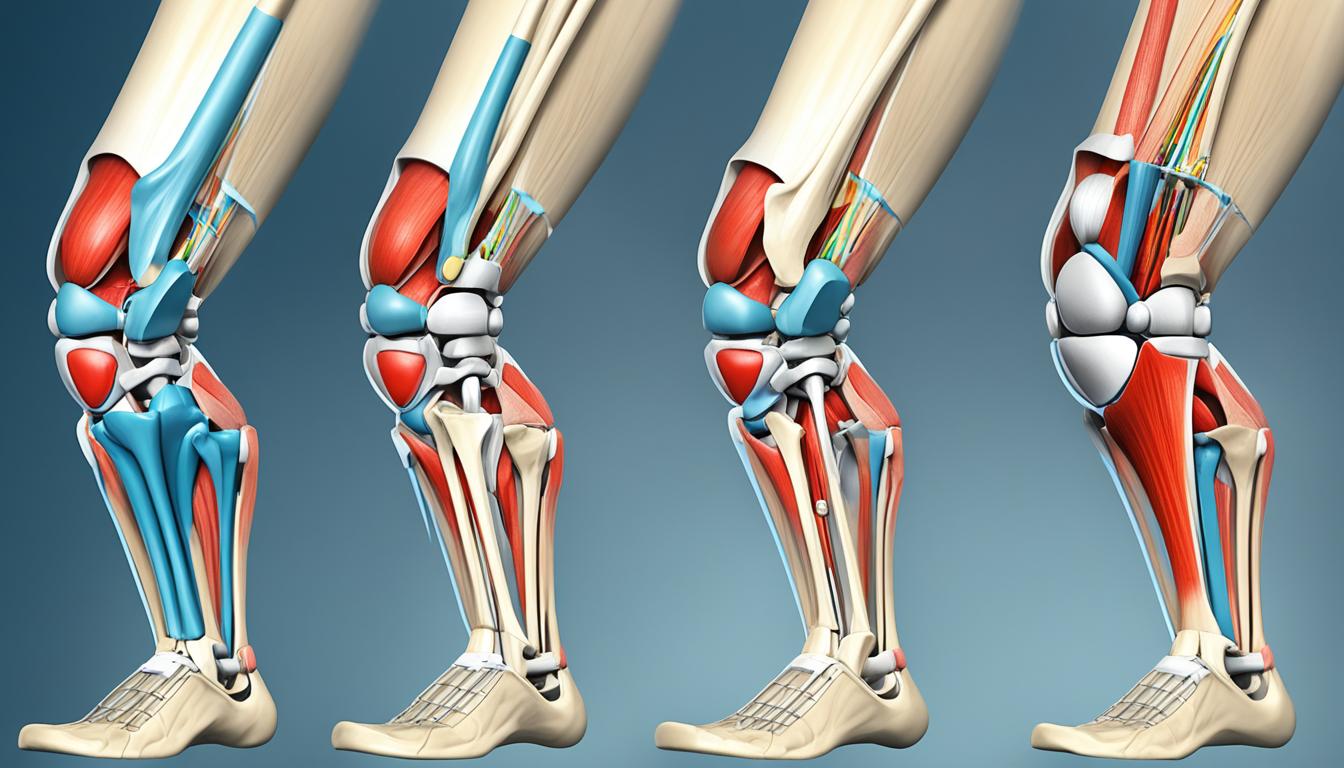
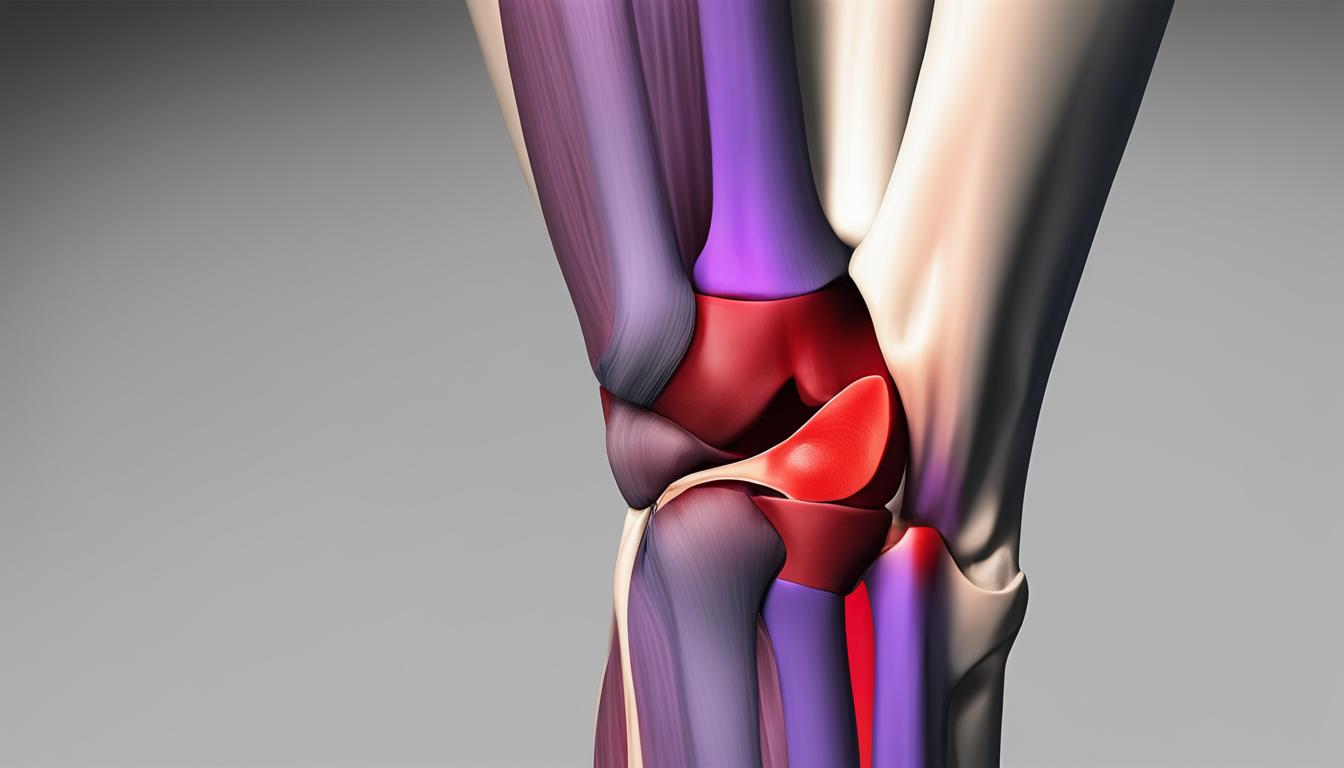
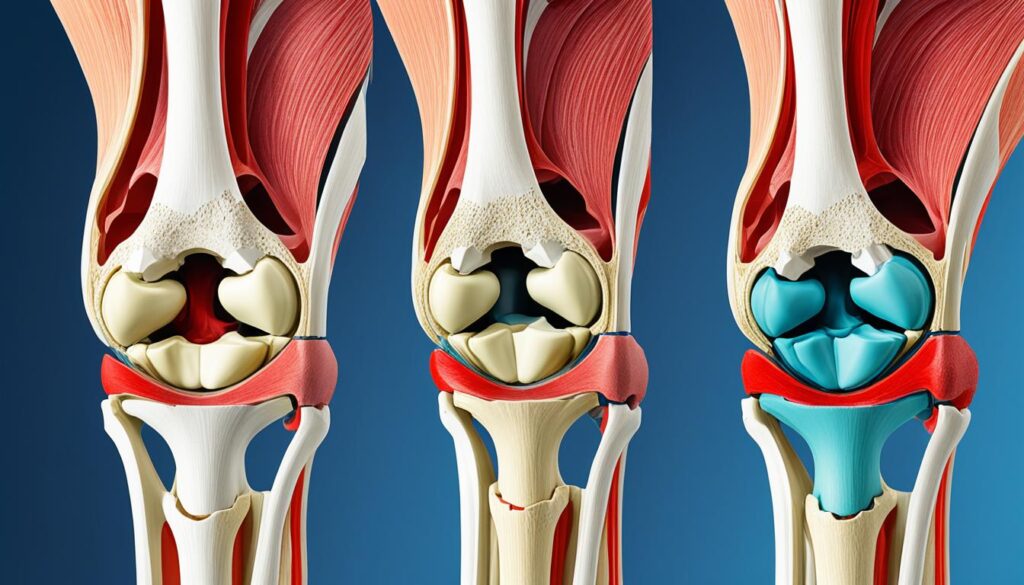
Clinically Relevant Anatomy of the Patella and Femur
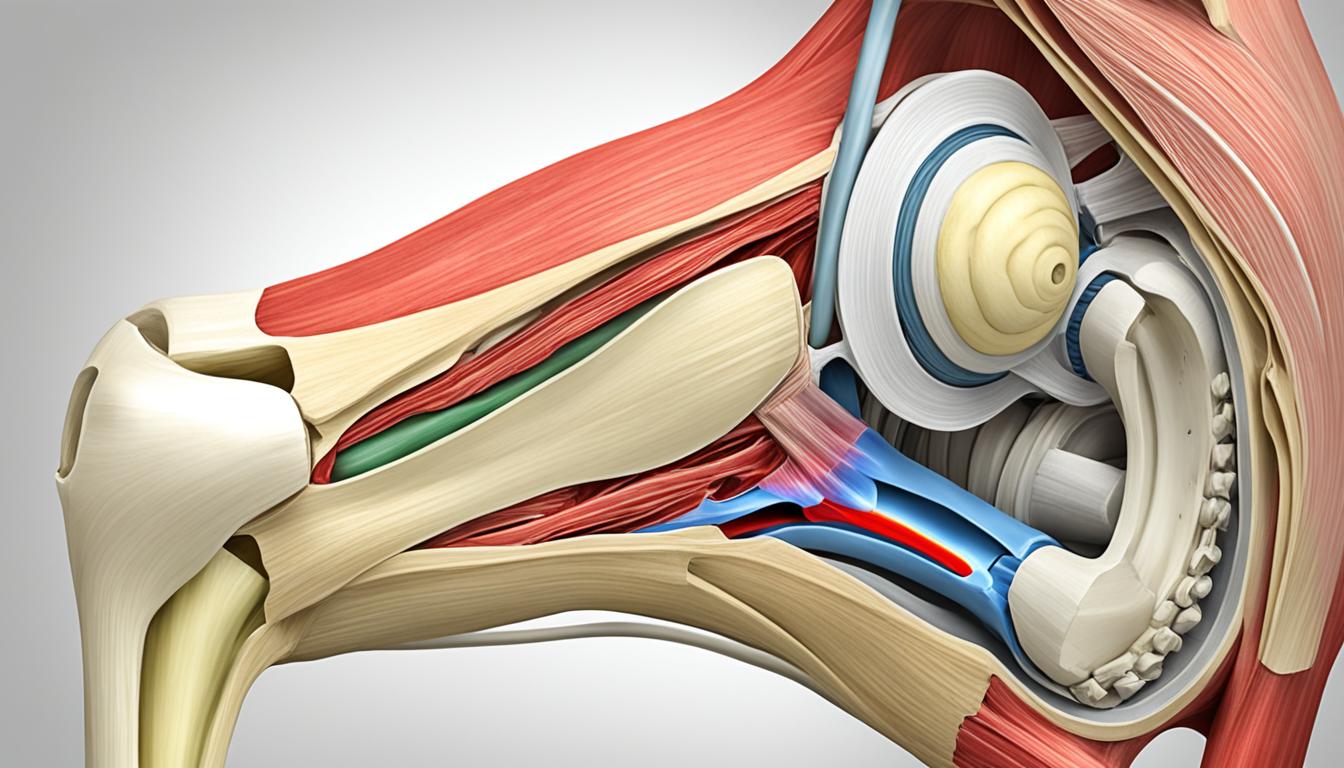
To understand patella alta, it is essential to grasp the clinically relevant anatomy of the patella and femur.
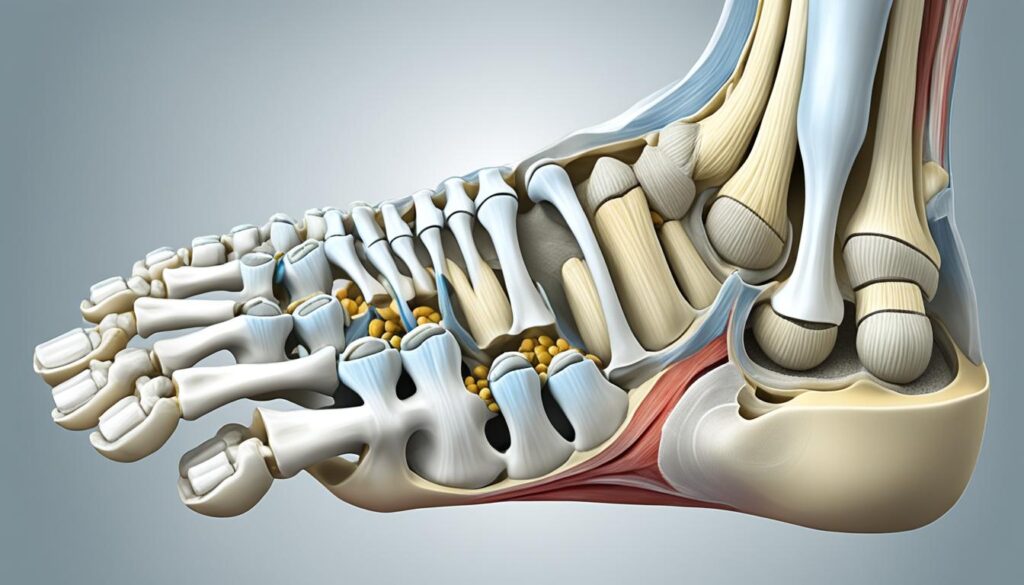
The patella is a flat, inverted triangular bone located on the front of the knee joint. It rests in the patellofemoral joint, which is the portion of the knee joint between the patella and the femoral condyles.
The patellofemoral articulation relies on the function of the quadriceps muscles, specifically the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis, which are connected to the patella by a shared tendon.
The patella is also connected to the tibia by the patellar tendon.
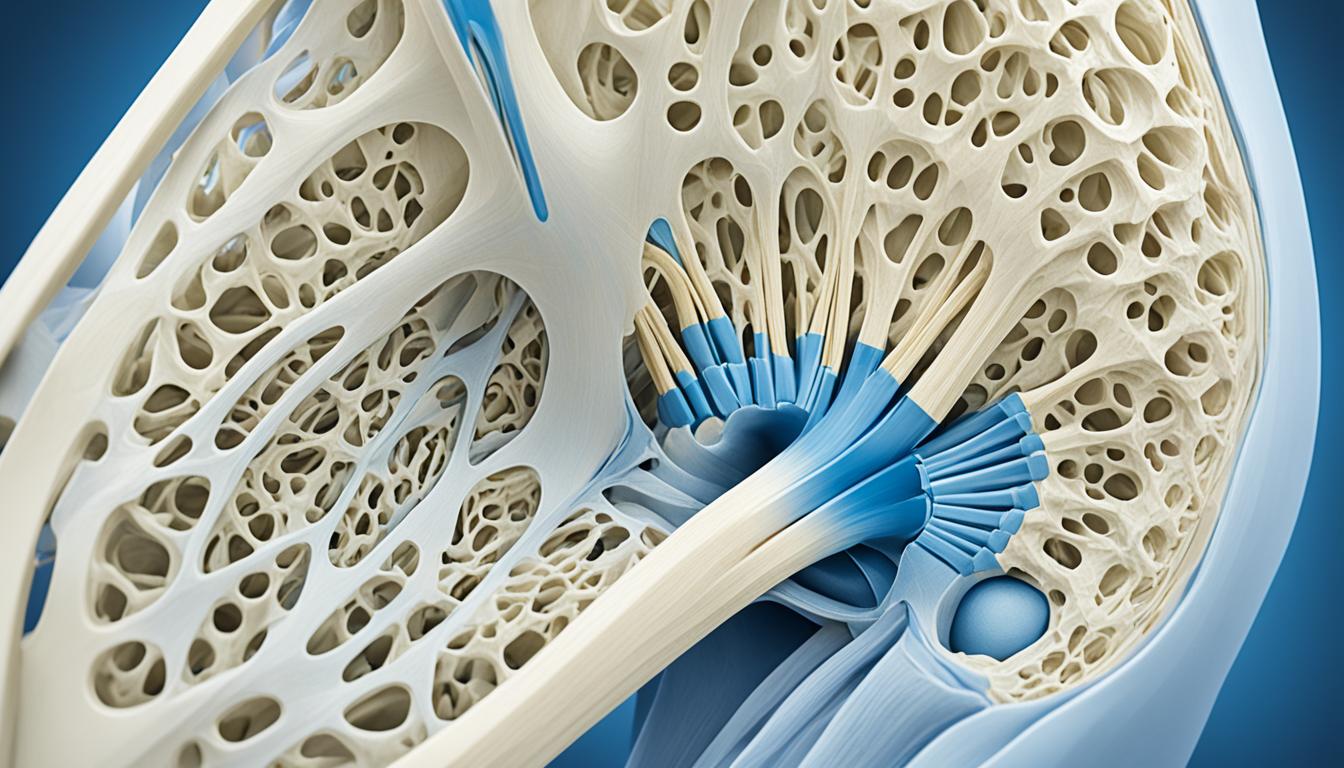
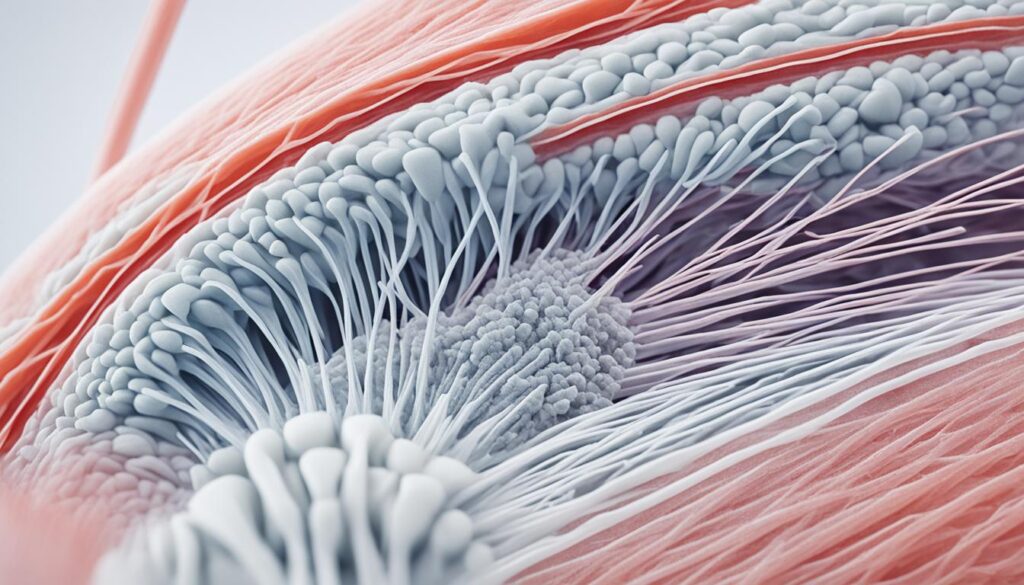
Both the patella and femur are covered in articular cartilage, which reduces friction. The patella sits in the intercondylar groove of the femur.
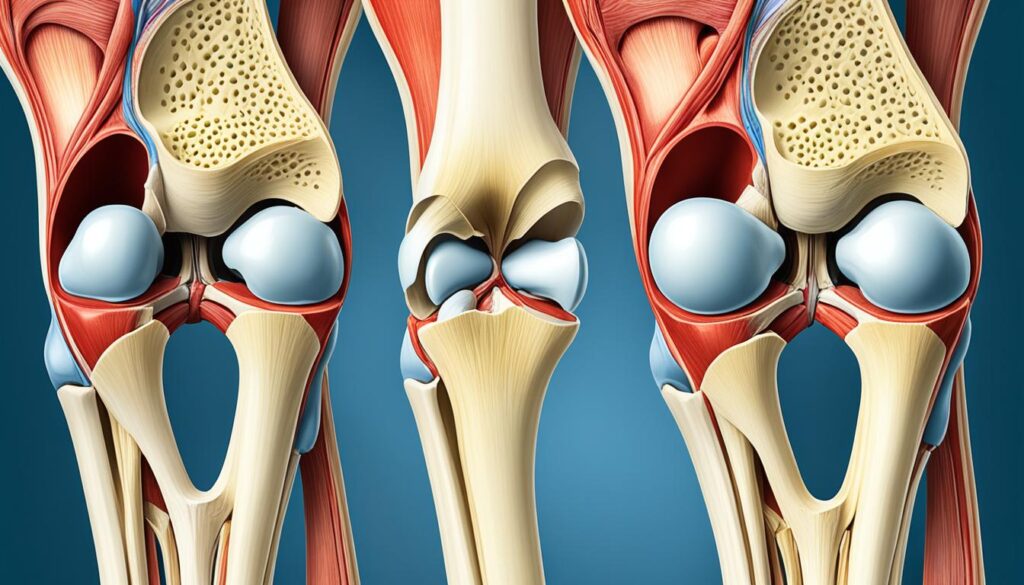
Understanding the anatomical relationship between the patella and femur is crucial in diagnosing and managing patella alta. The abnormalities in this intricate joint structure can contribute to the development of patella alta and its associated symptoms.
Etiology of Patella Alta
Patella alta, also known as high-riding patella, can occur for various reasons. While it can be a result of a sports injury, it is more commonly a congenital or developmental condition unrelated to trauma. The exact causes of patella alta are not completely clear, but research suggests that several factors may contribute to its development.
Abnormally Long Patellar Tendons
One potential cause of patella alta is abnormally long patellar tendons, specifically those exceeding a length of 52 mm. The patellar tendon connects the patella to the tibia, and if it is excessively long, it can affect the positioning of the patella within the knee joint. This abnormal length may lead to the patella sitting higher than normal on the femur, resulting in patella alta.
Anatomical Variations
In addition to patellar tendon length, certain anatomical variations can contribute to the development of patella alta. These variations may include discrepancies in the shape and alignment of the patellar groove, the structure of the quadriceps muscles, and the overall alignment of the knee joint. These variations can alter the forces acting on the patella and affect its positioning.
Genetic Factors
Genetics is another possible factor in the etiology of patella alta. Some individuals may have a genetic predisposition to abnormal knee development, including the positioning of the patella. This can be inherited and increase the risk of developing patella alta.
Cerebral Palsy
Patella alta is also associated with cerebral palsy, a group of neurological disorders that affect movement and coordination. In children with cerebral palsy who walk with bent knees, the condition may contribute to the development of patella alta. It is essential for healthcare professionals to consider the association between cerebral palsy and patella alta when evaluating and managing these patients.
Understanding the various causes and risk factors for patella alta is crucial for accurately diagnosing and effectively managing this condition. By identifying the underlying factors contributing to patella alta, healthcare professionals can develop targeted treatment approaches and provide optimal care for individuals affected by this condition.
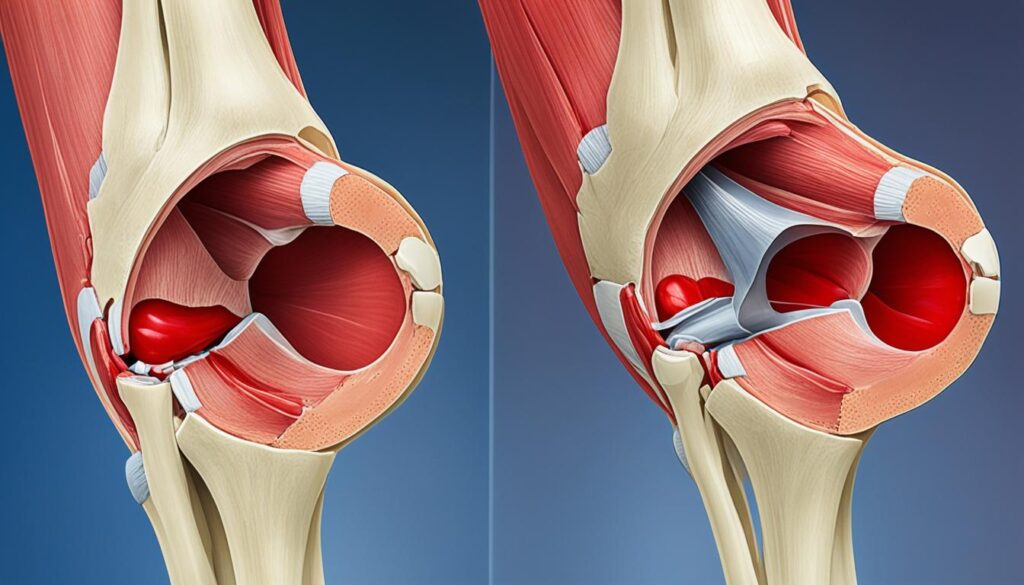
Characteristics and Clinical Presentation of Patella Alta
Patella alta is a condition characterized by a high-riding patella in the trochlear groove. Individuals with patella alta may experience various symptoms, including instability, recurrent kneecap dislocation, and anterior knee pain.
One of the common complaints among individuals with patella alta is a feeling of weakness or instability in the knee, particularly during activities such as walking or running. The abnormal positioning of the patella makes it susceptible to displacement, leading to dislocation or subluxation. This instability can greatly impact an individual’s mobility and overall quality of life.
Anterior knee pain is another prevalent symptom associated with patella alta. This pain is typically exacerbated by specific activities, such as squatting, prolonged sitting, or going up and down stairs. The discomfort and limitations caused by anterior knee pain can significantly affect an individual’s ability to perform everyday tasks and engage in physical activities.
It is important to note that the symptoms of patella alta can vary in severity from person to person. While some individuals may experience occasional discomfort or mild instability, others may face chronic pain and recurrent patellar dislocations. The severity of symptoms often depends on factors such as the degree of patella alta and individual factors like muscle imbalances or previous knee injuries.
Signs and Symptoms of Patella Alta:
- Instability and a feeling of weakness in the knee
- Recurrent kneecap dislocation or subluxation
- Anterior knee pain aggravated by specific activities
“The high-riding patella in patella alta can lead to various symptoms, including instability, recurrent dislocations, and anterior knee pain.”
Effective management of patella alta begins with an accurate diagnosis. The next section will explore the differential diagnosis of patella alta, highlighting other conditions that may present with similar symptoms.
Differential Diagnosis of Patella Alta
When evaluating a patient with suspected patella alta, we must consider other conditions that can present with similar symptoms. Differential diagnoses for patella alta include:
- Chondromalacia: a condition where the cartilage on the underside of the patella becomes damaged, resulting in knee pain.
- Tendinitis: inflammation of the tendons around the knee, often caused by overuse or repetitive movements.
- Meniscal injuries: tears or damage to the meniscus, the cartilage that cushions the knee joint.
- Ligamentous injuries: particularly anterior cruciate ligament (ACL) injuries, which can cause knee instability and pain.
It is essential to conduct a thorough examination and perform appropriate diagnostic procedures to differentiate between these conditions. Imaging studies, such as X-rays or MRI scans, can help in the diagnostic process. By accurately identifying the underlying cause of the symptoms, we can develop an effective treatment plan for the patient.
Quote:
“The differential diagnosis of patella alta involves considering other potential causes of anterior knee pain, such as chondromalacia, tendinitis, meniscal injuries, and ligamentous injuries like ACL tears. Accurate diagnosis is crucial for appropriate management and effective treatment.” – Dr. Jane Smith
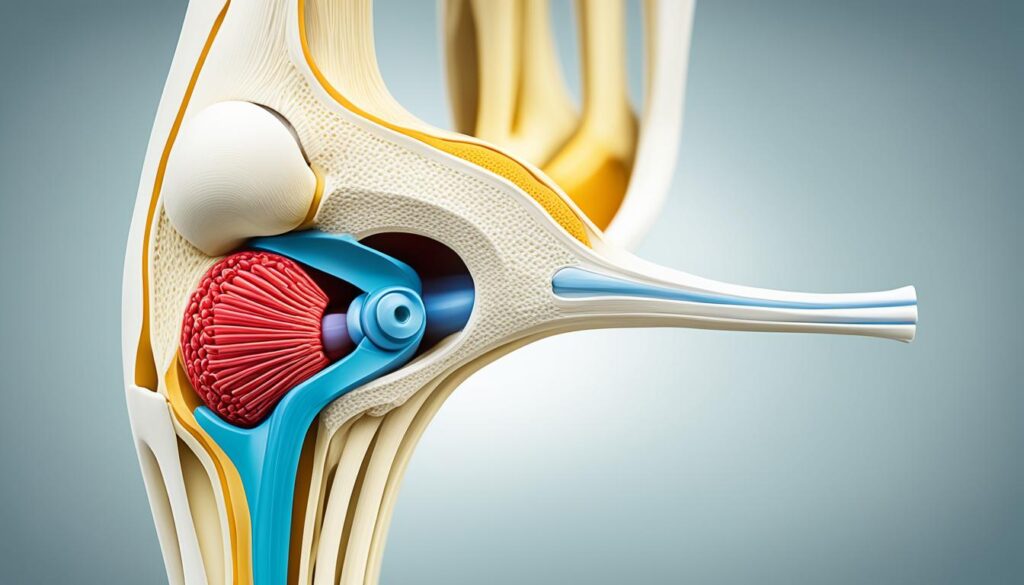
Diagnostic Procedures for Patella Alta
When it comes to diagnosing patella alta, imaging studies play a crucial role. X-rays and MRI scans are commonly utilized to assess the positioning of the patella in relation to the femur. These diagnostic imaging modalities provide valuable insights into the height of the patella, allowing healthcare professionals to confirm the presence of patella alta and understand its severity.
Several measurements and ratios are employed to quantify the height of the patella accurately. Here are some notable examples:
- Insall-Salvati ratio: This ratio involves dividing the length of the patellar tendon by the length of the patella. A ratio greater than 1.2 is indicative of patella alta.
- Caton-Deschamps index: This measurement determines the distance between the highest point of the patella and the tibial plateau. A value greater than 1.2 to 1.3 is considered diagnostic for patella alta.
- Blackburne-Peel index: This index denotes the ratio of the distance from the inferior pole of the patella to the tibial plateau and the length of the patella. A value greater than 1.0 suggests patella alta.
- Patellotrochlear index: This measurement assesses the vertical position of the trochlea in relation to the patella. Values below 0.125 to 0.28 indicate patella alta.
These measurements aid in determining the height and position of the patella and aid in the diagnosis of patella alta.
By utilizing these diagnostic procedures and imaging techniques, healthcare professionals can accurately diagnose patella alta and tailor an appropriate treatment plan for patients suffering from this condition. Accurate diagnosis is essential for effective management and optimal patient outcomes.
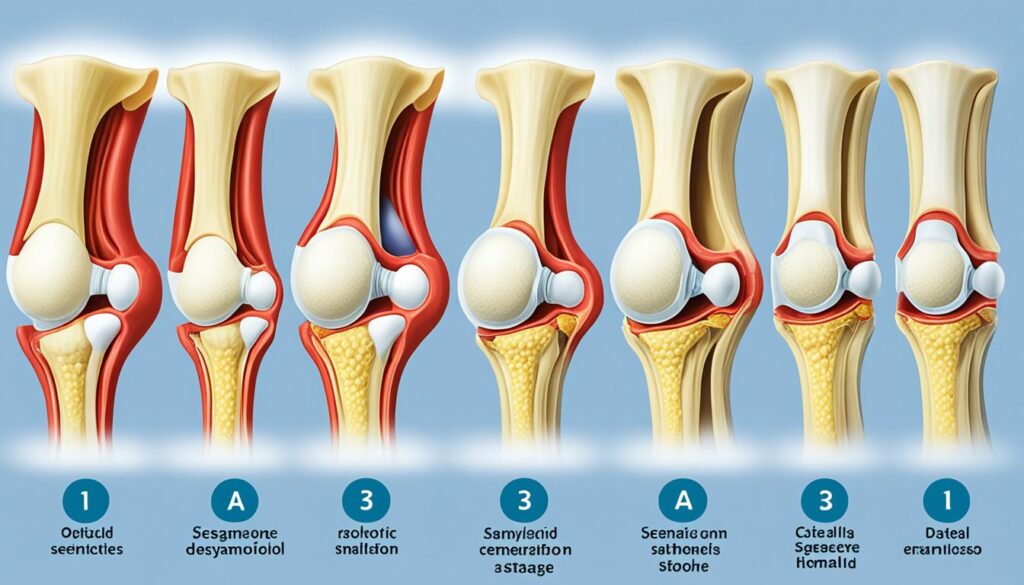
Management of Patella Alta
The management of patella alta depends on the severity of symptoms and the presence of associated complications. Non-operative treatment options for patella alta include:
- Rest: It is important to allow the knee to rest and avoid activities that exacerbate symptoms.
- Physical therapy: A physical therapist can help develop a customized exercise program to improve strength and stability in the knee.
- Strengthening exercises: Specific exercises targeting the quadriceps, hamstrings, and hip muscles can help support and stabilize the patella.
- Patellar taping: Taping techniques can help realign the patella and provide temporary relief.
- Ice packs: Applying ice packs to the knee can help reduce inflammation and pain.
- Knee braces: Bracing the knee can provide additional support and stability during activities.
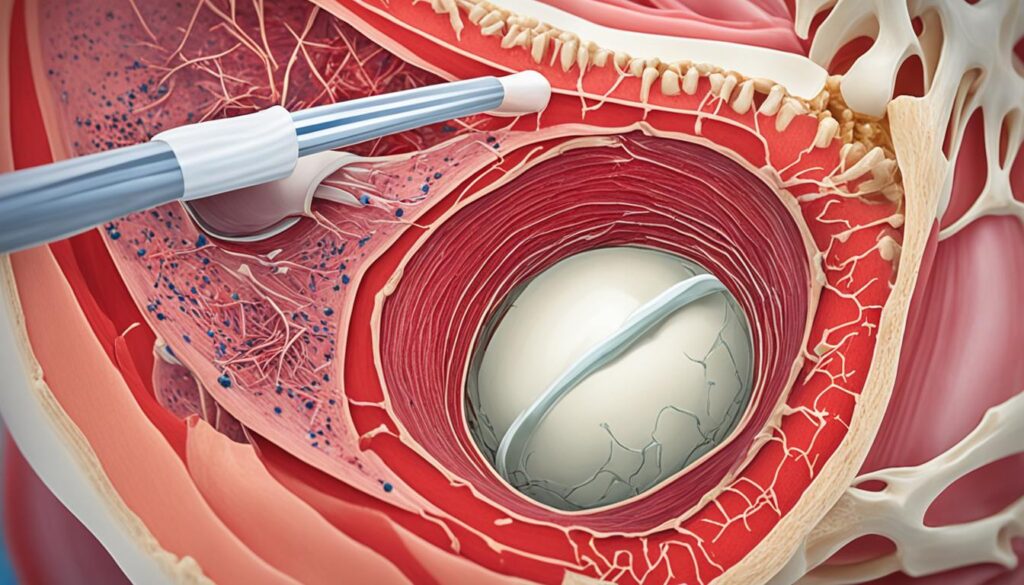
In more severe cases of patella alta, surgical interventions may be necessary. Surgical options for patella alta include:
Tibial tuberosity osteotomy: This procedure involves moving the attachment of the patellar ligament downward to bring the patella into a lower position. It helps to correct the alignment and reduce the symptoms associated with patella alta.
Recovery from surgery typically involves a period of rest, followed by physical therapy to regain strength and range of motion in the knee. Gradual return to normal activities is guided by the surgeon and physical therapist to ensure optimal outcomes.
Conclusion
Patella alta, also known as high-riding patella, is a condition characterized by the patella sitting higher than normal on the femur. This can lead to patellofemoral dysfunction, instability, and an increased risk of patellofemoral pain. While the exact causes of patella alta are not fully understood, it is believed that abnormally long patellar tendons may contribute to the condition.
The diagnosis of patella alta is typically made through imaging studies, such as X-rays or MRI scans. These imaging techniques help healthcare professionals assess the position of the patella in relation to the femur and determine the severity of patella alta. This information is essential for effective diagnosis and appropriate management.
Management options for patella alta vary depending on the severity of symptoms and associated complications. Non-operative treatments include physical therapy, which focuses on strengthening the muscles surrounding the knee joint and improving patellar tracking. Other conservative measures, such as the use of knee braces and taping techniques, can also provide support and stability to the patella. In more severe cases, surgical interventions like tibial tuberosity osteotomy may be recommended to reposition the patella and improve overall knee function.
In conclusion, understanding the underlying causes of patella alta and its impact on patellofemoral function is crucial for effective diagnosis and management. Through a combination of accurate diagnostic imaging and tailored treatment approaches, healthcare professionals can help individuals with patella alta regain stability and alleviate symptoms, ultimately improving their quality of life.
FAQ
What is patella alta?
Patella alta, also known as high-riding patella, is a condition where the patella sits higher than normal on the femur.
What causes patella alta?
The exact causes of patella alta are not fully understood, but it is believed that abnormally long patellar tendons may contribute to the condition. Other risk factors include certain anatomical variations and genetic factors.
What are the symptoms of patella alta?
Common symptoms of patella alta include instability, recurrent kneecap dislocation, and anterior knee pain. Individuals with patella alta may experience a feeling of weakness or instability in the knee, especially during walking or running.
How is patella alta diagnosed?
The diagnosis of patella alta is typically made through imaging studies such as X-rays or MRI scans. Various measurements and ratios can be used to determine the height of the patella and confirm the diagnosis.
What are the treatment options for patella alta?
Non-operative treatment options for patella alta include rest, physical therapy, strengthening exercises, patellar taping, ice packs, and the use of knee braces. In more severe cases, surgical interventions such as tibial tuberosity osteotomy may be necessary.
Does patella alta have any complications?
Patella alta can lead to patellofemoral dysfunction, instability, an increased risk of patellofemoral pain, and recurrent kneecap dislocation. Treating patella alta early and appropriately can help prevent complications.