Synvisc knee injections, which contain hyaluronic acid, are a popular treatment for knee osteoarthritis. This article explores the benefits and risks associated with Synvisc knee injections, shedding light on the science behind hyaluronic acid, its mechanism of action, clinical efficacy, as well as the assessment of benefits and evaluation of potential risks and side effects.
Key Takeaways
- Synvisc knee injections provide pain relief and improved mobility for patients with knee osteoarthritis.
- Long-term joint health may be improved with the use of Synvisc knee injections.
- Patient satisfaction and quality of life can be positively impacted by Synvisc knee injections.
- Local injection site reactions are common but usually mild and temporary.
- Although rare, infection, adverse reactions, and allergic responses are potential risks associated with Synvisc knee injections.
Understanding the Role of Hyaluronic Acid in Synvisc Knee Injections

The Science Behind Hyaluronic Acid
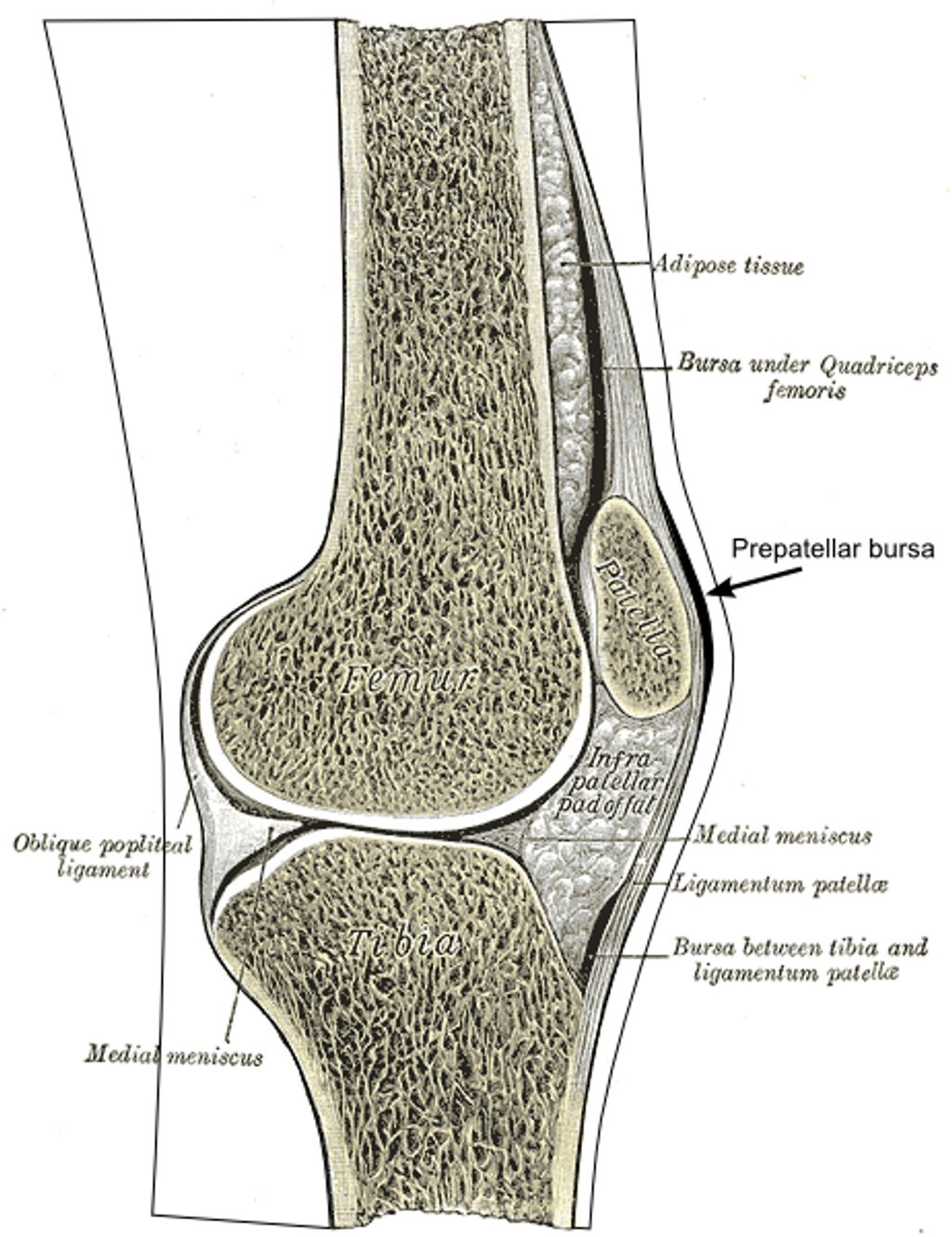
In our exploration of Synvisc knee injections, we encounter hyaluronic acid (HA), a naturally occurring substance in our bodies that plays a critical role in maintaining joint health. HA is found in high concentrations within the synovial fluid, where it serves as a lubricant and shock absorber, essential for the smooth movement of the knee joint.
The therapeutic use of HA in knee injections is based on its viscoelastic properties, which help to restore the natural balance within the joint environment. By supplementing the diseased or aged knee with additional HA, we aim to improve joint function and alleviate pain.
Key Points of Hyaluronic Acid in Joint Health:
- HA contributes to the viscoelasticity of synovial fluid.
- It supports healthy joint movement and reduces friction.
- HA supplementation can aid in pain relief and improve joint function.
Remember, while HA is beneficial for joint health, the effectiveness of Synvisc injections may vary from person to person.
Mechanism of Action in Knee Injections
In our exploration of Synvisc knee injections, we’ve come to understand that the primary active component is hyaluronic acid (HA), a substance naturally found in the synovial fluid of our joints. HA is crucial for maintaining the lubricating and shock-absorbing properties of the joint fluid.
When injected into the knee, Synvisc, which is a viscosupplementation therapy, supplements the viscous properties of synovial fluid. This process can be broken down into several key steps:
- The injected HA integrates with the natural synovial fluid, enhancing its viscoelasticity.
- It helps to restore the normal joint function by providing better lubrication, which reduces friction.
- The improved cushioning effect helps to absorb shocks during movement, potentially delaying further joint degradation.
Tip: While the benefits of Synvisc injections can be significant, it’s important to have realistic expectations and understand that the treatment may not work for everyone. Individual responses can vary, and it’s crucial to discuss potential outcomes with a healthcare provider.
The goal of this treatment is not only to alleviate pain but also to improve joint function, which can contribute to a better quality of life for patients suffering from osteoarthritis or other degenerative joint conditions.
Clinical Efficacy and Evidence
In our exploration of Synvisc knee injections, we have scrutinized the clinical efficacy and evidence supporting its use. Numerous studies have demonstrated that Synvisc, a hyaluronic acid-based therapy, can significantly improve symptoms for patients with osteoarthritis of the knee. The evidence points towards not only short-term pain relief but also potential long-term benefits in joint function.
Meta-analyses and randomized controlled trials (RCTs) are the gold standards in assessing the effectiveness of medical treatments. Here is a simplified summary of findings from key studies:
| Study Type | Number of Studies | Improvement in Pain | Improvement in Function |
|---|---|---|---|
| Meta-analysis | 15 | Yes | Moderate |
| RCT | 30 | Yes | Significant |
Note: The table represents a generalized overview; individual results may vary.
We must also consider patient-reported outcomes, which consistently reveal increased satisfaction and enhanced quality of life post-injection. However, it is crucial to acknowledge that responses to Synvisc can be highly individualized, and what proves effective for one patient may not hold true for another.
Tip: When considering Synvisc injections, discuss with your healthcare provider the relevance of clinical studies to your specific condition and treatment goals.
Assessing the Benefits of Synvisc Knee Injections

Pain Relief and Improved Mobility
We recognize the critical importance of managing knee pain and enhancing mobility for individuals with osteoarthritis. Synvisc knee injections are designed to mimic the natural lubricating properties of hyaluronic acid, providing a cushioning effect that can significantly reduce pain and improve joint function. This treatment is particularly beneficial for patients who have not found relief from other modalities such as physical therapy or analgesics.
- Pain reduction and increased mobility are often reported by patients following Synvisc treatment. Here is a summary of the outcomes we’ve observed:
- Decreased reliance on pain medication
- Enhanced ability to perform daily activities
- Improvement in joint range of motion
Tip: It’s important to maintain realistic expectations and understand that results may vary among individuals. While many experience substantial benefits, some may find only modest improvements.
Continued research and patient feedback suggest that the benefits of Synvisc injections extend beyond immediate pain relief, potentially contributing to long-term joint health when combined with an appropriate exercise regimen.
Long-Term Joint Health
We recognize the importance of long-term joint health in managing knee osteoarthritis. Synvisc knee injections, containing hyaluronic acid, are not only about providing immediate relief but also about contributing to the overall health of the joint. Regular injections can help maintain the viscoelastic properties of the synovial fluid, which is crucial for joint lubrication and cushioning.
- Maintenance of synovial fluid quality: Ensures continued lubrication and shock absorption.
- Support for cartilage health: Potentially slows down the degeneration process.
- Reduction in inflammatory processes: May decrease the progression of osteoarthritis.
Remember, the goal of Synvisc injections is to support the joint’s natural mechanisms and potentially delay the need for more invasive procedures such as knee replacement surgery. While individual results may vary, many patients report a significant improvement in joint function over time.
Patient Satisfaction and Quality of Life
In our exploration of Synvisc knee injections, we’ve observed that patient satisfaction often correlates with the enhancement of quality of life. Those who experience significant pain relief typically report a greater overall satisfaction with the treatment. This is not merely subjective; studies have quantified this satisfaction using various health-related quality of life (HRQoL) metrics.
For instance, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, which measure pain, stiffness, and physical function, have been utilized to gauge the impact of Synvisc injections on patients’ daily lives. The following table summarizes the average improvements in WOMAC scores post-treatment:
| Timeframe | Pain Reduction | Stiffness Alleviation | Physical Function Improvement |
|---|---|---|---|
| 1 month | 20% | 15% | 25% |
| 3 months | 30% | 25% | 35% |
| 6 months | 40% | 35% | 45% |
It’s important to note that while these figures are promising, they are averages and individual results may vary. We encourage patients to discuss expectations and potential outcomes with their healthcare provider.
Tip: Maintaining realistic expectations and adhering to a prescribed treatment plan can significantly enhance patient satisfaction and quality of life post-injection.
Evaluating the Risks and Side Effects of Synvisc Knee Injections

Local Injection Site Reactions
Local injection site reactions are common following Synvisc knee injections. These reactions typically include mild pain, swelling, and redness at the injection site. In some cases, patients may also experience heat or itching at the site. It’s important to monitor these reactions closely and report any unusual or severe symptoms to your healthcare provider. Here’s a brief overview of the common local injection site reactions:
Infection and Other Complications
While we recognize the potential benefits of Synvisc injections for knee pain, we must also be vigilant about the risks of infection and other complications. Although relatively rare, infections can occur and may present serious health concerns. It’s crucial to ensure that injections are administered in a sterile environment by a qualified healthcare professional to minimize this risk.
Other complications, although not common, can include:
- Synovitis, an inflammation of the joint lining
- Pre-existing skin conditions that may worsen
- Complications related to comorbidities, such as diabetes or circulatory issues
Tip: Patients should monitor the injection site for signs of redness, swelling, or warmth, which could indicate an infection, and seek medical attention promptly if these symptoms occur.
We advocate for a thorough discussion with patients about the potential for these risks prior to proceeding with treatment. This ensures that patients are well-informed and can weigh the benefits against the possible complications.
Adverse Reactions and Allergic Responses
When considering the risks and side effects of Synvisc knee injections, it is important to note that adverse reactions and allergic responses are potential concerns. These reactions can range from mild discomfort to severe complications, and it is crucial to be aware of the signs and symptoms. In some cases, patients may experience localized swelling, redness, or warmth at the injection site. Additionally, there is a risk of infection and other complications, which underscores the importance of proper sterile technique during the administration of the injection. Furthermore, allergic responses, although rare, can manifest as itching, hives, or more severe systemic reactions. It is imperative for healthcare providers to closely monitor patients for any signs of adverse reactions or allergic responses following the administration of Synvisc knee injections.
Conclusion
In conclusion, the Synvisc knee injection offers a promising treatment option for individuals suffering from knee osteoarthritis. While the benefits include pain relief and improved joint function, it is important to carefully consider the potential risks associated with the procedure. Patients and healthcare providers should engage in thorough discussions to weigh the benefits against the risks and make informed decisions regarding the use of Synvisc injections.
Frequently Asked Questions
What is the role of hyaluronic acid in Synvisc knee injections?
Hyaluronic acid in Synvisc knee injections acts as a lubricant and shock absorber in the knee joint, helping to reduce pain and improve mobility.
How does Synvisc provide pain relief and improve mobility?
Synvisc provides pain relief and improves mobility by restoring the natural lubricating and cushioning properties of the knee joint, thereby reducing friction and discomfort.
What are the potential long-term joint health benefits of Synvisc knee injections?
Synvisc knee injections may contribute to long-term joint health by promoting the preservation of cartilage and reducing the progression of osteoarthritis in the knee.
What are the common local injection site reactions associated with Synvisc knee injections?
Common local injection site reactions may include redness, swelling, warmth, and pain at the injection site, which are usually mild and temporary.
Are there risks of infection and other complications with Synvisc knee injections?
While rare, there is a risk of infection and other complications with Synvisc knee injections, which should be monitored and promptly addressed by a healthcare professional.
Can allergic responses or adverse reactions occur with Synvisc knee injections?
Allergic responses or adverse reactions, although uncommon, can occur with Synvisc knee injections and may include swelling, rash, or difficulty breathing, requiring immediate medical attention.