Knee pain can significantly impact an individual’s quality of life, affecting mobility and overall well-being. In this article, we will explore a comprehensive approach to managing knee pain, encompassing both non-surgical and surgical interventions. By understanding the anatomy and physiology of the knee, diagnostic techniques, and various treatment options, individuals can make informed decisions about their knee health.
Key Takeaways
- Understanding the structure of the knee joint is crucial for effective pain management.
- Physical examination, imaging modalities, and range of motion assessment are essential for accurate diagnosis of knee pain.
- Non-surgical treatment options such as physical therapy, pain management strategies, and lifestyle interventions play a key role in managing knee pain.
- Different types of knee surgery, post-surgery rehabilitation, and potential risks should be carefully considered when exploring surgical interventions for knee pain.
- A holistic approach to knee therapy involves addressing not only the physical aspects but also the nutritional and lifestyle factors that contribute to knee health.
Understanding Knee Pain: Anatomy and Physiology
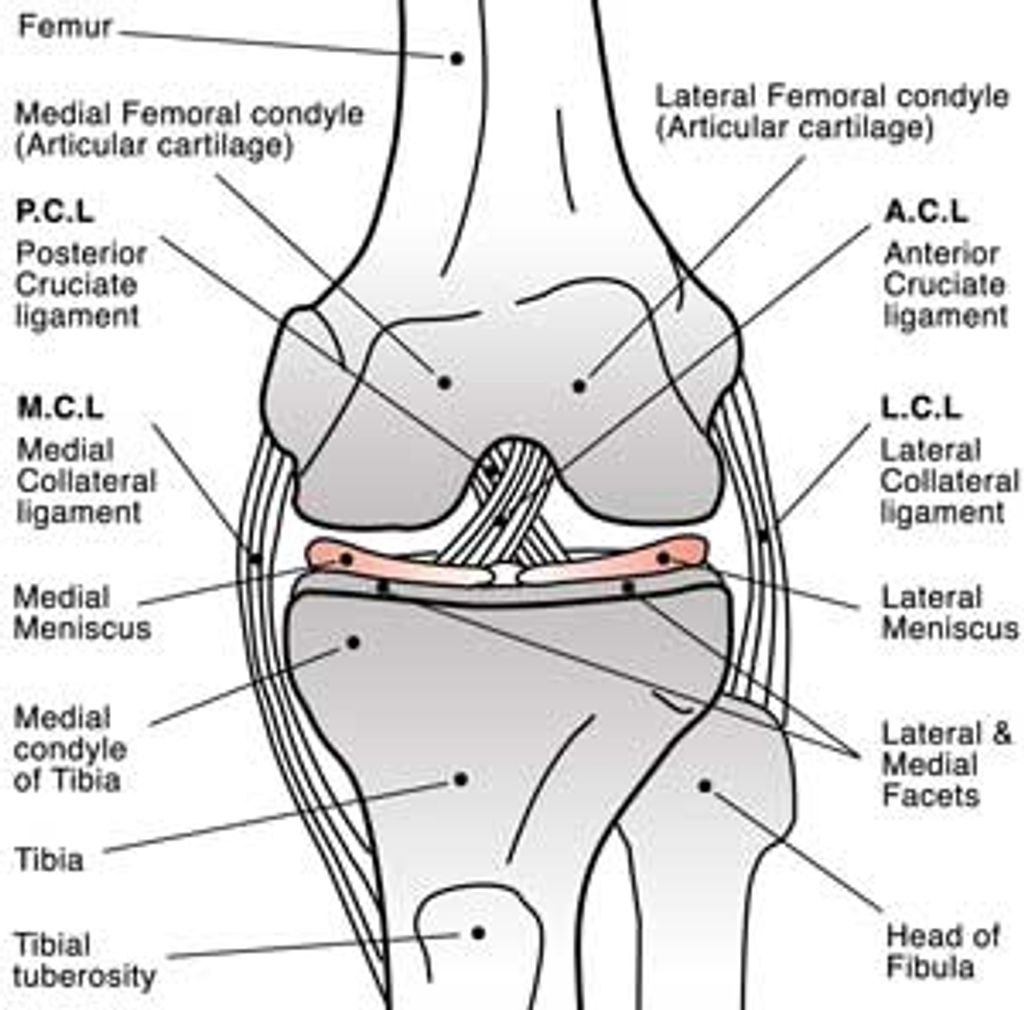
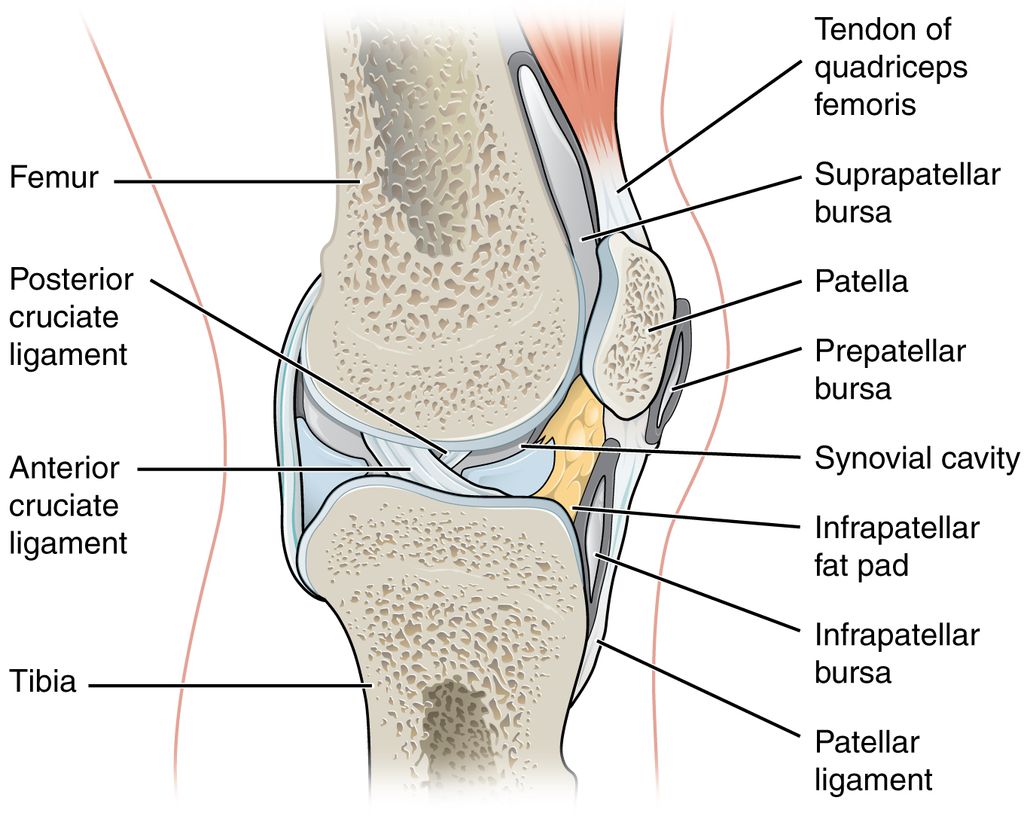
Structure of the Knee Joint
We recognize the knee joint as a complex hinge that allows for motion such as bending, straightening, and bearing weight. Its stability and movement are made possible by its unique structure, which includes bones, cartilage, ligaments, and tendons. The femur, tibia, and patella are the primary bones that form the knee joint, with the fibula also playing a supportive role.
The cartilage within the knee includes two types: the menisci, which act as shock absorbers, and the articular cartilage, which reduces friction. These components work in unison to ensure smooth and pain-free knee function.
- Menisci: Two C-shaped pieces of tough, rubbery cartilage.
- Articular Cartilage: Smooth, white tissue covering the ends of bones.
- Ligaments: Bands of tissue connecting bones.
- Tendons: Tissues attaching muscles to bones.
Tip: Maintaining strong muscles around the knee joint is crucial for its stability and can prevent injury. Regular exercise and weight management are key components of knee health.
Functions of Knee Ligaments and Tendons
In our exploration of knee pain, we recognize the critical role that ligaments and tendons play in the joint’s function. Ligaments are tough, elastic bands of tissue that connect bones to each other, providing stability and guiding the joint through proper movement. Tendons, on the other hand, attach muscles to bones, facilitating the transmission of forces that allow us to walk, run, and jump.
The knee joint is stabilized by a series of ligaments, including the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), which prevent the femur from sliding forward or backward on the tibia. The medial collateral ligament (MCL) and the lateral collateral ligament (LCL) provide stability against sideways motion. Tendons such as the patellar tendon play a pivotal role in knee extension, a necessary action for many daily activities.
Understanding the specific functions of each ligament and tendon can significantly enhance our approach to knee therapy. Here is a list of the primary knee ligaments and tendons along with their specific roles:
- Anterior Cruciate Ligament (ACL): Prevents forward sliding of the femur
- Posterior Cruciate Ligament (PCL): Prevents backward sliding of the femur
- Medial Collateral Ligament (MCL): Resists forces that would push the knee inward
- Lateral Collateral Ligament (LCL): Resists forces that would push the knee outward
- Patellar Tendon: Connects the patella to the tibia and enables knee extension
Tip: Regularly engaging in exercises that strengthen the muscles around the knee can help maintain the integrity of ligaments and tendons, potentially reducing the risk of injury.
Role of Muscles in Knee Stability
After understanding the role of muscles in knee stability, it is crucial to emphasize the importance of targeted strength training. This can help improve overall knee function and reduce the risk of injury. Additionally, proper nutrition plays a vital role in supporting muscle health and promoting recovery. A balanced diet rich in protein, vitamins, and minerals is essential for muscle repair and maintenance.
Furthermore, it is important to note that muscle imbalances can contribute to knee pain and instability. Addressing these imbalances through targeted exercises and physical therapy can help restore proper muscle function and improve overall knee stability.
Tip: Incorporating a variety of exercises that target different muscle groups can help achieve a well-rounded approach to muscle strength and stability.
Diagnostic Techniques for Knee Pain Assessment
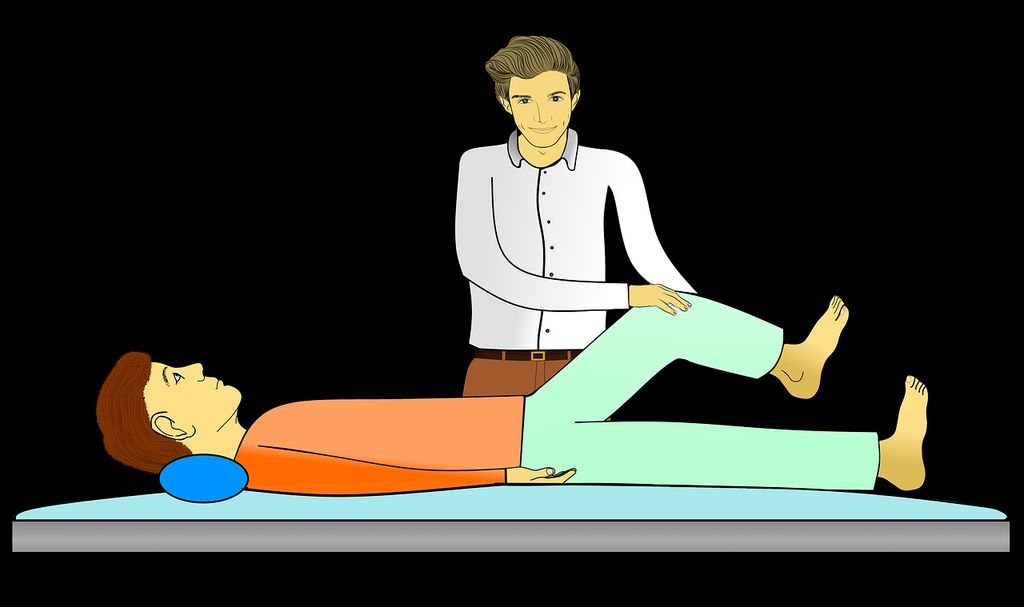
Physical Examination of the Knee
In our comprehensive approach to knee therapy, we place significant emphasis on the physical examination of the knee. This initial assessment is crucial in identifying the underlying causes of knee pain and determining the appropriate course of treatment.
During the examination, we systematically evaluate the knee’s structure, looking for signs of swelling, redness, warmth, and deformities. We palpate the joint to pinpoint areas of tenderness and assess the integrity of the ligaments and tendons.
Range of motion tests are performed to assess the knee’s flexibility and strength. We ask patients to perform specific movements while we observe for any limitations or discomfort that may indicate joint or muscular issues.
Remember, a thorough physical examination can often provide valuable insights that imaging alone cannot reveal.
The following list outlines the key components of a knee examination:
- Inspection for visual abnormalities
- Palpation to identify areas of pain or swelling
- Assessment of ligament stability
- Evaluation of meniscal integrity
- Measurement of range of motion and muscle strength
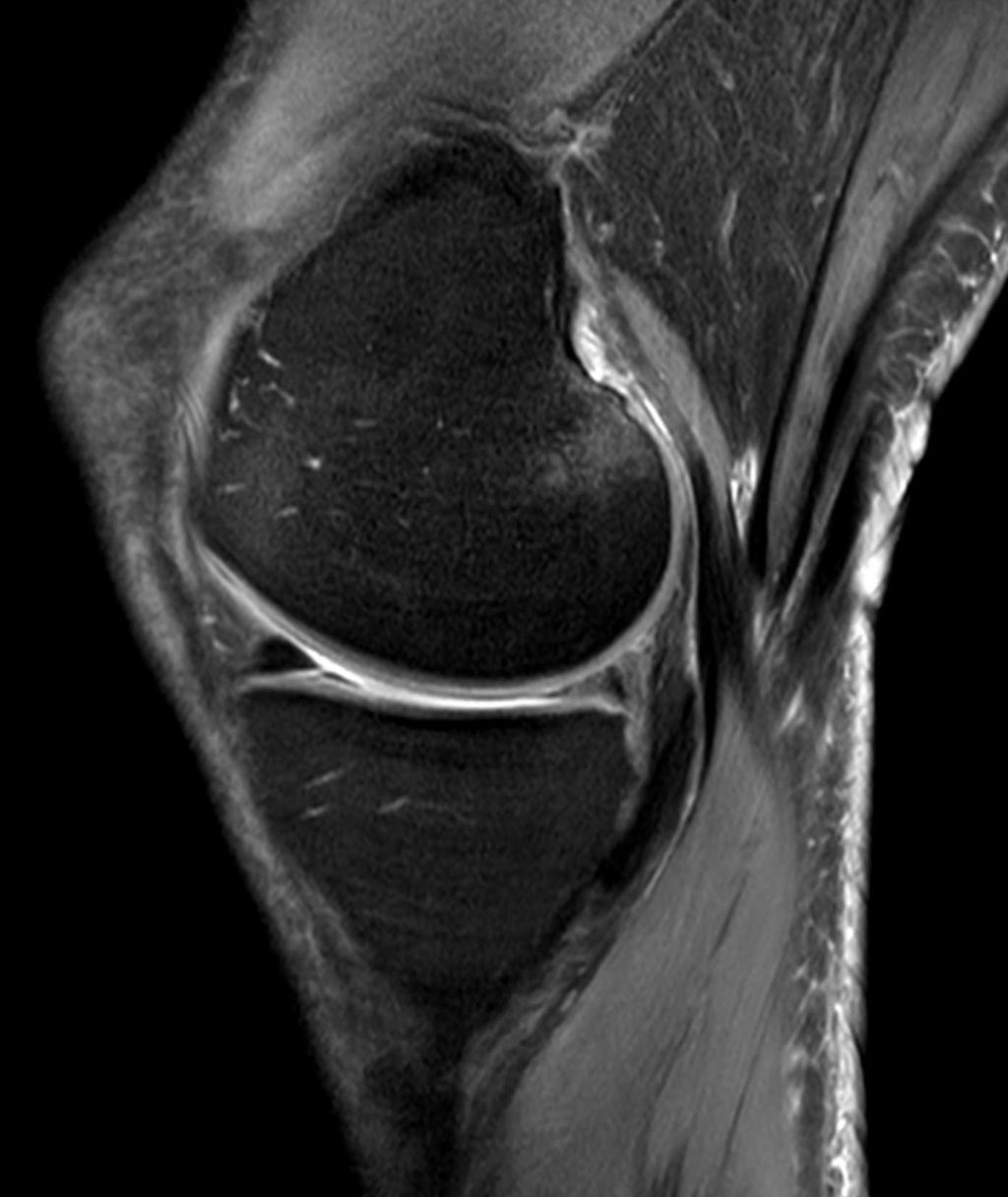
Imaging Modalities for Knee Evaluation
After conducting a thorough physical examination and considering the patient’s medical history, we utilize a variety of imaging modalities to further assess the condition of the knee. These modalities include X-rays, MRI scans, and CT scans. Each modality provides unique insights into the structural integrity and soft tissue health of the knee joint. We have found that MRI scans are particularly useful for evaluating ligament and meniscal injuries, while X-rays are valuable for assessing bone density and alignment. CT scans are employed when a more detailed view of bone structures is required. We prioritize the use of these imaging techniques to ensure a comprehensive understanding of the patient’s knee condition, guiding our treatment approach effectively.
Assessment of Range of Motion and Flexibility
After completing the physical examination of the knee, we move on to the assessment of range of motion and flexibility. This step is crucial in determining the extent of mobility and flexibility in the knee joint. We carefully measure the range of motion in different planes, including flexion, extension, and rotation. Additionally, we assess the flexibility of the surrounding muscles and ligaments to understand their ability to support the knee joint.
In our assessments, we use a combination of quantitative measurements and qualitative observations to gain a comprehensive understanding of the knee’s functional capabilities. This approach allows us to identify any limitations or abnormalities in the knee’s range of motion and flexibility.
For a more structured presentation of our findings, we utilize a table to document the quantitative measurements of range of motion in various planes. This table provides a clear overview of the knee’s mobility and helps in tracking changes over time, guiding our treatment plans effectively.
Non-Surgical Treatment Options for Knee Pain

Physical Therapy and Rehabilitation
After undergoing a thorough assessment, physical therapy and rehabilitation play a crucial role in our comprehensive approach to knee pain management. We focus on strengthening and flexibility exercises tailored to each individual’s needs, promoting optimal recovery and function. Additionally, we emphasize the importance of nutrition and lifestyle modifications to support the healing process.
- Implement a table for presenting structured, quantitative data. Ensure it’s succinct and formatted correctly in Markdown.
- Use a bulleted or numbered list for less structured content, like steps, qualitative points, or a series of related items.
It’s essential to adhere to the prescribed exercise regimen and lifestyle modifications to achieve the best outcomes and long-term relief from knee pain.
Pain Management Strategies
Pain management strategies are crucial in addressing knee pain. We emphasize a multidisciplinary approach that combines physical therapy, medication, and lifestyle modifications. Exercise is a cornerstone of our approach, focusing on strengthening and flexibility exercises to improve knee function. Additionally, we advocate for the use of non-steroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and reduce inflammation. Our holistic approach also includes nutritional guidance, emphasizing a diet rich in anti-inflammatory foods such as fruits, vegetables, and omega-3 fatty acids.
Furthermore, we encourage patients to maintain a healthy weight, as excess weight can exacerbate knee pain. We believe that a balanced and sustainable approach to pain management is essential for long-term relief and improved quality of life. It is important for patients to actively participate in their pain management plan, and we provide ongoing support and education to empower them in their journey to better knee health.
Nutritional and Lifestyle Interventions
In our journey to alleviate knee pain, we recognize the profound impact of nutritional and lifestyle interventions. A balanced diet rich in anti-inflammatory foods can significantly reduce joint inflammation and pain. We encourage the inclusion of omega-3 fatty acids, found in fish and flaxseeds, and antioxidants from fruits and vegetables. Adequate hydration is also crucial for joint health.
Exercise is a cornerstone of a healthy lifestyle and is particularly beneficial for those suffering from knee pain. Low-impact activities such as swimming, cycling, and walking can strengthen the muscles around the knee, improving stability and flexibility without exacerbating pain.
We must not overlook the importance of maintaining a healthy weight. Excess body weight puts additional stress on knee joints, which can aggravate pain and hinder recovery. Here’s a simple guideline to follow:
- Maintain a balanced diet with a focus on anti-inflammatory foods
- Engage in regular low-impact exercise
- Stay hydrated
- Aim for a healthy body weight
Tip: Consistency in these interventions is key to long-term pain management and joint health.
Surgical Interventions for Knee Pain Management
Types of Knee Surgery
When we consider surgical interventions for knee pain management, it’s essential to recognize the variety of procedures available. Arthroscopy is a minimally invasive technique that allows us to address issues within the joint with precision. For more severe cases, total knee arthroplasty, or knee replacement surgery, may be the most effective option to restore function and alleviate pain.
The choice of surgery is highly dependent on the individual’s condition and needs. Here’s a brief overview of common surgical procedures:
- Arthroscopy: Used for diagnosing and treating joint problems.
- Osteotomy: Alters bone structure to relieve pressure.
- Ligament Reconstruction: Repairs or replaces damaged ligaments.
- Total Knee Replacement: Replaces the entire knee joint.
Remember, the goal of surgery is not only to relieve pain but also to improve mobility and quality of life. Each procedure carries its own set of potential benefits and risks, which should be thoroughly discussed with a healthcare provider.
Rehabilitation Following Knee Surgery
After knee surgery, rehabilitation is crucial for a successful recovery. Our team focuses on personalized treatment plans tailored to each patient’s needs. We emphasize progressive exercises to improve strength, flexibility, and range of motion. Additionally, we provide education on proper body mechanics and gait training to promote optimal function. Our comprehensive approach includes a combination of manual therapy, therapeutic modalities, and functional training.
For a structured overview of the rehabilitation process, refer to the following table:
| Rehabilitation Components | Description |
|---|---|
| Progressive Exercises | Gradually increasing intensity and difficulty to promote recovery and function. |
| Education and Training | Providing guidance on proper movement patterns and functional activities. |
| Manual Therapy | Hands-on techniques to improve joint mobility, reduce pain, and enhance function. |
| Therapeutic Modalities | Application of modalities such as heat, cold, and electrical stimulation for pain management and tissue healing. |
| Functional Training | Focusing on activities of daily living and functional movements to restore independence and mobility. |
Our approach to rehabilitation is centered on empowering patients to actively participate in their recovery journey. We encourage open communication and collaboration to ensure the best possible outcomes. As part of our commitment to excellence, we prioritize patient education and support throughout the rehabilitation process.
Potential Risks and Complications
After undergoing knee surgery, we must be vigilant in monitoring for potential risks and complications. These can range from the more common, such as infections or blood clots, to the less frequent but serious issues like nerve damage or implant failure. It’s imperative to understand that every surgical procedure carries inherent risks, and knee surgeries are no exception.
Rehabilitation is a critical phase where patients must adhere to prescribed protocols to minimize the risk of complications. For instance, failure to properly rehabilitate can lead to stiffness, decreased range of motion, or even chronic pain, which could negate the benefits of the surgery.
Tip: Always follow your surgeon’s post-operative instructions and attend all follow-up appointments to ensure the best possible outcome.
While we strive to achieve a successful surgical outcome, we must also prepare for the possibility of revision surgery. This is particularly true in cases where the initial procedure does not yield the desired results or when complications arise that necessitate further intervention.
Conclusion
In conclusion, a comprehensive approach to knee therapy is essential for effective pain management. By addressing the physical, emotional, and lifestyle factors that contribute to knee pain, patients can experience holistic healing and long-term relief. This holistic approach emphasizes the importance of personalized care and a multidisciplinary treatment plan, ultimately leading to improved patient outcomes and quality of life. As the field of knee therapy continues to evolve, it is imperative to prioritize a holistic approach that considers the whole person, not just the symptoms. Embracing this approach can pave the way for advancements in pain management and overall well-being for individuals with knee-related concerns.
Frequently Asked Questions
What are the common causes of knee pain?
Common causes of knee pain include injuries, arthritis, overuse, and muscle imbalances.
How can physical therapy help with knee pain?
Physical therapy can improve strength, flexibility, and mobility, and reduce pain through targeted exercises and rehabilitation techniques.
What are the non-surgical options for managing knee pain?
Non-surgical options include physical therapy, pain management strategies, lifestyle modifications, and nutritional interventions.
What is the recovery process after knee surgery?
The recovery process involves rehabilitation, physical therapy, and gradual return to normal activities, with a focus on reducing pain and restoring function.
What are the potential risks of knee surgery?
Potential risks include infection, blood clots, nerve damage, and prolonged recovery time, among others. Your surgeon will discuss these risks with you before the procedure.
How can I prevent knee pain and injuries?
Preventive measures include maintaining a healthy weight, staying active, using proper footwear, and practicing good posture and body mechanics during physical activities.