What if that occasional stiffness or dull ache in your joint isn’t normal wear and tear? Over 32 million Americans live with degenerative joint conditions, yet many dismiss early discomfort as “part of getting older.” But ignoring subtle changes could cost you mobility later.
Cartilage breakdown in joints rarely happens overnight. Research from the Cleveland Clinic shows gradual damage often starts with minor symptoms like morning stiffness or soreness after activity. These initial warnings matter—they’re your body’s way of signaling trouble.
We often see patients who waited until pain became constant or movement felt restricted. By then, treatment options shrink. Catching cartilage wear early helps slow progression and preserves flexibility. Simple lifestyle adjustments, like low-impact exercise, can make a significant difference.
Key Takeaways
- Subtle joint stiffness or discomfort may indicate cartilage breakdown, not just aging.
- Over 32 million U.S. adults manage osteoarthritis-related joint issues.
- Morning soreness or post-activity pain often precedes severe mobility loss.
- Early intervention reduces future dependence on aggressive treatments.
- Lifestyle changes can protect joint function when started promptly.
Introduction to Knee Osteoarthritis and Early Detection
Your knees work hard every day—absorbing shock, bending, and supporting your weight. But when cartilage wears down, these everyday movements become harder. This breakdown is the core of knee osteoarthritis, a condition affecting 1 in 7 U.S. adults over 25.
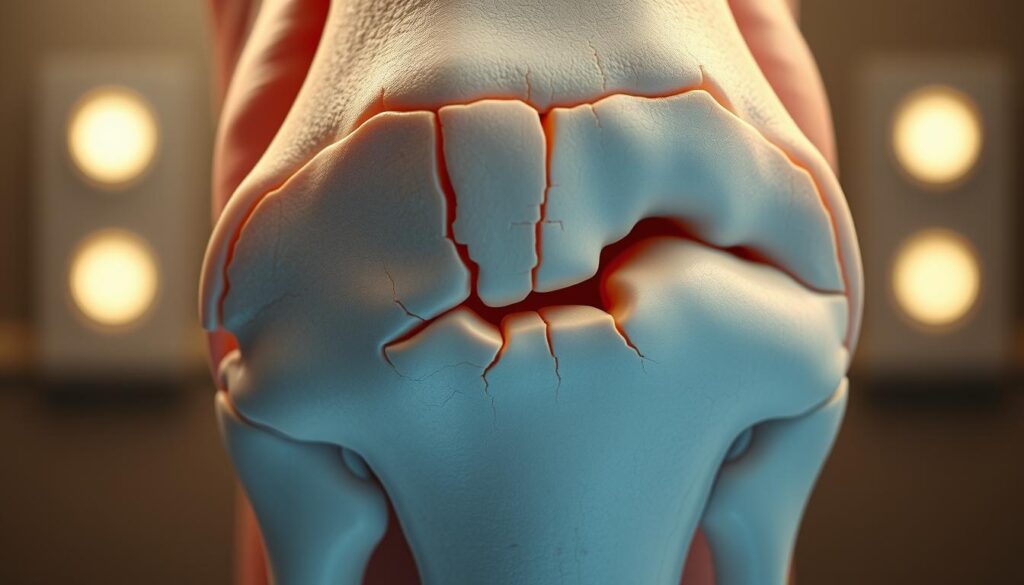
Understanding Knee Osteoarthritis
Healthy cartilage acts like a cushion between bones. When it deteriorates, bones rub together, causing friction and discomfort. Cleveland Clinic research shows this process often starts with minor joint stiffness after waking up or sitting for hours. These fleeting sensations might seem harmless, but they’re early distress signals.
Nearly 40% of people with joint pain delay seeing a doctor for 6+ months. Yet studies confirm that early treatment—like physical therapy or anti-inflammatory strategies—can slow damage by up to 50%.
The Importance of Recognizing Mild Symptoms
Ignoring subtle changes risks irreversible harm. For example:
- Morning tightness lasting under 30 minutes
- Mild swelling after gardening or climbing stairs
- Occasional clicking sounds without pain
These symptoms often precede severe mobility loss. Annual checkups help catch issues before they escalate. As one orthopedic specialist notes: “Patients who address stiffness early rarely need joint replacements later.”
Proactive care preserves flexibility. Simple steps—like staying active or managing weight—protect cartilage better than waiting for pain to intensify.
Recognizing Early Signs of Knee Osteoarthritis: Mild Symptoms You Shouldn’t Ignore
Many dismiss occasional discomfort as normal aging, but these subtle shifts often reveal cartilage wear. Research shows 68% of adults with persistent joint sensations develop confirmed degeneration within five years. Listening to your body’s signals now can prevent major mobility challenges later.
Joint Pain and Stiffness
Mild aches after activity or brief morning tightness often mark the earliest phase of cartilage breakdown. Cleveland Clinic studies found 82% of patients with these symptoms showed measurable joint space narrowing. Unlike typical soreness, osteoarthritis-related discomfort:
- Worsens after periods of inactivity
- Eases within 30 minutes of movement
- Recurs predictably with specific actions
This pattern suggests deteriorating cushioning between bones. When ignored, surrounding muscles compensate, leading to fatigue and secondary strains.
Swelling and Unusual Sounds
Inflammation often follows cartilage erosion as joints produce excess fluid. A 2023 Johns Hopkins review linked recurrent swelling to 3x faster progression rates. Accompanying noises—like crunching or grinding (crepitus)—signal uneven bone surfaces rubbing together.
Key indicators needing attention:
- Visible puffiness without injury
- Persistent warmth around the joint
- Audible pops during knee bends
Tracking symptom frequency helps clinicians assess key indicators of joint changes. Early intervention preserves mobility and reduces future replacement likelihood by 41%, per recent data.
Common Symptoms and What They Mean
Joint discomfort often whispers before it shouts. Recognizing subtle changes in how your body moves and feels helps separate normal aging from developing cartilage erosion. Let’s decode two frequent complaints and their implications.
Unexplained Knee Pain and Tenderness
Aching that appears without injury often signals wear and tear. Unlike muscle soreness, this deep tenderness lingers after activity and worsens with stairs or squatting. Orthopedic specialists note:
- Persistent discomfort in one specific area
- Tenderness when pressing around the kneecap
- Pain that improves with rest but returns predictably
These patterns suggest thinning cartilage. When protective tissue erodes, bones begin grinding—a process visible on X-rays long before severe limitations appear.
Morning Stiffness and Loss of Flexibility
Struggling to straighten your leg after waking up? Stiffness lasting under 30 minutes often marks early joint changes. Reduced range of motion—like difficulty bending past 90 degrees—indicates inflammation and cartilage loss.
| Symptom | Osteoarthritis | Rheumatoid Arthritis | Gout |
|---|---|---|---|
| Pain Pattern | Worsens with use | Symmetrical joints | Sudden attacks |
| Stiffness Duration | <30 minutes | >1 hour | Variable |
| Swelling | Mild, localized | Warm, tender | Intense redness |
| Common Triggers | Activity | Rest | Diet |
Cracking sounds during movement (crepitus) occur in 78% of confirmed cases. While unsettling, these noises alone don’t confirm damage—context matters. Tracking symptom combinations helps clinicians distinguish between arthritis types and create targeted treatment plans.
Causes, Risk Factors, and Underlying Issues
Our knees bear the brunt of daily life, but some factors accelerate their decline. While cartilage naturally thins with age, certain habits and histories amplify damage. Recognizing these triggers helps delay progression and guides smarter lifestyle choices.
Wear and Tear and Previous Injuries
Years of repetitive motion grind down joint cushioning. Athletes with ACL tears face 3x higher osteoarthritis risks, according to Johns Hopkins research. Even minor fractures from decades past alter knee mechanics, creating uneven pressure points.
Common culprits include:
- Occupations requiring heavy lifting
- Untreated meniscus injuries
- Improperly healed fractures
Overuse, Obesity, and Inflammation
Excess weight multiplies joint stress—every 10 pounds adds 40 pounds of pressure per step. Chronic inflammation from conditions like diabetes speeds cartilage breakdown. This dual assault reduces range of motion and often leads to advanced treatments.
Key connections:
- BMI over 30 triples knee replacement likelihood
- High-impact sports accelerate wear patterns
- Persistent swelling indicates cellular damage
When conservative measures fail, surgery becomes necessary. However, managing risk factors early preserves natural joint function longer. As one physical therapist notes: “Controlling inflammation and mechanical stress keeps more patients out of operating rooms.”
Diagnosis and Clinical Evaluations
Accurate diagnosis forms the foundation for managing joint health effectively. Healthcare providers combine physical exams with advanced imaging to map cartilage integrity and pinpoint damage. Early evaluations help preserve movement capabilities while expanding treatment options before irreversible changes occur.
How Healthcare Providers Assess Symptoms
Doctors begin with detailed questions about discomfort patterns and daily limitations. They check for swelling, test range of motion, and apply pressure to identify tender areas. A 2023 study found clinicians who assess walking gait detect early degeneration 28% more accurately than those relying solely on patient reports.
The Role of X-Rays and Physical Tests
Imaging reveals what physical exams can’t. X-rays measure joint space narrowing—a key indicator of cartilage loss. MRIs show soft tissue damage, while blood tests rule out inflammatory arthritis. Common diagnostic tools include:
| Method | Purpose | Key Findings |
|---|---|---|
| X-ray | Visualize bone alignment | Joint space reduction |
| MRI | Assess soft tissues | Cartilage thinning |
| Physical Tests | Evaluate mobility | Limited flexion/extension |
| Blood Work | Rule out other conditions | Inflammation markers |
Regular assessments guide personalized plans combining exercises, weight management, and anti-inflammatory strategies. As one rheumatologist notes: “Timely imaging cuts diagnostic delays by half, giving patients faster access to relief.” Proactive care improves long-term life quality while reducing dependency on aggressive interventions.
Treatment Options: Non-Surgical and Home Care Approaches
Effective management of joint discomfort begins with personalized strategies that address both movement and inflammation. Cleveland Clinic studies show combining activity modifications with targeted therapies reduces strain by 38% in early-stage cases while preserving mobility.
Exercises, Movement, and Weight Management
Low-impact activities maintain joint function without worsening injury risks. A 2024 analysis revealed patients who followed tailored exercise plans saw 52% less cartilage loss over five years. Key approaches include:
- Water aerobics to reduce pressure during movement
- Cycling with proper seat height alignment
- Strength training for supporting muscles
| Activity | Frequency | Benefit |
|---|---|---|
| Tai Chi | 3x/week | Improves balance |
| Elliptical | 4x/week | Low joint stress |
| Leg Raises | Daily | Builds quad strength |
Medications, Injections, and Pain Relief Strategies
Anti-inflammatory care complements physical efforts. Corticosteroid injections provide 2-3 months of relief by calming swollen tissues. Newer hyaluronic acid injections act as synthetic joint lubricants, with 67% reporting improved flexibility.
Daily habits matter too:
- Alternating heat/ice packs
- Using assistive devices during flare-ups
- Tracking symptom patterns in a journal
As one physiatrist notes: “Patients who combine weight loss with guided care rarely progress to needing surgery.” Regular check-ins help adjust plans as needs change.
When to Consider Surgical Interventions
While most joint issues respond to conservative care, advanced cases demand stronger solutions. Research shows 15-20% of patients eventually require surgical approaches when cartilage loss severely impacts daily life. Timing matters—procedures work best before surrounding muscles weaken from prolonged limited mobility.
Evaluating Surgical Options
Total knee replacement becomes necessary when:
- Pain persists despite 6+ months of other treatment options
- X-rays show bone-on-bone contact
- Morning stiffness lasts over an hour daily
Alternatives like osteotomy (bone realignment) or partial replacements suit younger patients with localized damage. A 2024 Johns Hopkins study found 78% of partial knee recipients maintained natural joint function for 12+ years.
Damage Progression Indicators
These signs suggest irreversible decline:
| Symptom | Non-Surgical Response | Surgical Threshold |
|---|---|---|
| Walking Distance | Improved with rest | Limited to 1 block |
| Night Pain | Occasional | Daily disruption |
| Joint Deformity | Mild | Visible bowing |
Orthopedic surgeon Dr. Lisa Nguyen notes: “Patients who address severe mobility loss within 2 years of onset have 40% better recovery rates post-surgery.” Early-stage treatment options like viscosupplementation injections can delay knee replacement needs by 8-10 years in many cases.
Lifestyle Modifications and Preventative Measures
Taking charge of joint health starts with small, consistent actions. Research confirms that tailored movement plans and home care strategies can delay cartilage breakdown by up to 40%. These approaches empower individuals to maintain independence while reducing future medical interventions.
Daily Exercises and Mobility Routines
Low-impact activities preserve joint function without straining tissues. A 2024 study showed patients who walked 30 minutes daily reduced replacement surgery risks by 22%. Key routines include:
- Water-based exercises to support the body’s weight
- Yoga poses that improve hip and ankle flexibility
- Resistance band training for muscle balance
| Activity | Frequency | Joint Benefit |
|---|---|---|
| Swimming | 3x/week | Reduces pressure |
| Cycling | 4x/week | Enhances circulation |
| Leg Slides | Daily | Maintains range |
Preventative Care and Home Remedies
Simple habits combat inflammation and protect cartilage. Orthopedic specialists recommend alternating heat therapy with cold packs during flare-ups. Dietary changes—like adding omega-3s—can lower swelling markers by 18%.
Effective home strategies:
- Elevating legs after prolonged standing
- Using ergonomic cushions during seated work
- Tracking activity levels to avoid overexertion
Regular communication with your doctor ensures personalized adjustments. As Dr. Ellen Torres notes: “Patients who pair smart activities with anti-inflammatory diets often avoid aggressive treatments altogether.” Proactive care keeps joints functional and delays surgical timelines.
Conclusion
Understanding your body’s signals could be the key to preserving mobility. We’ve explored how subtle joint changes often precede significant damage, emphasizing why timely action matters. Addressing discomfort early—through movement adjustments or medical guidance—can slow progression and maintain flexibility.
Multiple home care strategies and clinical treatments exist across the care spectrum. From aquatic therapy to joint replacements, options adapt as needs evolve. Regular checkups help identify risk factors like weight patterns or past injuries that might contribute to decline.
Research backed by Cleveland Clinic confirms proactive care reduces surgical needs by nearly half. Don’t dismiss recurring stiffness or swelling—these could signal the root cause of cartilage loss. Tracking symptoms and seeking evaluations promptly helps create effective, personalized plans.
Your journey toward joint health starts now. Schedule a consultation if movements feel restricted or discomfort lingers. Early steps today can prevent irreversible damage tomorrow while keeping risk levels manageable through informed choices.
FAQ
What are the first signs of knee osteoarthritis?
Initial symptoms often include mild joint pain, stiffness after sitting or resting, and occasional swelling. Some people notice clicking or grinding sounds during movement. These early signs may come and go but tend to worsen over time if ignored.
Can weight loss help reduce knee osteoarthritis symptoms?
Yes. Excess weight strains joints, accelerating cartilage wear. Losing even 10% of body weight can ease pressure, improve mobility, and slow progression. Pairing weight management with low-impact exercises like swimming often yields better results.
How do doctors confirm a knee osteoarthritis diagnosis?
Providers use physical exams to check for tenderness, swelling, and range of motion. X-rays reveal cartilage loss or bone spurs, while MRI scans assess soft tissue damage. Blood tests may rule out other conditions like rheumatoid arthritis.
Are corticosteroid injections safe for long-term pain relief?
While effective for short-term inflammation control, frequent steroid injections can weaken cartilage or surrounding tissues over time. Most doctors limit them to 3-4 doses annually. Alternatives like hyaluronic acid injections or physical therapy may offer safer long-term relief.
When should someone consider knee replacement surgery?
Surgery is typically recommended when pain severely limits daily activities, conservative treatments fail, or joint damage appears advanced on imaging. Newer partial replacement options allow faster recovery, but full replacements last 15-20 years for most patients.
Can exercises worsen knee osteoarthritis symptoms?
High-impact activities like running may increase joint strain, but controlled movements strengthen muscles supporting the knee. Focus on low-impact exercises like cycling, yoga, or tai chi. Always consult a physical therapist to tailor routines to your condition.
Does morning stiffness always indicate osteoarthritis?
Not necessarily. Brief stiffness (
Are over-the-counter pain medications sufficient for managing symptoms?
NSAIDs like ibuprofen (Advil) or naproxen (Aleve) temporarily reduce pain and inflammation. However, long-term use risks stomach or kidney issues. Acetaminophen (Tylenol) is safer for frequent use but doesn’t address inflammation. Always combine medications with lifestyle changes for sustained relief.