Running is a popular cardio workout that offers numerous health benefits. However, it’s not uncommon for runners to experience sore knees after their runs. This discomfort can arise due to the stress placed on the knee joints and muscles during the activity. To ensure that you can continue enjoying your runs without unnecessary pain or injury, it’s essential to know how to soothe sore knees and prevent knee pain. In this article, we will explore effective techniques and strategies for knee pain relief and injury prevention that will keep you on track with your running routine.
Key Takeaways:
- Stretching the muscles around the knees before running can help prevent knee injuries.
- Strengthening the leg muscles and core, as well as incorporating plyometric exercises, can aid in preventing knee pain.
- Using cold therapy, taking breaks from running, and staying hydrated are important strategies for soothing sore knees after running.
- Resting the knee, applying ice therapy, and using supportive devices can provide relief from knee pain.
- Stretching and strengthening exercises, proper footwear, and maintaining a healthy weight contribute to better knee health and pain management.
Tips for Knee Pain Relief and Management
When experiencing knee pain after running, it’s important to take steps for pain relief and management. Resting the knee and avoiding activities that worsen the pain, such as running, squatting, or sitting for long periods, can help reduce discomfort. Applying ice to the knee for 20-30 minutes every 3-4 hours can help ease pain and swelling.
Using an elastic bandage or patellar straps to provide support to the knee can also be beneficial. Over-the-counter medications like ibuprofen or naproxen can help with pain and swelling, but should be used as directed and with caution.
Stretching and strengthening exercises, particularly for the quadriceps muscles, can aid in knee pain relief and prevention of future injuries. Additionally, shoe inserts, maintaining a healthy weight, and avoiding running on hard surfaces can contribute to better knee health and pain management.
Knee Pain Relief and Management Tips Summary:
| Tip | Description |
|---|---|
| Resting the Knee | Avoid activities that worsen the pain and provide the knee with adequate rest. |
| Applying Ice | Use ice therapy for 20-30 minutes every 3-4 hours to ease pain and reduce swelling. |
| Using Supportive Measures | Apply an elastic bandage or use patellar straps to provide support to the knee. |
| Over-the-Counter Medications | Take ibuprofen or naproxen as directed for pain and swelling relief. |
| Stretching and Strengthening | Include exercises that target the quadriceps muscles to alleviate knee pain and prevent future injuries. |
| Proper Footwear | Use shoe inserts to provide cushioning and support while running. |
| Maintaining a Healthy Weight | Reduce stress on the knee joints by maintaining a healthy body weight. |
| Avoiding Hard Surfaces | Choose running routes that are softer on the joints, such as grass or a track. |
Understanding Runner’s Knee and Its Causes
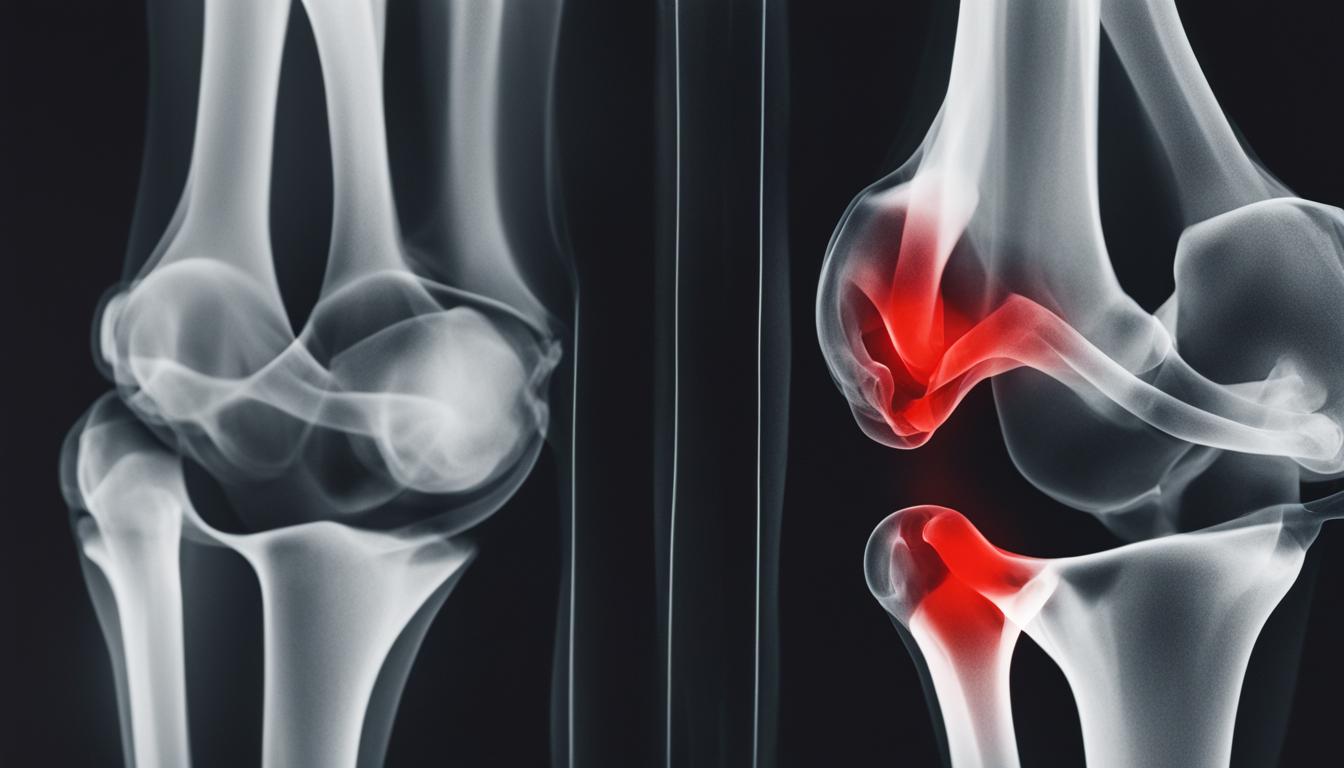
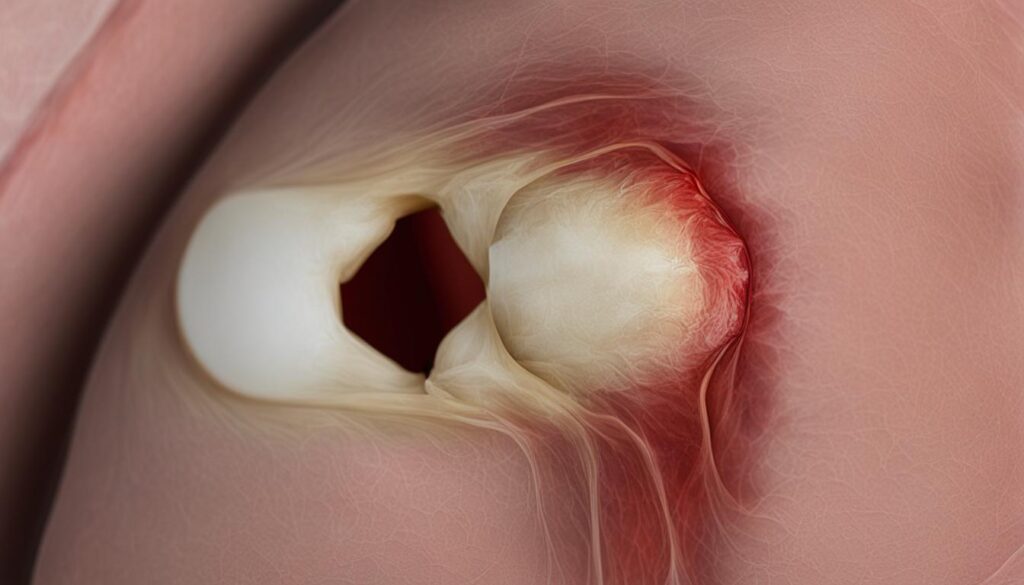
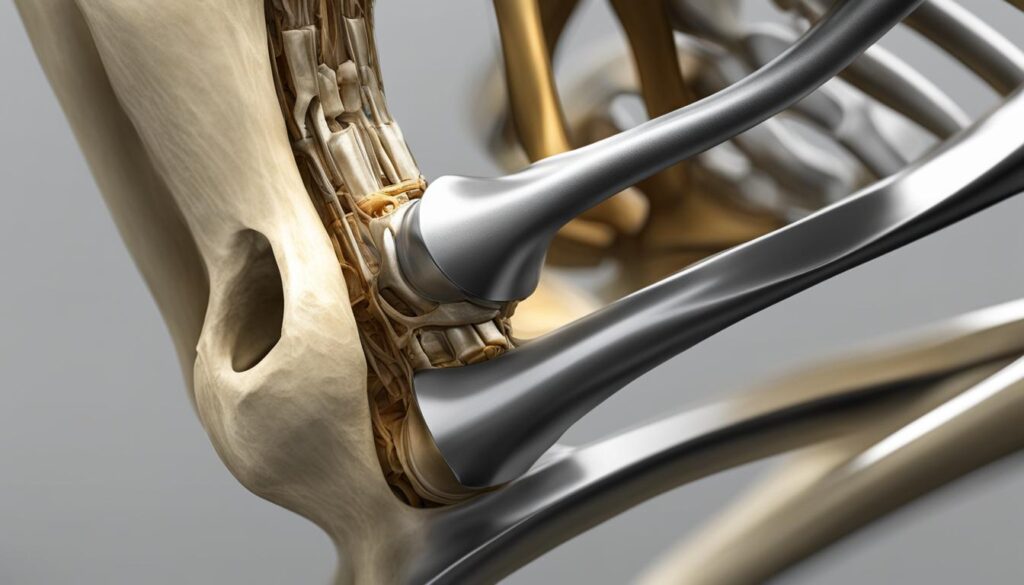
Runner’s knee, also known as patellofemoral pain syndrome, is a common condition that causes pain in the knees due to various underlying problems. It is often experienced by runners and athletes who frequently engage in activities that put stress on the knees. Understanding the causes of runner’s knee can help individuals recognize the risk factors and take appropriate measures to prevent and manage this condition.
There are several factors that contribute to the development of runner’s knee. Overuse, such as running long distances or participating in high-impact sports without proper rest, can lead to excessive stress on the knee joint. Direct impact to the knee, such as a fall or a blow, can also result in runner’s knee. Malalignment of the bones in the leg, foot problems, and weak thigh muscles can further increase the risk of developing this condition.
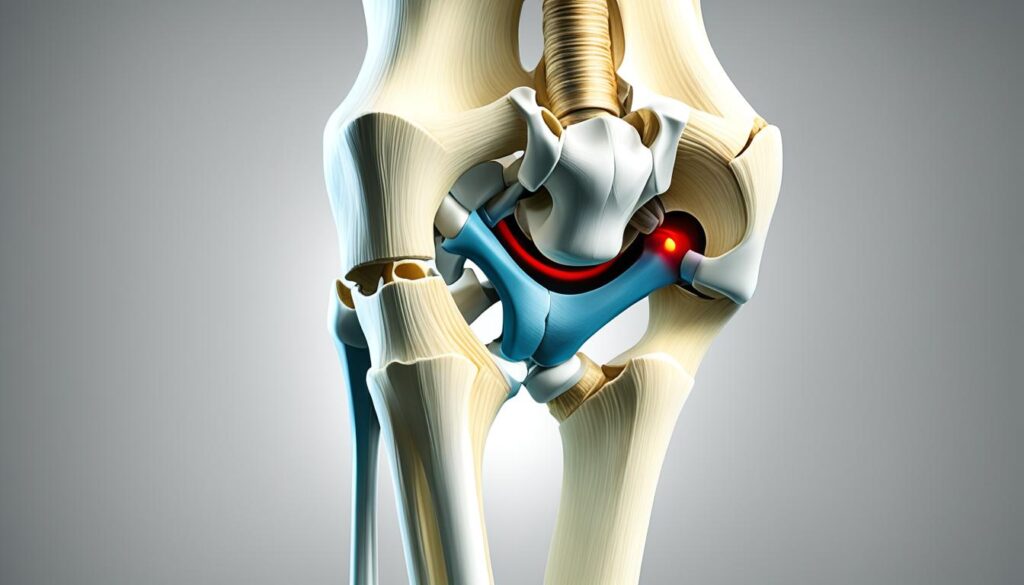
Common symptoms of runner’s knee include pain in the front of the kneecap that worsens with activities such as walking, squatting, and running. Individuals may also experience swelling and a grinding sensation in the knee. These symptoms can significantly impact daily activities and hinder participation in sports or exercise.
Diagnosing runner’s knee typically involves a physical examination by a healthcare professional who will evaluate the range of motion, stability, and alignment of the knee joint. In some cases, imaging tests such as X-rays may be used to rule out other possible causes of knee pain.
Treatment options for runner’s knee vary depending on the severity and underlying cause of the condition. Rest is crucial to allow the knee to heal and reduce inflammation. Applying ice therapy, wrapping the knee, and elevating the leg can help alleviate pain and swelling. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended for pain relief. Stretching and strengthening exercises, particularly targeting the quadriceps muscles, can improve knee stability and support recovery.
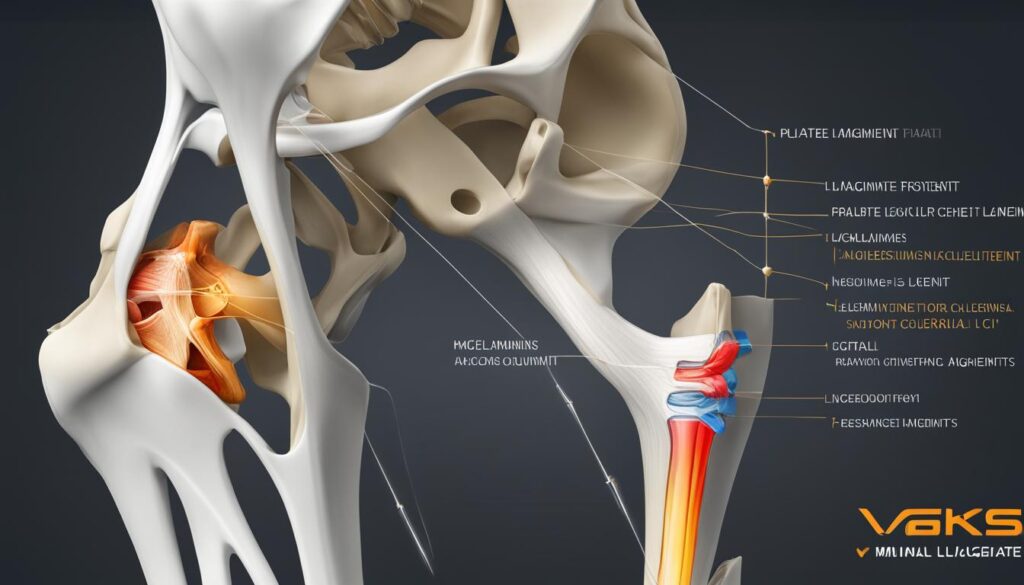
Proper footwear that provides adequate cushioning and support is essential for individuals with runner’s knee. Using orthotic inserts may help correct any foot alignment issues that contribute to knee problems. Additionally, paying attention to the body’s signals and modifying or avoiding activities that aggravate the knee pain can aid in managing and preventing runner’s knee.
It is essential for individuals experiencing knee pain to consult with a healthcare professional to receive an accurate diagnosis and appropriate treatment plan. With proper understanding, proactive measures, and guidance from healthcare providers, individuals can effectively manage runner’s knee and minimize its impact on their daily lives.

Recovery and Prevention Strategies for Runner’s Knee
Recovery from runner’s knee requires patience and proper care. It’s crucial to give the knee sufficient rest and avoid activities that worsen the pain. We must take proactive steps to alleviate symptoms and promote healing.
First and foremost, we recommend using ice therapy and elevating the affected knee to reduce swelling and discomfort. Applying an ice pack to the knee for 15-20 minutes several times a day can help alleviate pain. Elevating the leg while icing can further reduce swelling and promote blood circulation.

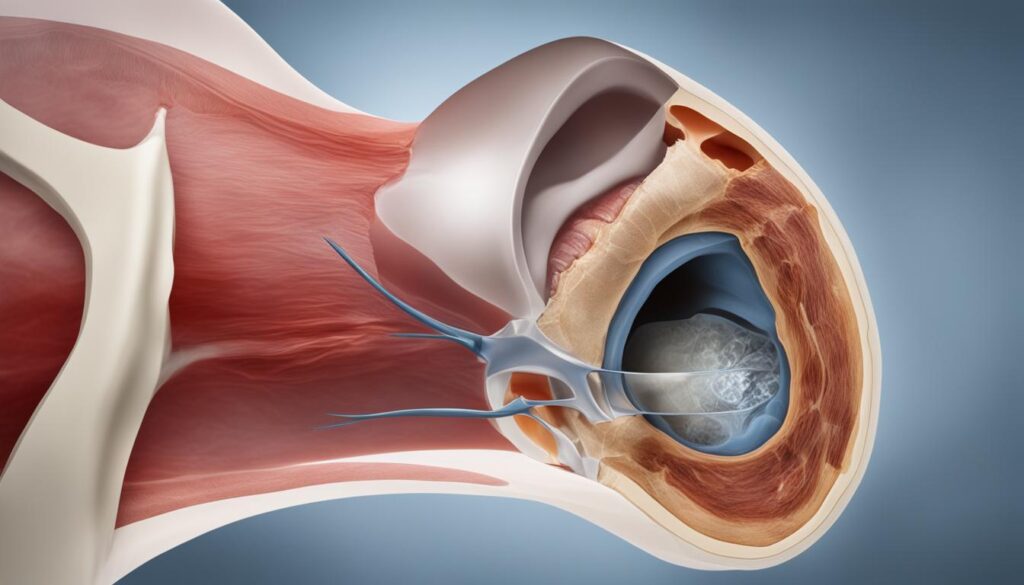
Proper footwear is also crucial in the recovery process. Using supportive shoes with adequate cushioning and arch support can minimize the stress on the knee joints and provide additional stability.
Stretching and Strengthening Exercises
Incorporating stretching and strengthening exercises into our routine is essential for both recovery and prevention of runner’s knee. We should gradually increase the intensity and duration of these exercises as the knee strengthens and pain subsides.
An important focus should be on strengthening the quadriceps muscles. These muscles, located in the front of the thigh, play a crucial role in knee stability. We recommend the following exercises:
- Leg extensions: Sit on a chair with your back straight and legs bent at a 90-degree angle. Extend one leg at a time, straightening the knee and holding for a few seconds before lowering it back down.
- Wall squats: Stand with your back against a wall and your feet shoulder-width apart. Slowly lower yourself into a sitting position, keeping your back against the wall and your knees aligned with your ankles. Hold for a few seconds, then push yourself back up to a standing position.
- Step-ups: Stand facing a step or bench. Step one foot onto the step, then bring the other foot up to join it. Step back down and repeat on the other side.
Remember to listen to your body and not push through any pain or discomfort during these exercises. Gradually increasing the intensity and repetitions will yield the best results without risking further injury.
Preventing Future Runner’s Knee
Taking steps to prevent runner’s knee in the future is equally important. By incorporating these strategies into our daily routine, we can minimize the risk of experiencing knee pain or injury again.
- Maintain a balanced exercise routine: It’s important to engage in a variety of activities that strengthen different muscle groups, including the legs, core, and hips. This helps prevent muscle imbalances that can lead to knee problems. Consider cross-training with low-impact exercises such as swimming or cycling.
- Use supportive shoe inserts: Custom orthotics or over-the-counter shoe inserts can provide additional support and cushioning for the feet, reducing stress on the knees.
- Avoid running on hard surfaces: Running on concrete or other hard surfaces increases the impact on the knees. Whenever possible, choose softer surfaces like grass or trails.
- Maintain a healthy weight: Excess weight puts additional strain on the knees. By maintaining a healthy weight through a balanced diet and regular exercise, we can reduce the risk of knee injuries.
Incorporating these post-run knee care strategies, performing knee strengthening exercises, and following injury prevention measures can significantly reduce the risk of runner’s knee and promote overall knee health. By taking care of our knees, we can continue to enjoy running and other physical activities without unnecessary pain or injury.
Conclusion
Sore knees after running can be a common issue, but with the right strategies for knee pain relief, management, and prevention, you can continue enjoying your favorite exercise while minimizing discomfort and reducing the risk of injuries.
One of the key aspects of post-run knee care is to focus on stretching and strengthening the muscles around the knees. Incorporating knee pain exercises and knee strengthening exercises into your routine can help improve the stability and flexibility of the knee joints, reducing the strain during running and preventing future injuries.
In addition to exercise, incorporating post-run knee care techniques like using cold therapy, taking breaks from running, and staying hydrated are crucial. Applying cold packs to the knees after a run can help reduce inflammation and alleviate pain. Taking breaks and allowing your knees time to rest and recover is important to prevent overuse and excessive strain. Staying hydrated ensures optimal joint lubrication, enhancing the overall health of the knees.
Understanding the causes of runner’s knee, such as weak thigh muscles or malalignment of the bones, is also vital. By implementing recovery and prevention strategies, such as gradually returning to physical activity, using proper footwear, and maintaining a balanced exercise routine, you can promote long-term knee health and reduce the risk of recurring knee pain.
Incorporating these tips into your routine will enable you to maintain healthy knees and continue pursuing your fitness goals with confidence. Remember, taking care of your knees is essential for a lifetime of pain-free running and overall well-being.
FAQ
What can I do to soothe sore knees after running?
To soothe sore knees after running, you can try using cold therapy, such as applying ice to the knee for 20-30 minutes every 3-4 hours. It’s also important to take breaks from running and give your knees time to rest and recover. Staying hydrated and stretching the muscles around the knees can also help alleviate discomfort.
What are some tips for knee pain relief and management?
To relieve and manage knee pain, it’s important to rest the knee and avoid activities that worsen the pain. Applying ice to the knee, using an elastic bandage or patellar straps for support, and taking over-the-counter medications like ibuprofen or naproxen can help reduce pain and swelling. Stretching and strengthening exercises, particularly for the quadriceps muscles, can aid in pain relief and prevention of future injuries.
What is runner’s knee and what causes it?
Runner’s knee, also known as patellofemoral pain syndrome, is a condition characterized by pain in the front of the kneecap. It can be caused by overuse, direct impact to the knee, malalignment of the bones, foot problems, or weak thigh muscles. Activities like walking, squatting, and running can worsen the pain, and symptoms may include swelling and a grinding sensation in the knee.
What are some recovery and prevention strategies for runner’s knee?
Recovery from runner’s knee requires rest and proper care. It’s important to give the knee sufficient rest and avoid activities that worsen the pain. Applying ice therapy, elevating the knee, and wearing proper footwear can help reduce swelling and alleviate symptoms. Gradually returning to physical activity and incorporating stretching and strengthening exercises, especially for the quadriceps muscles, can aid in the recovery process. To prevent runner’s knee in the future, maintaining a balanced exercise routine, using supportive shoe inserts, avoiding running on hard surfaces, and staying in shape with regular exercise are recommended.
How can I prevent knee injuries and care for my knees after running?
To prevent knee injuries, it’s important to stretch the muscles around the knees before running, focusing on the quadriceps, hamstrings, and calves. Strengthening the leg muscles and core, as well as incorporating plyometric exercises, can also help prevent knee injuries. After running, it’s crucial to take care of your knees by using cold therapy, taking breaks from running, and staying hydrated. Additionally, maintaining a healthy weight, using shoe inserts, and avoiding running on hard surfaces can contribute to better knee health and injury prevention.