Hot knees can be a source of discomfort and inconvenience, impacting daily activities and overall quality of life. Understanding the causes and solutions for hot knees is essential for effective management. In this article, we will explore the anatomy of the knee joint, identify the causes of hot knees, discuss diagnostic techniques, and explore treatment options to alleviate this common issue.
Key Takeaways
- Hot knees can be caused by inflammatory conditions, overuse and strain, or environmental factors.
- Diagnostic techniques for hot knees include physical examination, imaging studies, and laboratory tests.
- Treatment options for hot knees may involve medication and pain management, physical therapy and rehabilitation, or surgical interventions.
- Understanding the structure and function of the knee joint is crucial in addressing hot knee problems.
- Hot knees can significantly impact daily activities, highlighting the importance of effective management strategies.
Understanding the Anatomy of the Knee Joint

Structure and Function of the Knee Joint
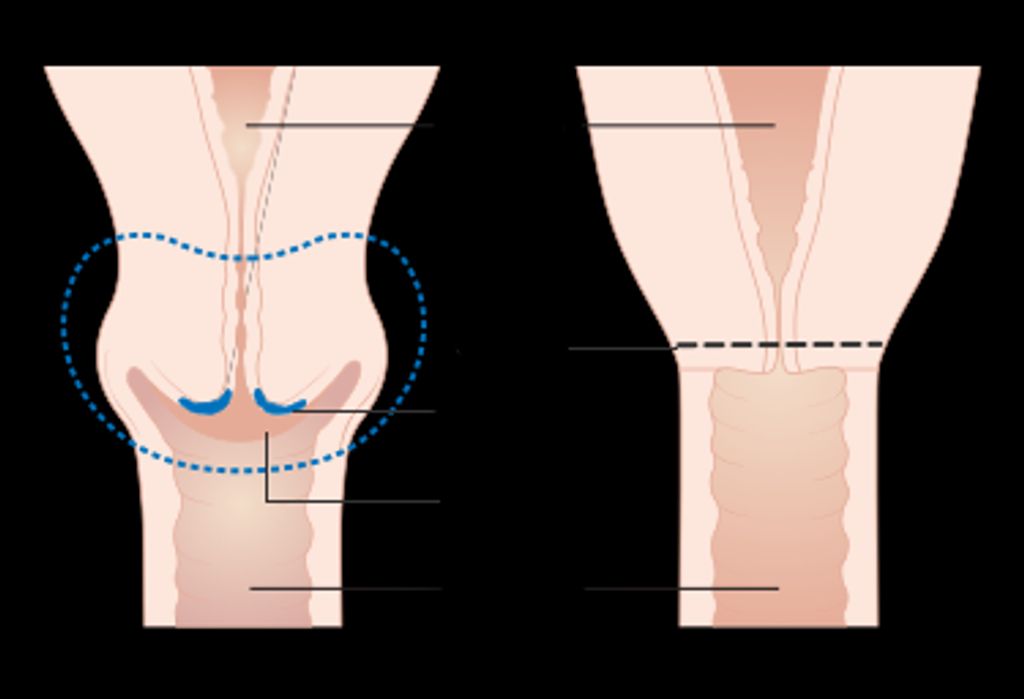
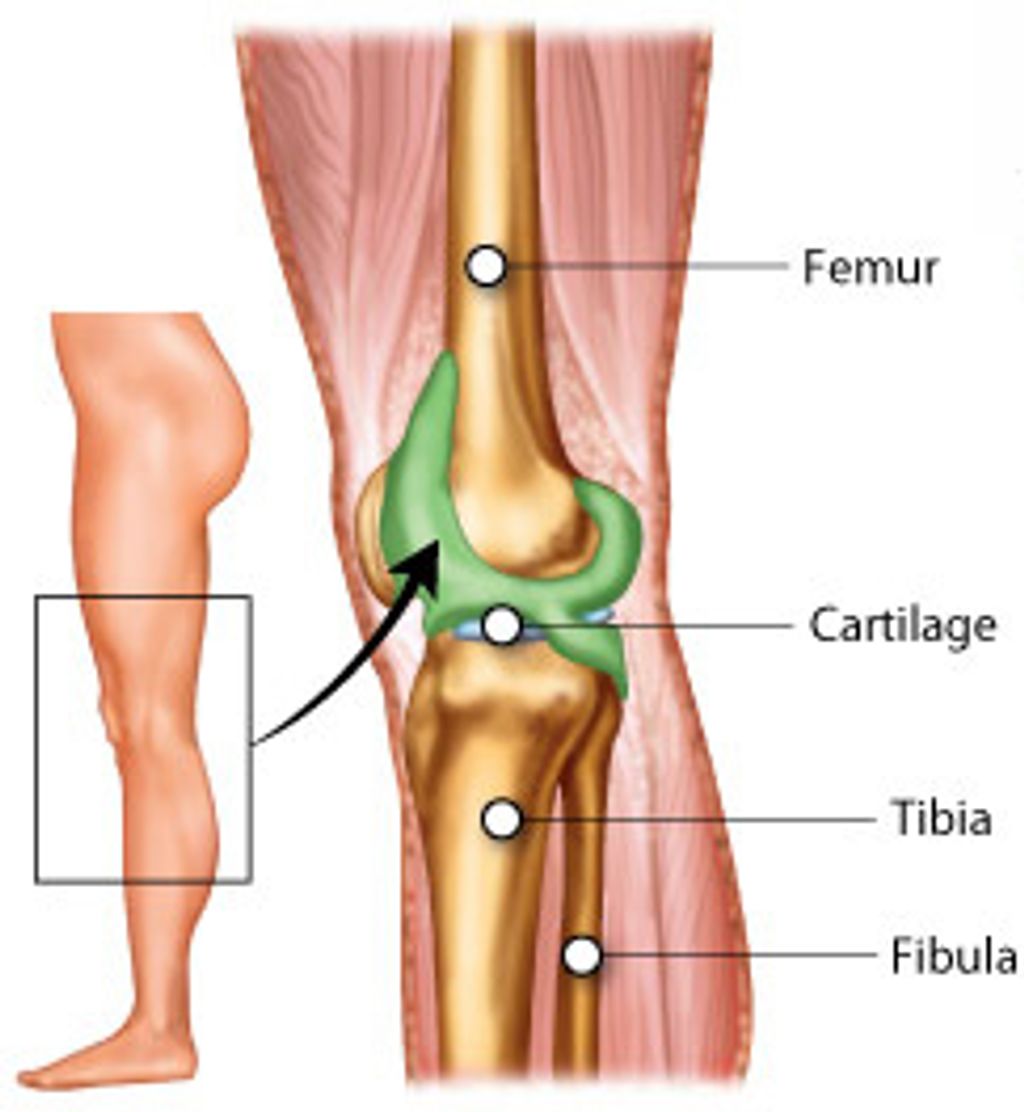
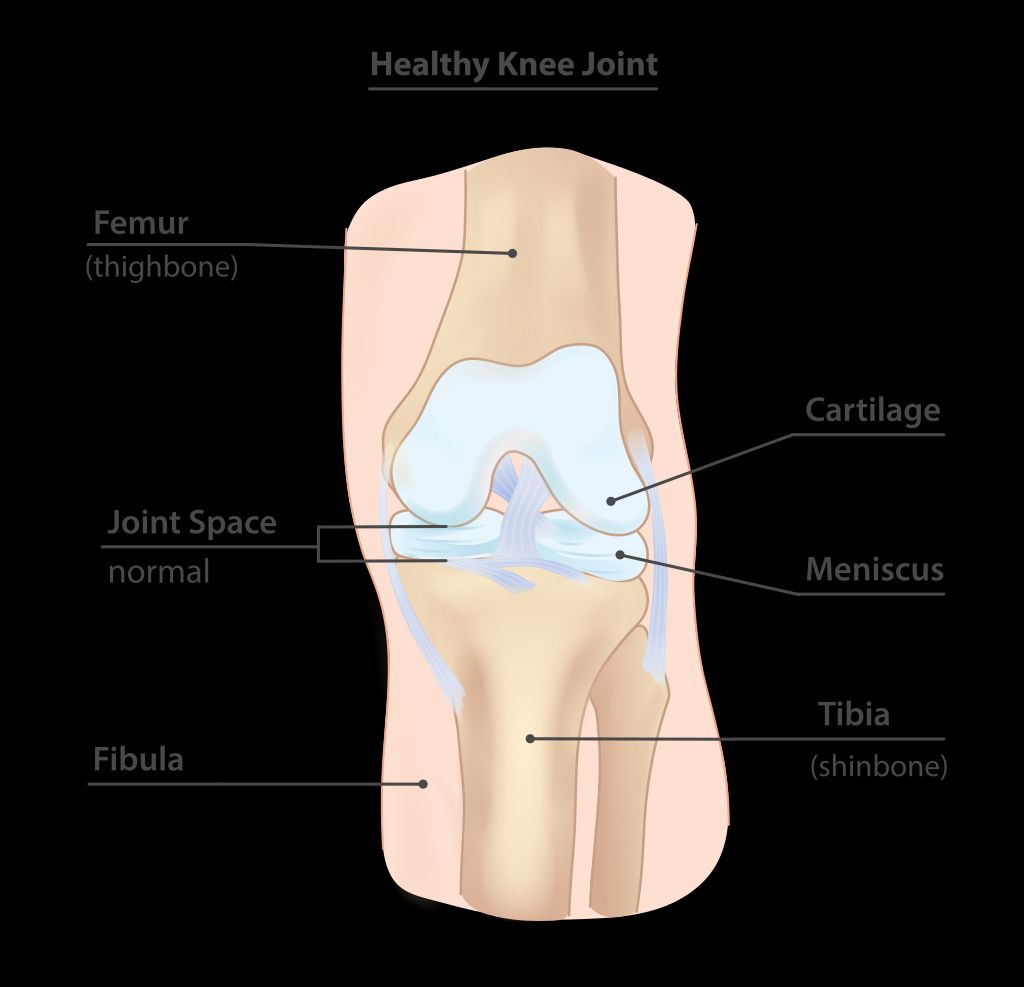
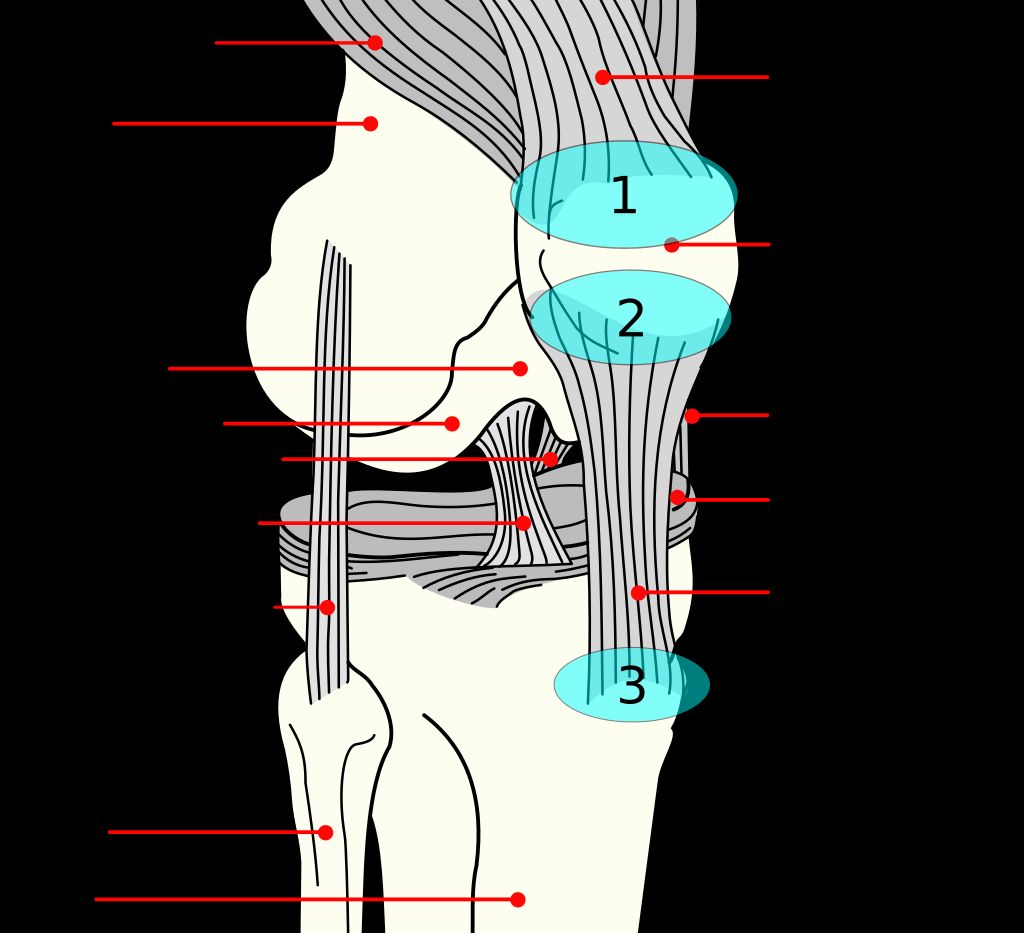
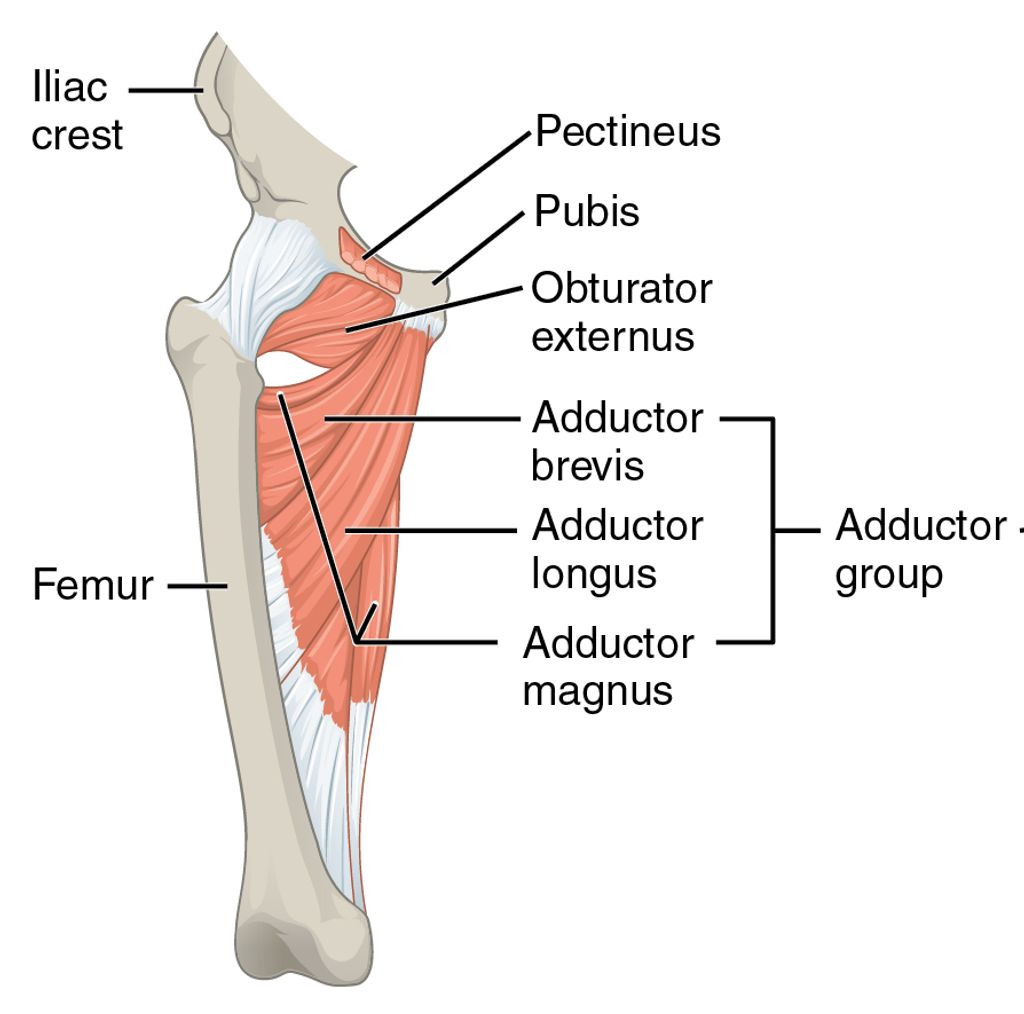
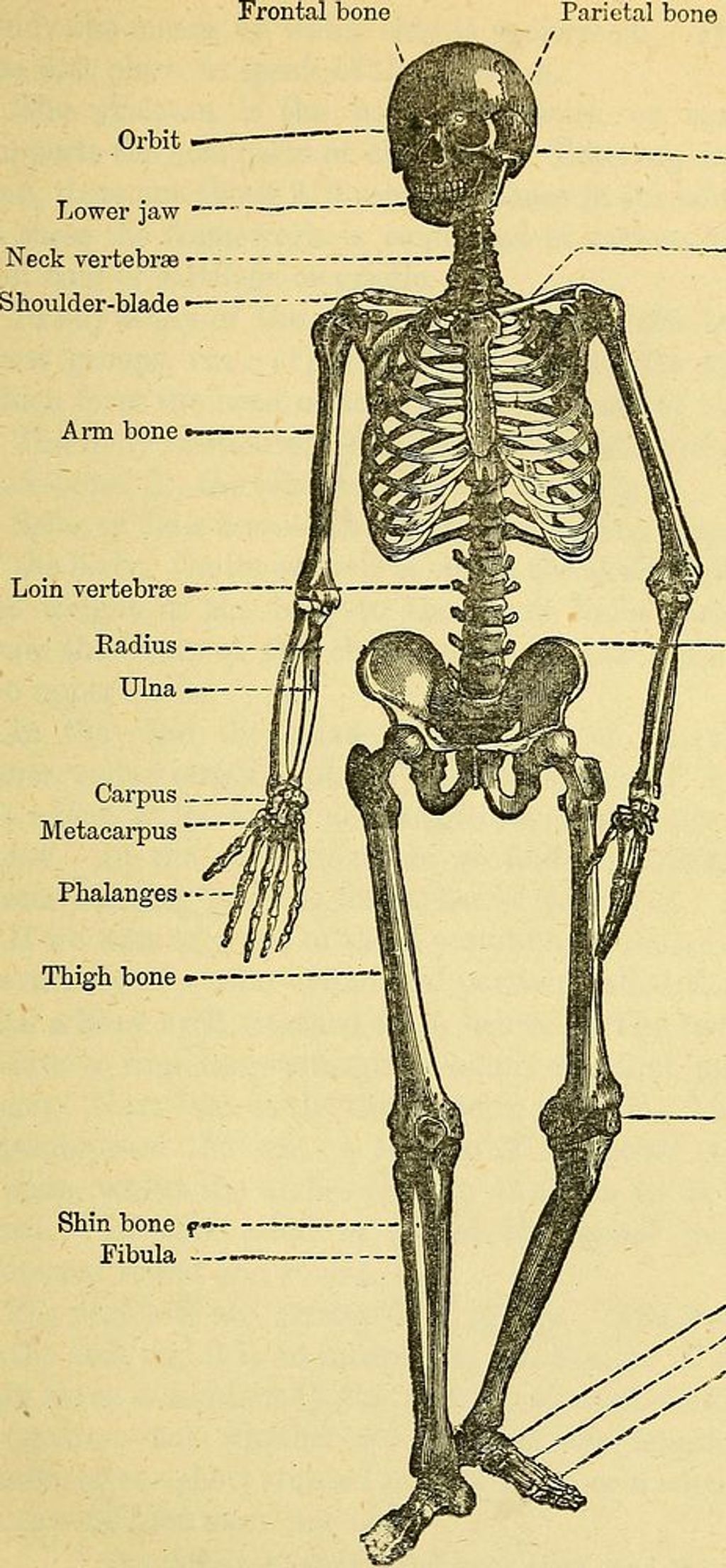
The knee joint is a complex structure that plays a crucial role in supporting our body weight and facilitating movement. It consists of several components, including the femur, tibia, and patella, which work together to provide stability and flexibility. Additionally, the knee joint is surrounded by a network of ligaments and tendons that help maintain its integrity.
One of the key functions of the knee joint is to absorb shock and distribute the forces generated during activities such as walking, running, and jumping. This is achieved through the presence of specialized cartilage, such as the meniscus, which acts as a cushion and reduces friction between the bones. The intricate interplay of these structures allows for smooth and coordinated motion, essential for our daily activities.
| Component | Function |
|---|---|
| Femur | Weight-bearing bone |
| Tibia | Supports body weight |
| Patella | Protects knee joint |
| Ligaments | Provide stability |
| Tendons | Facilitate movement |
Common Knee Problems
Structure and Function of the Knee Joint
Common Knee Problems
Hot knees can be caused by a variety of factors, including inflammation, overuse, and environmental factors. These issues can significantly impact our daily activities, making it important to address them promptly and effectively.
- Inflammatory Conditions
- Overuse and Strain
- Environmental Factors
Impact of Hot Knees on Daily Activities
We often underestimate the pivotal role our knees play in our daily lives until we experience discomfort like hot knees. This sensation can be a sign of underlying issues that, if left unaddressed, may lead to more serious complications. The impact of hot knees on daily activities can be significant, affecting everything from simple movements to our ability to engage in physical exercise.
-
Mobility and Stability: Our knees are crucial for both mobility and stability. When they’re inflamed or painful, even basic tasks such as walking, climbing stairs, or standing for extended periods become challenging.
-
Sleep Disturbances: Hot knees can also disrupt sleep patterns, as the discomfort may prevent finding a comfortable position, leading to restlessness and fatigue.
Tip: To minimize the impact on daily activities, it’s essential to address hot knee symptoms promptly with appropriate interventions.
- Work and Recreation: Professional responsibilities and recreational activities that require knee exertion can be particularly affected, potentially leading to decreased productivity and a diminished quality of life.
Identifying the Causes of Hot Knees

Inflammatory Conditions
Inflammatory conditions play a significant role in the development of hot knees. Chronic inflammation within the knee joint can lead to discomfort and heat sensation. It is important to consider conditions such as arthritis and synovitis, which are known to contribute to the heat experienced in the knees. Additionally, autoimmune disorders like rheumatoid arthritis can exacerbate the inflammatory response, further intensifying the sensation of heat within the knee joint. Understanding the underlying inflammatory processes is crucial in addressing the root cause of hot knees.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
Overuse and Strain
Overuse and strain are common contributors to the development of hot knees. Prolonged and repetitive stress on the knee joint can lead to inflammation and discomfort. It’s important to recognize the signs of overuse and strain to prevent further complications. Here’s a brief overview of the common causes:
| Causes of Hot Knees |
|---|
| Overexertion |
| Misalignment |
| Excessive Weight |
| Poor Footwear |
Seeking professional guidance and making necessary lifestyle adjustments can help alleviate the symptoms and promote knee health.
Environmental Factors
Environmental factors play a significant role in the development of hot knees. Excessive heat exposure and humidity are known to exacerbate knee discomfort, especially in individuals with pre-existing knee conditions. Additionally, prolonged exposure to pollutants and irritants in the environment can contribute to inflammation and discomfort in the knee joint. It’s important to be mindful of our surroundings and take necessary precautions to minimize the impact of environmental factors on knee health.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
Diagnostic Techniques for Hot Knees
Physical Examination
When we approach the issue of hot knees, our initial step is to conduct a thorough physical examination. This process allows us to observe the knee’s range of motion, detect any swelling or redness, and identify areas of tenderness. We systematically assess the knee by palpating specific anatomical landmarks and by asking patients to perform certain movements that may reveal underlying problems.
Palpation and observation during the physical examination can provide us with valuable clues about the knee’s condition. For instance, warmth and redness over the joint may indicate an inflammatory process, while crepitus— a crackling sensation felt under the skin—could suggest cartilage wear.
Remember, the physical examination is a non-invasive way to gather important information and should always be performed with care to avoid exacerbating any knee discomfort.
The following list outlines the key components we examine:
- Inspection of the knee for signs of swelling and discoloration
- Assessment of the knee’s range of motion
- Palpation to pinpoint areas of warmth or tenderness
- Evaluation of the ligaments and tendons for stability and integrity
- Observation of gait and posture to identify biomechanical issues that may affect the knee
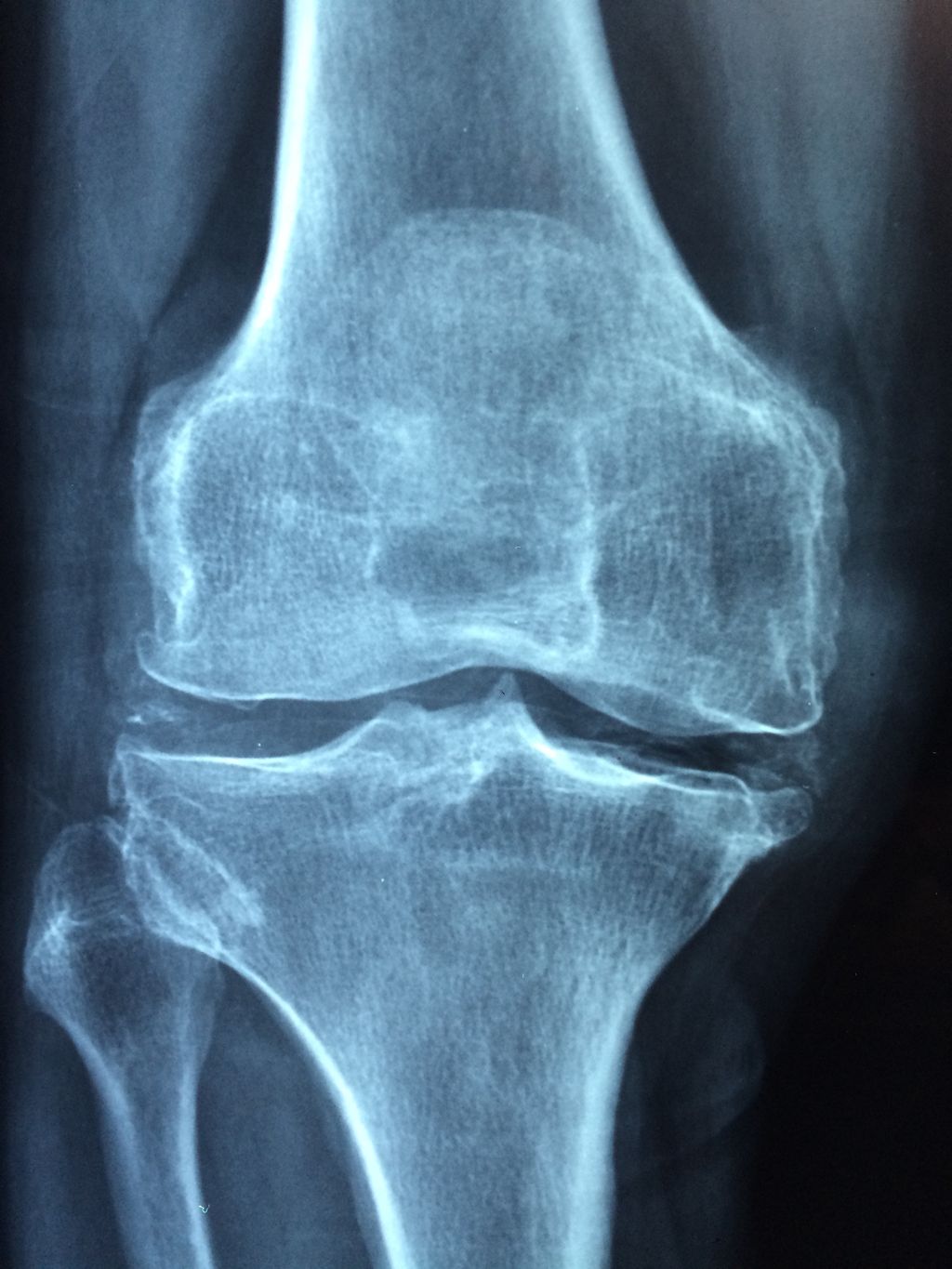
Imaging Studies
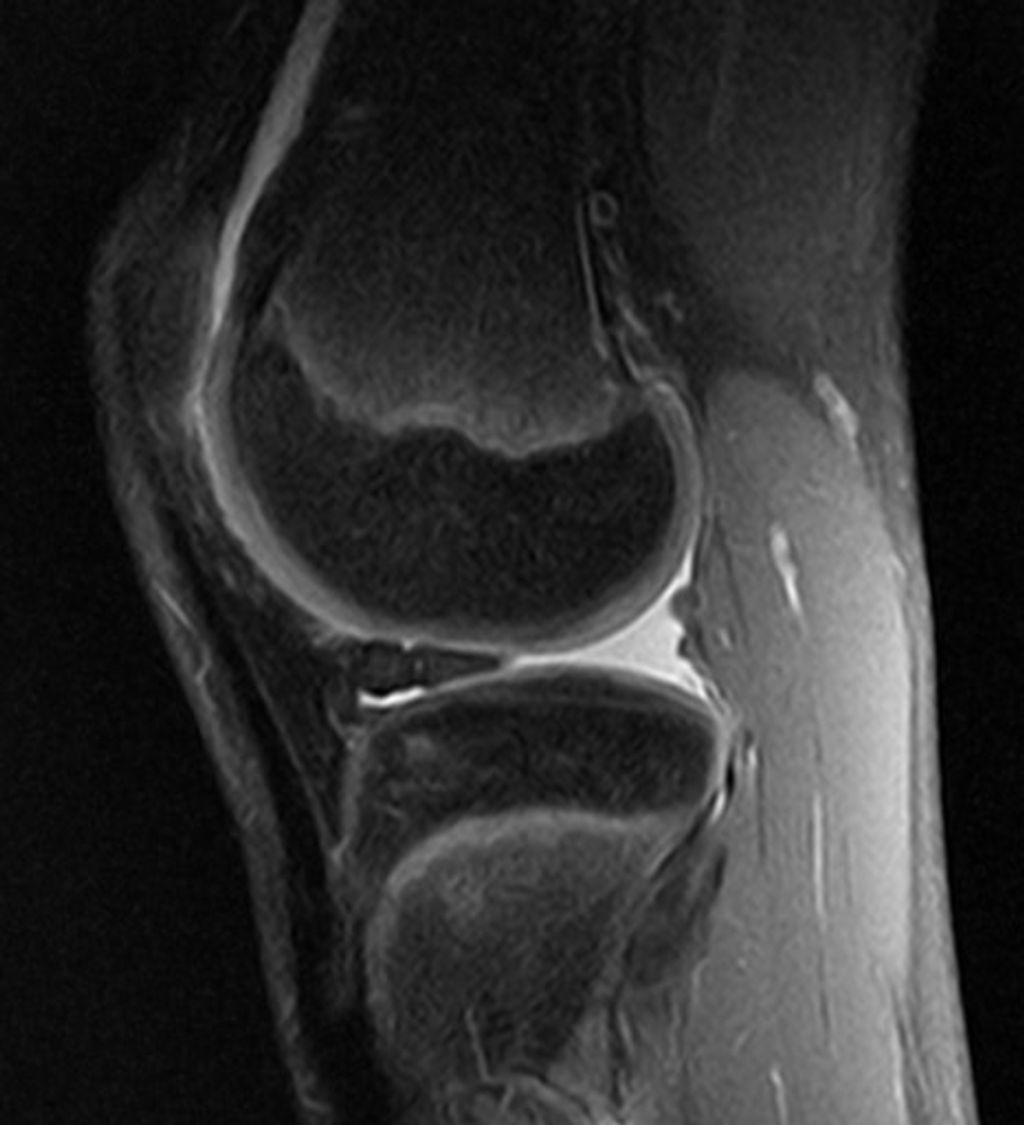
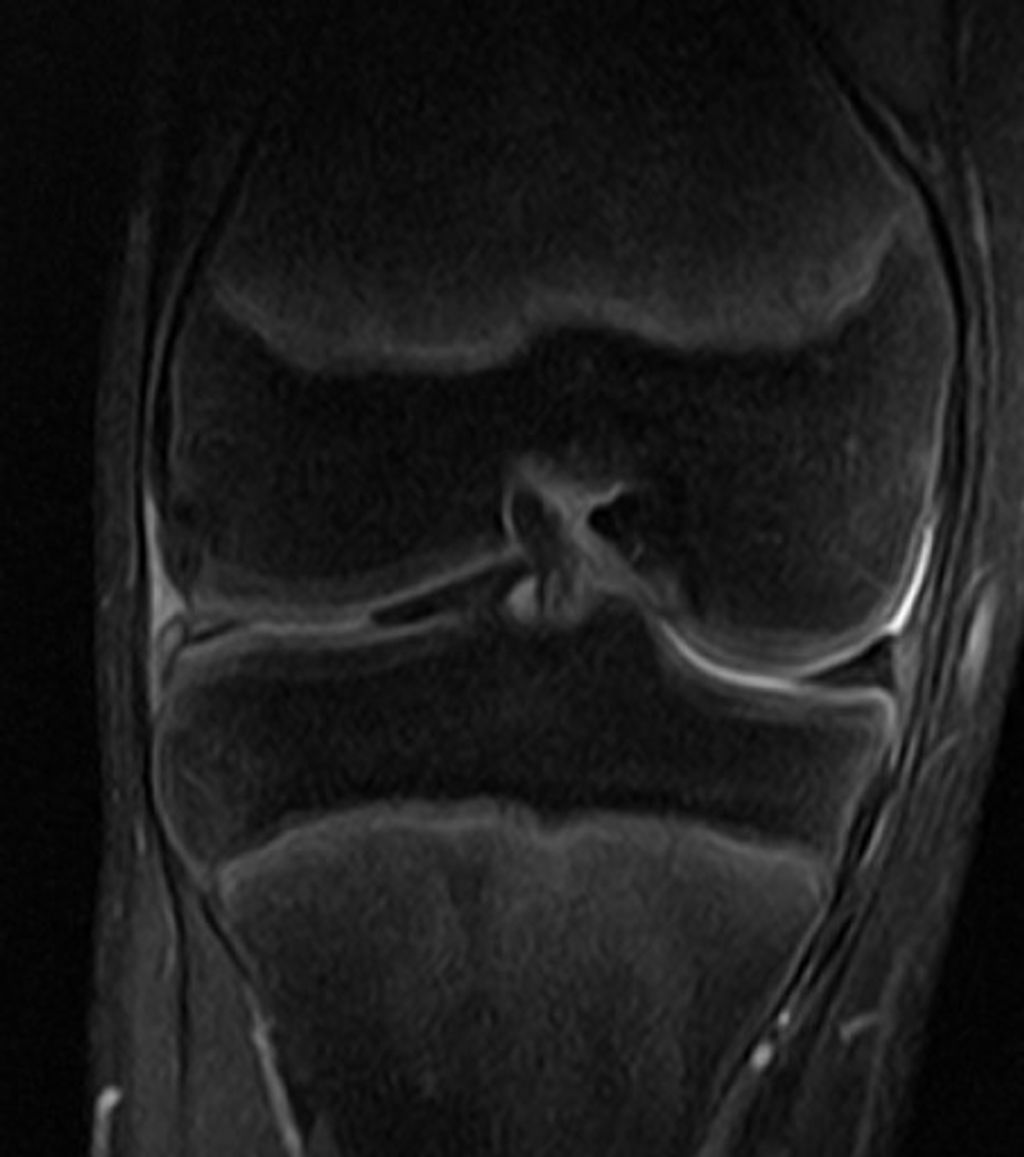
After undergoing the Imaging Studies, we can analyze the results to identify any abnormalities or structural issues in the knee joint. This analysis may involve comparing the images to standard measurements and reference values. For example, the size and alignment of the knee joint components can be assessed to determine any deviations from the norm. Additionally, the presence of any inflammation or fluid accumulation can be noted, providing valuable insights into the underlying causes of hot knees.
Furthermore, it may be beneficial to create a table summarizing the quantitative data obtained from the imaging studies. This table could include measurements of joint space, bone density, and any visible abnormalities. Such a structured presentation of data can aid in the comprehensive evaluation of the knee joint’s condition and guide further diagnostic and treatment decisions.
Lastly, it’s important to note that the interpretation of imaging studies should be performed by qualified healthcare professionals with expertise in musculoskeletal radiology and diagnostic imaging.
It is crucial to ensure that the imaging studies are of high quality and accurately capture the details of the knee joint. This can significantly impact the accuracy of the diagnostic findings and subsequent treatment recommendations.
Laboratory Tests
After conducting a thorough physical examination and reviewing the results of imaging studies, we proceed to perform laboratory tests to assess specific biomarkers and inflammatory markers. These tests provide valuable quantitative data that aid in confirming the presence of underlying inflammatory conditions or other pathologies. The results of these tests, including levels of C-reactive protein and erythrocyte sedimentation rate, play a crucial role in guiding the subsequent course of treatment and management strategies for hot knees. It is important to interpret these results in conjunction with the clinical presentation and imaging findings to ensure a comprehensive understanding of the patient’s condition. Additionally, the use of a bulleted list can effectively summarize the key laboratory tests:
Treatment Options for Hot Knees

Medication and Pain Management
In our quest to alleviate the discomfort associated with hot knees, we often turn to medication and pain management strategies. These approaches are designed to reduce inflammation, alleviate pain, and improve joint function. It’s essential to strike a balance between effective pain relief and the minimization of potential side effects.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are commonly prescribed to manage knee pain. However, for more severe cases, stronger painkillers may be necessary. We must be cautious, as researchers have highlighted concerns regarding the prescription of painkillers for inflammatory conditions due to a lack of evidence and the risk of serious side effects.
It is advisable to consider alternative treatments in conjunction with medication, such as disease-modifying antirheumatic drugs (DMARDs) and tailored exercise programs, to enhance outcomes and reduce dependency on painkillers.
Here is a list of common medications and their purposes in managing hot knees:
- NSAIDs: Reduce inflammation and alleviate pain
- Corticosteroids: Decrease severe inflammation
- Analgesics: Provide pain relief
- DMARDs: Slow disease progression and improve joint health
- Biologic agents: Target specific pathways in the inflammatory process
Physical Therapy and Rehabilitation
After undergoing a comprehensive physical examination and imaging studies, physical therapy and rehabilitation play a crucial role in the management of hot knees. Our treatment plan involves a combination of strengthening exercises, flexibility training, and low-impact activities to improve knee function and reduce discomfort. Additionally, we emphasize the importance of proper body mechanics and posture to prevent further strain on the knee joint.
Furthermore, a structured approach to rehabilitation is essential for achieving optimal outcomes. Our program includes a progressive exercise regimen tailored to individual needs, with a focus on restoring range of motion and building muscle strength. We also provide education on self-care techniques and lifestyle modifications to support long-term knee health.
For a more detailed overview of the rehabilitation program, please refer to the following table:
| Rehabilitation Program Components | Description |
|---|---|
| Strengthening Exercises | Target major muscle groups to improve stability and support for the knee joint. |
| Flexibility Training | Focus on enhancing joint mobility and reducing stiffness. |
| Low-Impact Activities | Incorporate gentle movements to maintain cardiovascular fitness without exacerbating knee discomfort. |
In addition to the structured program, it is important to note that consistency and compliance with the prescribed regimen are key factors in achieving successful rehabilitation outcomes. Our team is dedicated to providing ongoing support and guidance to ensure that each individual receives the best possible care for their hot knees.
Surgical Interventions
After considering all treatment options, surgical intervention may be recommended for severe cases of hot knees. This may involve procedures such as arthroscopy or knee replacement surgery. The decision to undergo surgery should be carefully discussed with a qualified orthopedic surgeon. It’s important to weigh the potential benefits against the risks and recovery process. Here is a brief overview of the surgical interventions:
| Procedure | Description |
|---|---|
| Arthroscopy | Minimally invasive procedure to diagnose and treat knee joint problems. |
| Knee Replacement Surgery | Surgical procedure to replace a damaged knee joint with an artificial implant. |
It’s essential to follow post-operative care instructions diligently to optimize recovery and minimize complications. Maintaining a healthy lifestyle and adhering to the prescribed rehabilitation program are crucial for successful outcomes. Patients should also be aware of potential risks and complications associated with surgical interventions, and seek guidance from their healthcare provider if any concerns arise.
Conclusion
In conclusion, hot knees can be caused by a variety of factors, including overuse, injury, and medical conditions. It is important to listen to your body and seek professional medical advice if you experience persistent knee heat. By addressing the underlying causes and implementing appropriate remedies, individuals can effectively manage and alleviate hot knee symptoms, thereby improving their overall quality of life.
Frequently Asked Questions
What are the common symptoms of hot knees?
Common symptoms of hot knees include warmth, redness, swelling, and pain in the knee joint.
Can hot knees be a sign of a serious medical condition?
In some cases, hot knees can indicate underlying inflammatory conditions or joint diseases that require medical attention.
How can I relieve hot knees at home?
Applying ice packs, elevating the knee, and resting can help relieve hot knees at home.
Are there specific exercises that can help with hot knees?
Low-impact exercises such as swimming, cycling, and gentle stretching can help improve knee mobility and reduce discomfort.
What are the potential complications of untreated hot knees?
Untreated hot knees can lead to chronic pain, joint damage, and limited mobility, affecting daily activities and quality of life.
When should I seek medical advice for hot knees?
It is advisable to seek medical advice if hot knees persist, worsen over time, or are accompanied by fever, severe swelling, or difficulty bearing weight on the affected knee.