Rehabilitation Exercises for Knee Ligaments: Strengthening and Recovery Techniques
As physical therapists, we often see patients with knee ligament injuries. Knee ligaments are strong bands of tissue that connect the thighbone to the shinbone and provide stability to the knee joint. Injuries to knee ligaments can result in pain, swelling, and decreased range of motion. Rehabilitation exercises for knee ligaments can help improve joint stability, reduce pain, and restore function.

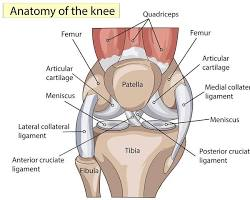
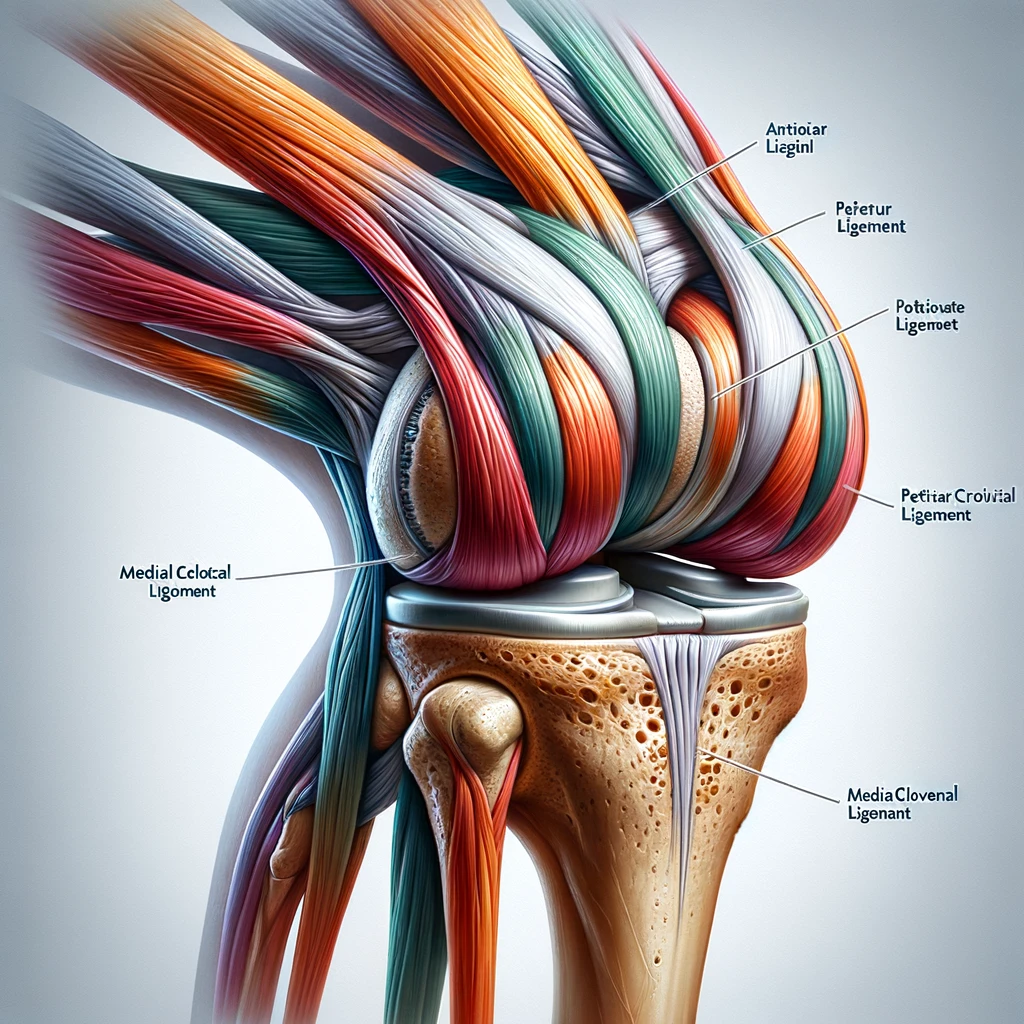
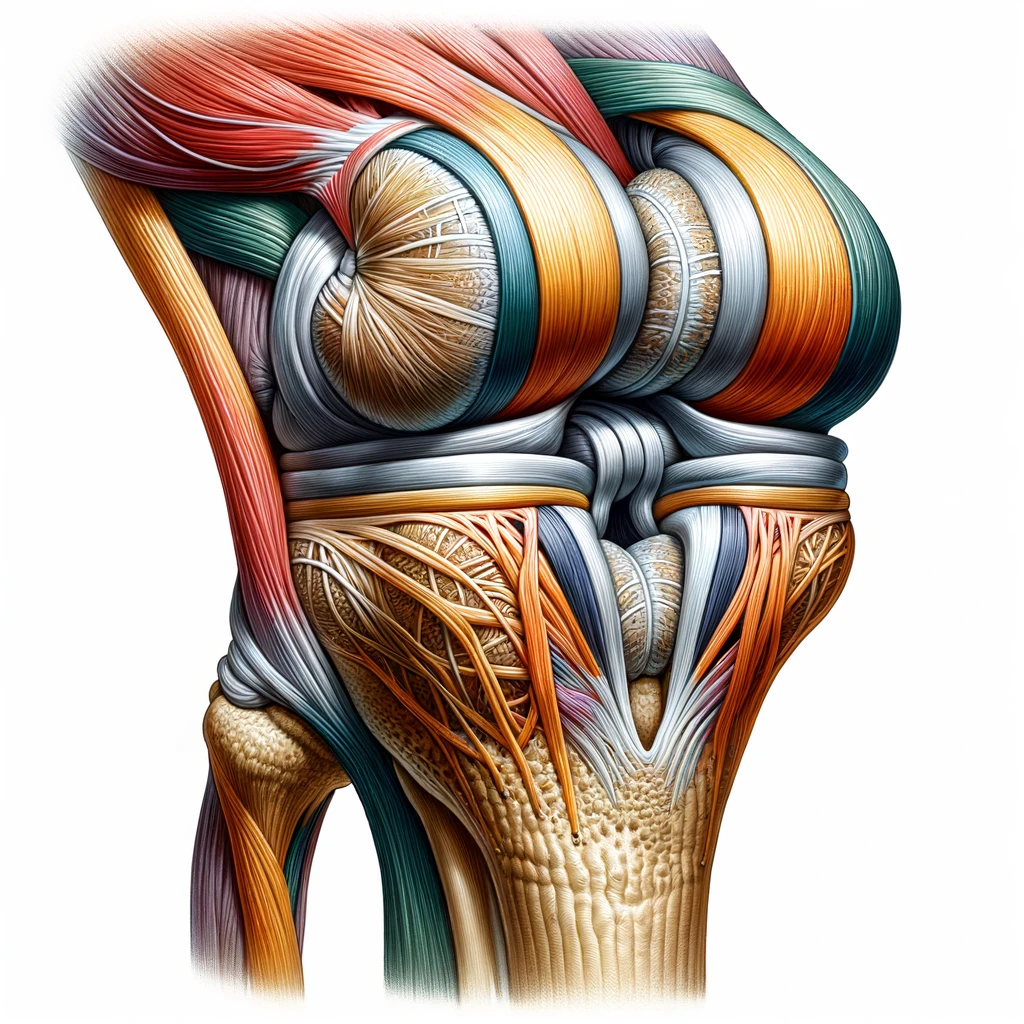
Understanding Knee Ligament Injuries is important for developing an effective rehabilitation plan. There are four main ligaments in the knee joint: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). ACL and PCL injuries are more common in athletes and can occur during sports that involve sudden stops, changes in direction, or jumping. MCL and LCL injuries can result from a direct blow to the knee or from twisting the knee. Depending on the severity of the injury, surgery may be required to repair or reconstruct the damaged ligament.

In this article, we will discuss 6 Rehabilitation Exercises for Knee Ligaments that can help improve joint stability, reduce pain, and restore function. These exercises are designed to strengthen the muscles that support the knee joint and improve biomechanical function. By following a structured rehabilitation program, patients can improve their recovery and return to their daily activities faster.
Key Takeaways
- Knee ligament injuries can result in pain, swelling, and decreased range of motion.
- There are four main ligaments in the knee joint: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL).
- Rehabilitation exercises for knee ligaments can help improve joint stability, reduce pain, and restore function.
Understanding Knee Ligament Injuries
Knee ligament injuries are common among athletes and individuals who engage in physical activities. These injuries can be caused by a wide range of factors, including trauma, overuse, and sports-related injuries. The most common types of knee ligament injuries include anterior cruciate ligament (ACL) injuries, medial collateral ligament (MCL) injuries, and posterior cruciate ligament (PCL) injuries.
Causes and Types of Injuries
ACL injuries are typically caused by a twisting motion or a direct blow to the knee. MCL injuries, on the other hand, are often caused by a direct blow to the outside of the knee. PCL injuries are usually the result of a direct blow to the front of the knee or a hyperextension injury.
Ligament injuries can be classified as either partial or complete tears. Partial tears involve damage to a portion of the ligament, while complete tears involve a complete separation of the ligament from the bone. Overuse injuries, such as tendinitis, can also occur in the knee.
Diagnosis and Assessment
Diagnosis of knee ligament injuries involves a physical examination, imaging tests, and other diagnostic procedures. Physical examination involves assessing the knee for pain, swelling, and instability. Imaging tests such as magnetic resonance imaging (MRI), radiographs, and ultrasound can also be used to assess the extent of the injury.
Treatment Options
Treatment options for knee ligament injuries depend on the severity of the injury. Nonoperative treatment may involve rest, ice, compression, and elevation (RICE), physical therapy, and immobilization. Operative treatment may involve surgery, such as arthroscopy or ACL reconstruction.
Post-Injury Challenges
Post-injury challenges may include pain, swelling, and instability. Rehabilitation is essential for restoring full function and reducing the risk of future injuries.
Understanding the Rehabilitation Process
Rehabilitation is an essential part of the recovery process for knee ligament injuries. The rehabilitation process involves a series of exercises and other interventions designed to improve muscle strength, proprioception, and joint stability.
Specific Rehabilitation Exercises
Specific rehabilitation exercises may include exercises to improve muscle strength, such as knee flexion and extension exercises, as well as exercises to improve proprioception, such as balance training.
Role of Imaging in Rehabilitation
Imaging tests such as MRI and radiographs can be used to assess the extent of the injury and monitor progress during rehabilitation.
Rehabilitation Exercises for Knee Ligament Recovery
| Exercise | Description | Target Area |
|---|---|---|
| Passive Range of Motion | Gentle movements of knee by therapist/device to improve flexion/extension early post-injury without overstressing | Restore mobility; reduce stiffness |
| Quad Sets | Contract quad muscles by pushing knees down into floor/table when in sitting/lying position | Activate quads; prevent atrophy |
| Straight Leg Raises | Tighten quads to lift straight leg up off floor/bed, keep knee locked | Strengthen quads; knee stabilization |
| Hip Abduction/Adduction | Move legs outward/inward against resistance or body weight | Strengthen hip muscles supporting knee |
| Calf Raises | Raise up onto ball/toes of foot, lower with control | Strengthen calves; improve balance/proprioception |
| Wall Sits | Slide down wall until knees/hips at 90 degree angle, hold position | Strengthen quads; improve endurance |
| Terminal Knee Extensions | Sit with resistance band around foot, fully straighten knee | Regain full extension range of motion |
| Hamstring Curls | Flex knees to pull heels toward buttress against resistance band | Strengthen hamstrings; decelerate knee extension |
| Balance Board/Wobble Board | Stand with knee slightly bent on unstable surface | Enhance balance and knee proprioception |
| Mini-Squats | Perform slight squatting motion within pain-free range of motion | Regain quad control; restore movement pattern |
The exact exercises and progressions are tailored by physical therapists depending on injury specifics, graft type, and post-surgical timeline. The goal is to restore strength, mobility, proprioception and movement control safely based on healing constraints

Preventing Future Injuries
Preventing future knee ligament injuries involves proper conditioning, warm-up, and cool-down exercises, as well as appropriate protective gear.
In conclusion, knee ligament injuries are common among athletes and individuals who engage in physical activities. Proper diagnosis, treatment, and rehabilitation are essential for restoring full function and reducing the risk of future injuries.