Welcome to our comprehensive guide on effective knee osteoarthritis treatment options. If you or a loved one is struggling with knee pain, stiffness, and reduced quality of life, this article is for you. We understand the challenges that knee osteoarthritis presents and the importance of finding the right solutions to manage symptoms and improve joint function.
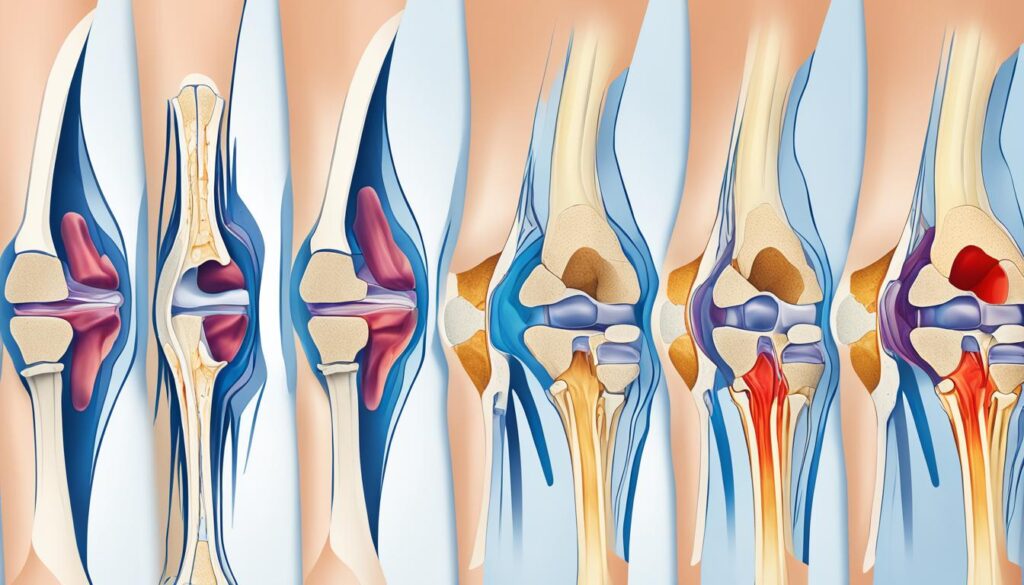
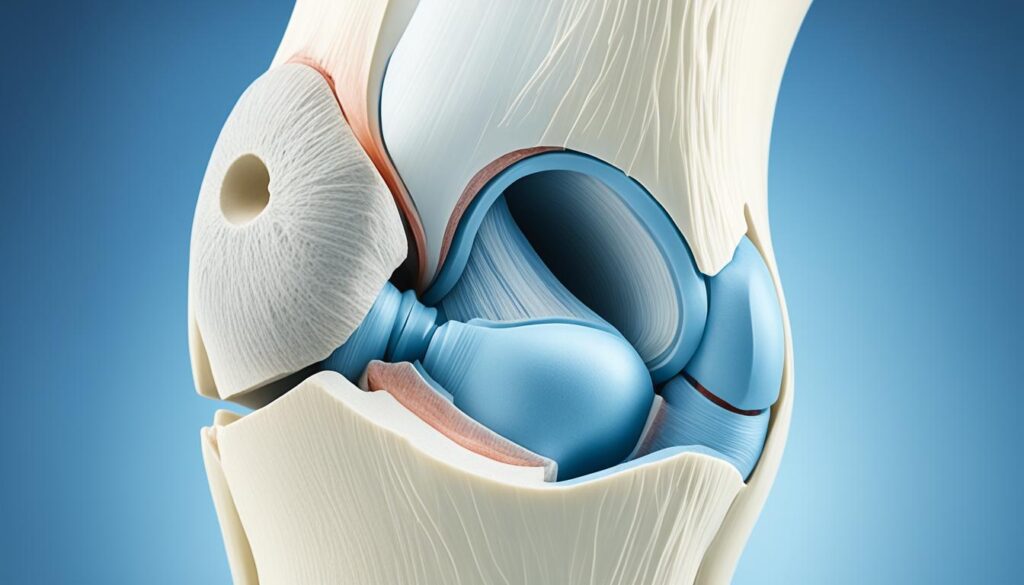
Knee osteoarthritis is a degenerative joint disease that primarily affects older adults. It is the most common condition affecting synovial joints and can cause pain, disability, and a decrease in quality of life. But the good news is that several treatment options are available to provide knee pain relief and help you manage knee osteoarthritis effectively.
In this article, we will explore various treatment approaches, including physical therapy, medications, injections, surgery, and alternative therapies. Each option aims to reduce pain, improve joint function, and enhance overall well-being. By understanding these treatment options, you can work with your healthcare professional to develop a personalized treatment plan that addresses your specific needs and goals for managing knee osteoarthritis.
So, whether you are looking for non-invasive methods to alleviate knee pain or considering surgical interventions, we’ve got you covered. Stay with us as we delve into the details of each treatment option, providing you with the information you need to make informed decisions about managing knee osteoarthritis.
Let’s explore effective knee osteoarthritis treatment options together and regain control over your knee health.
Physical Therapy for Knee Osteoarthritis
Physical therapy is an essential component of knee osteoarthritis management. It involves a range of exercises and techniques designed to strengthen the muscles supporting the knee, improve flexibility, and alleviate pain. Incorporating physical therapy into your treatment plan can significantly enhance your overall well-being and help you regain control over your knee health.
There are various types of physical therapy exercises that have proven to be effective in alleviating pain and disability caused by knee osteoarthritis. These include:
- Water-based and land-based exercises
- Aerobic walking
- Quadriceps strengthening exercises
- Resistance exercises
Additionally, tai chi, a mindful movement practice, has shown promising results in reducing pain and improving physical functioning in older women with knee osteoarthritis.
To develop a personalized exercise program tailored to your specific needs and goals, it is crucial to consult with a physical therapist. They will assess your condition, create a customized plan, and provide guidance and support throughout your rehabilitation journey.

Comparison of Physical Therapy Exercises
| Exercise Type | Benefits |
|---|---|
| Water-based exercises | Low impact, reduced joint stress, improved range of motion |
| Land-based exercises | Strengthening muscles, increased stability, improved joint function |
| Aerobic walking | Cardiovascular fitness, weight management, enhanced mobility |
| Quadriceps strengthening exercises | Improved leg strength, reduced pain, enhanced knee stability |
| Resistance exercises | Increased muscle strength, improved overall joint functioning |
Medications for Knee Osteoarthritis
Medications can play a crucial role in providing pain relief and managing the symptoms of knee osteoarthritis. When it comes to treating knee pain, there are several medications available that can effectively reduce pain, swelling, and stiffness associated with this condition.
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are commonly used to alleviate knee pain. These medications work by reducing inflammation in the affected joint, providing relief from pain and discomfort.
Acetaminophen is another option for pain relief and is recommended as the first-line treatment by the American College of Rheumatology. It is a non-prescription medication that can help manage mild to moderate knee pain. However, it is important to note that acetaminophen does not have anti-inflammatory properties.
For individuals with more severe pain, a healthcare professional may prescribe stronger medications. This may include prescription NSAIDs, such as meloxicam or diclofenac, which are similar to over-the-counter NSAIDs but with higher potency. Other medications, such as duloxetine, an antidepressant that also helps reduce pain, may be considered for individuals with persistent and severe knee pain.
It is essential to consult with a healthcare professional before starting any medication for knee osteoarthritis. They can evaluate your specific condition and provide appropriate guidance on dosage and potential side effects. Additionally, they may recommend a combination of medications or other treatment options to help alleviate knee pain and improve your quality of life.
Benefits and Risks of Medications for Knee Osteoarthritis
“Medications for knee osteoarthritis provide pain relief and help manage symptoms. However, it is important to understand the potential benefits and risks associated with these medications.”
While medications can offer significant benefits in managing knee osteoarthritis, it is essential to be aware of the potential risks and side effects. Some common side effects of NSAIDs include stomach upset, heartburn, and an increased risk of gastrointestinal bleeding. Acetaminophen, when used in excessive doses, can cause liver damage. Prescription NSAIDs and duloxetine may have additional side effects that should be discussed with a healthcare professional.
It is crucial to follow the recommended dosage and usage instructions provided by your healthcare professional or as indicated on the medication packaging. If you experience any unexpected or severe side effects, it is important to seek immediate medical attention.
| Medication | Benefits | Side Effects |
|---|---|---|
| Over-the-counter NSAIDs (ibuprofen, naproxen) | – Reduces pain, swelling, and stiffness – Easily accessible without a prescription |
– Stomach upset – Heartburn – Increased risk of gastrointestinal bleeding |
| Acetaminophen | – Provides pain relief – Recommended as first-line treatment |
– Risk of liver damage with excessive doses |
| Prescription NSAIDs (meloxicam, diclofenac) | – Higher potency for pain relief – May be necessary for severe pain |
– Similar side effects to over-the-counter NSAIDs |
| Duloxetine | – Reduces pain and may help with depression symptoms | – Potential side effects include nausea, dizziness, and fatigue |
Injections for Knee Osteoarthritis
When it comes to finding effective relief for knee osteoarthritis, injections can be a valuable treatment option. These injections are especially beneficial if other approaches haven’t provided sufficient pain relief. There are two main types of injections commonly used for knee osteoarthritis: corticosteroid injections and hyaluronic acid injections.
Corticosteroid Injections: These injections contain a powerful anti-inflammatory medication called corticosteroids. When injected directly into the knee joint, corticosteroids can effectively reduce inflammation, pain, and swelling. This provides long-lasting relief to individuals suffering from knee osteoarthritis. Corticosteroid injections may be recommended as an alternative to surgery or used along with other treatments to manage the symptoms.
Hyaluronic Acid Injections: Hyaluronic acid injections aim to provide lubrication to the knee joint. As knee osteoarthritis progresses, the natural production of hyaluronic acid diminishes, leading to increased friction and pain in the joint. By injecting hyaluronic acid into the knee, these injections can improve mobility, reduce pain, and enhance joint function. Hyaluronic acid injections can be a valuable treatment option, particularly for individuals looking to avoid or delay surgical intervention.
It’s crucial to have an open discussion with a healthcare professional to evaluate the potential benefits and risks of injections for your specific condition. They can provide guidance on which type of injection is most suitable and outline a comprehensive treatment plan tailored to your needs.

Comparing Corticosteroid and Hyaluronic Acid Injections:
| Feature | Corticosteroid Injections | Hyaluronic Acid Injections |
|---|---|---|
| Pain relief | Provide immediate pain relief that can last for several weeks or months. | May take multiple injections over several weeks to achieve optimal pain relief. |
| Mechanism of action | Reduces inflammation in the joint | Provides lubrication to the knee joint |
| Treatment frequency | Can be administered every 3 to 4 months, depending on the individual’s response | Usually requires a series of injections over several weeks |
| Side effects | Potential side effects include a temporary increase in pain, infection, and thinning of nearby bones and tissues. | Possible side effects include local irritation, swelling, and bruising at the injection site. |
As with any medical procedure, injections for knee osteoarthritis should be discussed thoroughly with a healthcare professional to ensure the best possible outcome and minimize the risk of complications.
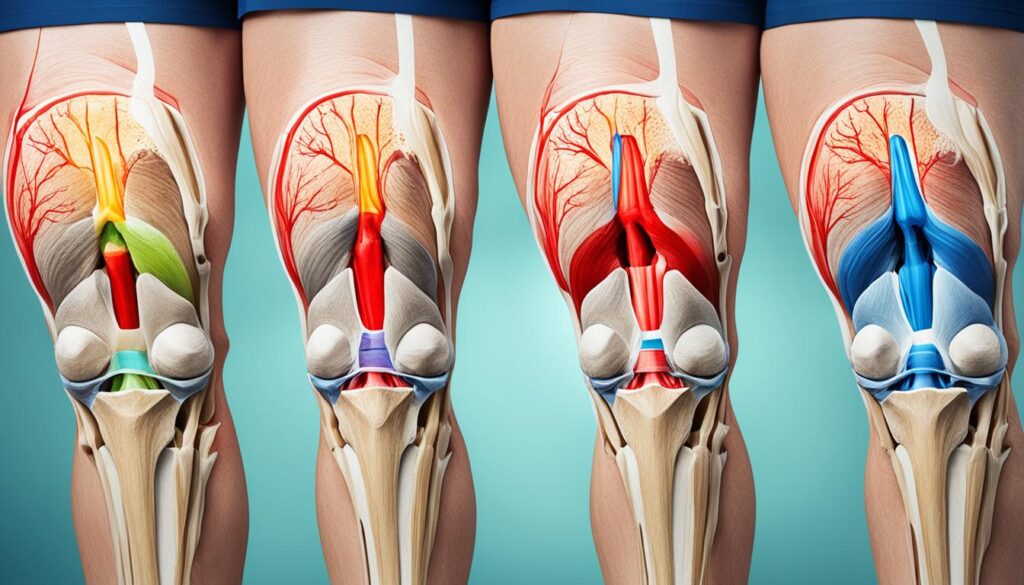
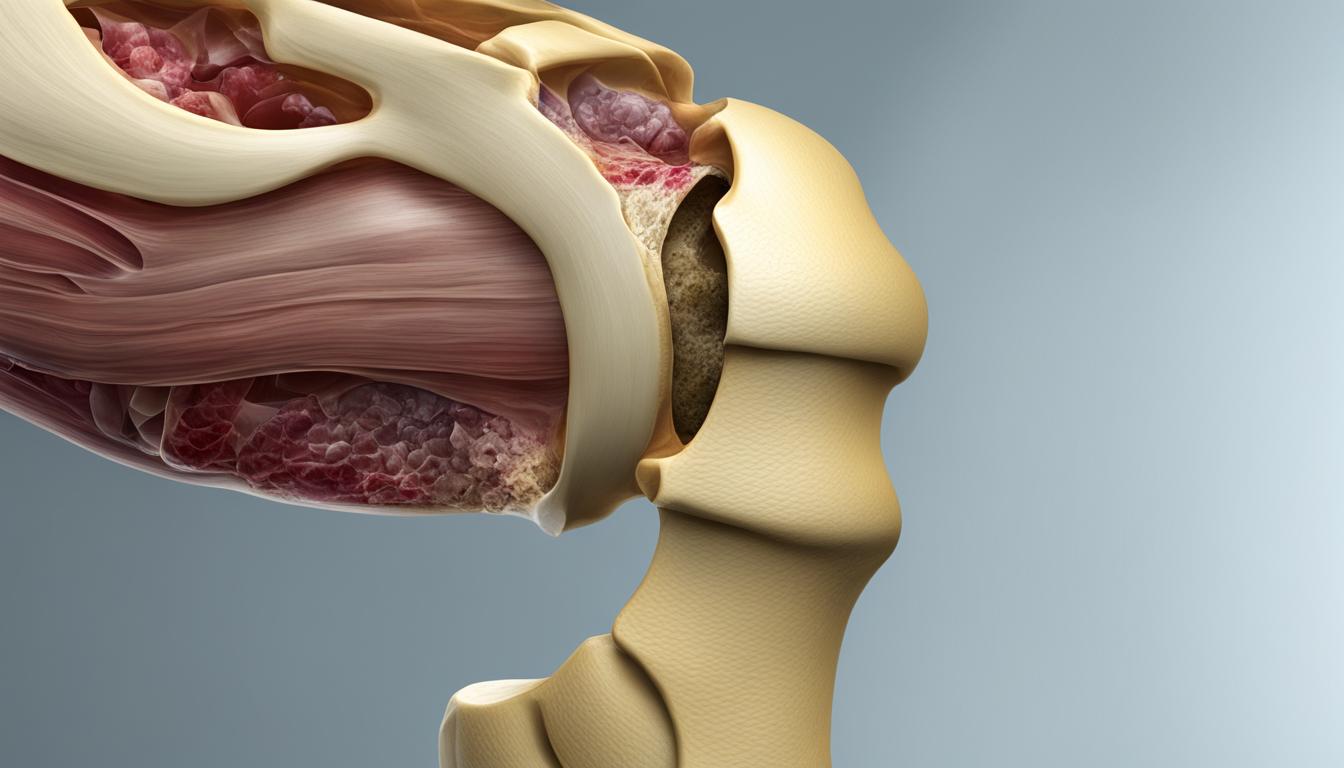
Surgical Treatment for Knee Osteoarthritis
In cases where conservative treatments have not provided sufficient pain relief or joint function improvement, surgical intervention may be necessary. Knee replacement surgery, also known as arthroplasty, is the most effective treatment for permanent pain relief in severe cases of knee osteoarthritis. During this surgical procedure, the damaged joint surfaces are replaced with artificial components made of metal and plastic. Other surgical options, such as arthroscopy to repair cartilage or meniscus tears, or osteotomy to realign bones, may be considered depending on the individual’s specific condition. Surgical treatments should be discussed thoroughly with a healthcare professional to determine the most appropriate approach.
| Surgical Treatment Options | Description |
|---|---|
| Knee Replacement Surgery (Arthroplasty) | Replacement of damaged joint surfaces with artificial components to provide permanent pain relief and improved joint function. |
| Arthroscopy | A minimally invasive surgical procedure that uses a tiny camera to repair cartilage or meniscus tears in the knee joint. |
| Osteotomy | A procedure that involves cutting and realigning bones to relieve pressure on the damaged knee joint and improve overall function. |
Alternative Therapies for Knee Osteoarthritis
Complementary and alternative medicine (CAM) therapies have gained popularity in the treatment of knee osteoarthritis. These therapies provide additional options for individuals seeking alternative approaches to traditional treatments. Although research on their effectiveness is ongoing, many people find relief and improved joint function through these alternative therapies.
Acupuncture
One widely practiced alternative therapy for knee osteoarthritis is acupuncture. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the body’s natural healing processes. It is believed to help reduce pain and inflammation associated with knee osteoarthritis. Although the exact mechanisms of its effect are not fully understood, many individuals report positive results from this ancient practice.
Glucosamine and Chondroitin Supplements
Glucosamine and chondroitin sulfate are commonly used supplements for knee osteoarthritis. These supplements are marketed as disease-modifying options, aiming to slow down the progression of joint damage and reduce pain. While some studies suggest that they can provide relief, the evidence is mixed, and their effectiveness may vary from person to person. Patients should consult with a healthcare professional before starting any supplement regimen.
Avocado-Soybean Unsaponifiables
Avocado-soybean unsaponifiables (ASU) is a natural extract derived from avocado and soybean oils. It has been used in Europe as an alternative therapy for knee and hip osteoarthritis. ASU is believed to help slow down or prevent joint damage by reducing inflammation and promoting cartilage repair. While more research is needed to fully understand its effectiveness, some individuals have reported positive outcomes from using ASU as part of their knee osteoarthritis treatment plan.
| Alternative Therapy | Description | Evidence of Effectiveness |
|---|---|---|
| Acupuncture | Insertion of thin needles into specific points on the body to stimulate healing processes | Some individuals report pain relief and improved joint function |
| Glucosamine and Chondroitin Supplements | Supplements marketed as disease-modifying options to slow down joint damage | Evidence of effectiveness is mixed; efficacy varies from person to person |
| Avocado-Soybean Unsaponifiables | Extract derived from avocado and soybean oils to reduce inflammation and promote cartilage repair | Some individuals experience reduced joint damage and improved symptoms |
It is important to note that alternative therapies should be used in conjunction with mainstream medical treatments and under the guidance of a healthcare professional. While these therapies may provide benefits for some individuals, they may not be suitable for everyone. It’s essential to have an open and honest conversation with your healthcare provider to discuss the potential benefits and risks of alternative therapies in your specific case.
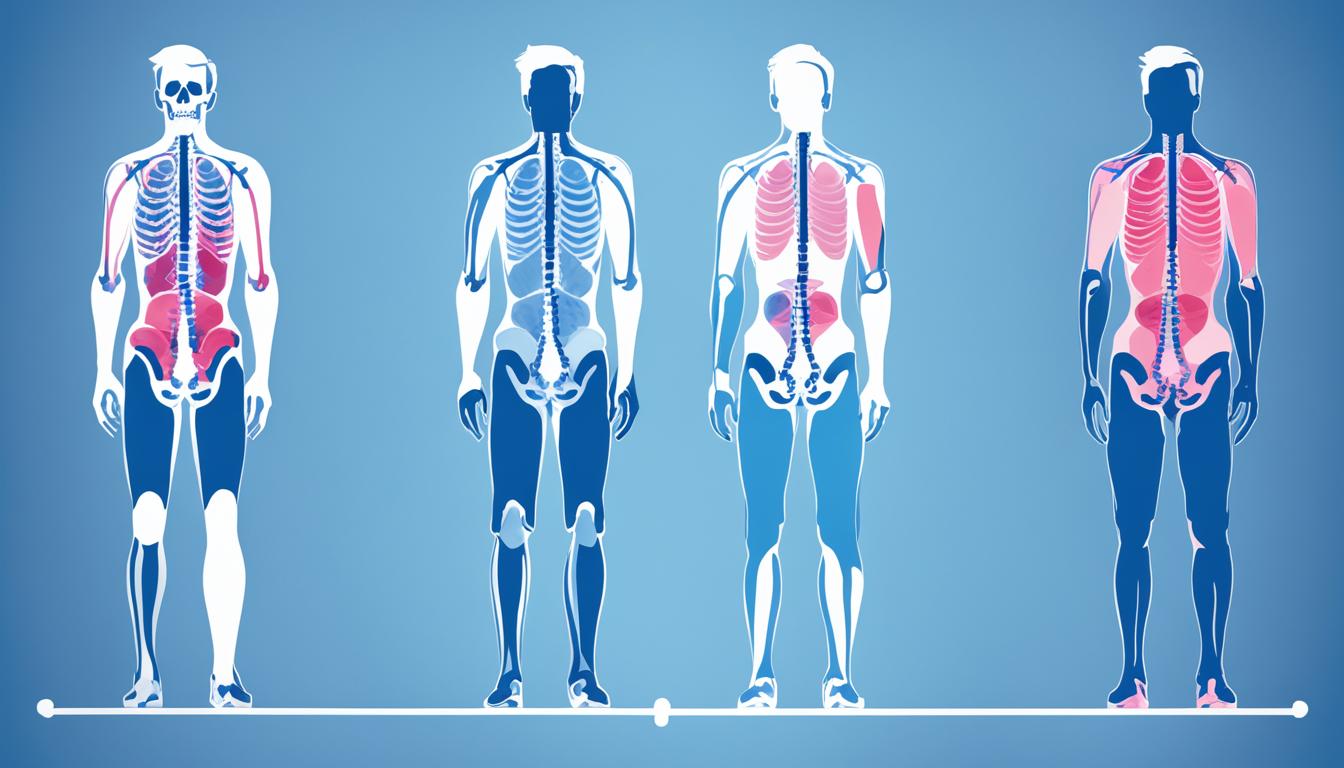
Diagnosis and Evaluation of Knee Osteoarthritis
The diagnosis of knee osteoarthritis involves a comprehensive evaluation that combines clinical examination and diagnostic tests. Healthcare professionals use these methods to assess the severity of symptoms and develop an accurate diagnosis. Physical examination, medical history, imaging tests, and joint fluid analysis are key components of the diagnostic process.
Physical Examination
A thorough physical examination is an essential part of diagnosing knee osteoarthritis. During the examination, the healthcare professional will assess the affected joint for tenderness, swelling, redness, and flexibility. These observations provide important clues about the presence and extent of joint damage. By evaluating the range of motion and joint stability, the healthcare professional can better understand the impact of the condition on daily activities.
Medical History
Obtaining a detailed medical history is crucial for diagnosing knee osteoarthritis. Healthcare professionals will ask about the duration and progression of symptoms, as well as any previous injuries or conditions that may have contributed to the development of osteoarthritis. Understanding the patient’s medical history helps determine the underlying causes and risk factors associated with the condition, enabling an accurate diagnosis.
Imaging Tests
Imaging tests play a vital role in diagnosing knee osteoarthritis by providing visual evidence of joint damage and ruling out other conditions. X-rays are commonly used to assess the extent of joint degeneration, the presence of bone spurs, and joint space narrowing. Magnetic resonance imaging (MRI) may be requested in more complex cases to evaluate the soft tissues, cartilage, and ligaments surrounding the knee joint.
By analyzing the images obtained from X-rays and MRI scans, healthcare professionals can determine the severity of knee osteoarthritis and devise suitable treatment plans. These tests also help rule out other potential causes of joint pain, such as fractures, tumors, or infections.
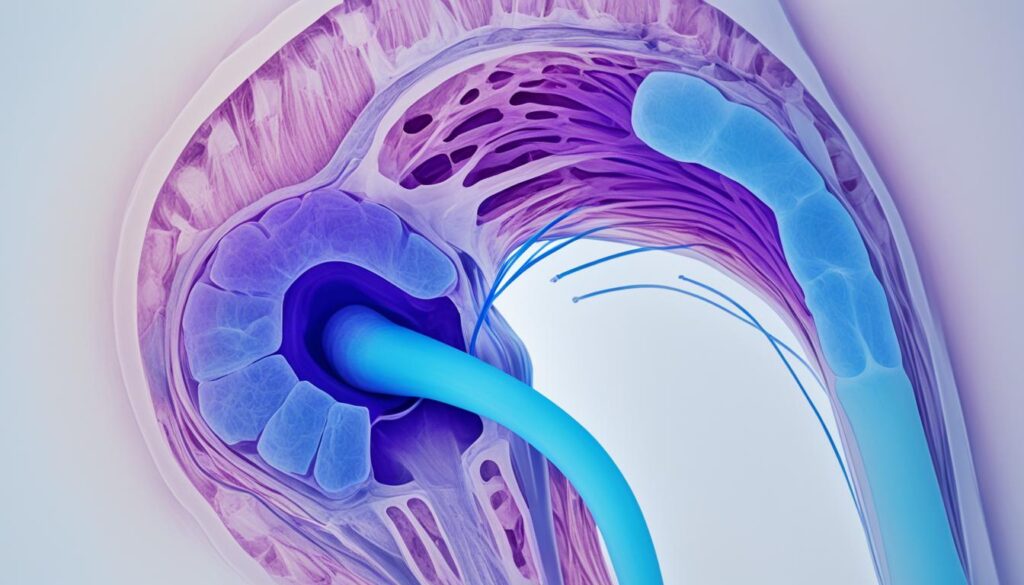
Joint Fluid Analysis
Joint fluid analysis, also known as arthrocentesis, involves withdrawing fluid from the affected joint to confirm the diagnosis of knee osteoarthritis and rule out other causes of joint pain. The fluid is then examined in a laboratory to assess its color, viscosity, and cell count. Healthcare professionals look for specific markers associated with osteoarthritis, such as high levels of inflammatory markers or crystals.
Joint fluid analysis helps differentiate knee osteoarthritis from other conditions, such as gout or infection. It provides valuable information about the inflammatory processes occurring within the joint, aiding in the development of an accurate diagnosis and treatment plan.
To ensure a comprehensive evaluation and accurate diagnosis of knee osteoarthritis, it is crucial to consult with a healthcare professional. They will utilize physical examination, medical history, imaging tests, and joint fluid analysis to develop an individualized approach that addresses your specific needs and symptoms.
| Diagnostic Method | Purpose | Advantages | Disadvantages |
|---|---|---|---|
| Physical Examination | Evaluate tenderness, swelling, redness, and flexibility of the affected joint | Non-invasive, provides immediate information about joint status | Subjective assessment, cannot provide detailed visualization of internal joint structures |
| Medical History | Collect information about symptom duration, progression, and contributing factors | Identify underlying causes and risk factors | Relies on patient’s recollection and may not capture all relevant details |
| Imaging Tests (X-rays) | Evaluate joint degeneration, bone spurs, and joint space narrowing | Provide visual evidence of joint damage and help determine severity | Limited assessment of soft tissues and cartilage |
| Imaging Tests (MRI) | Evaluate soft tissues, cartilage, and ligaments | Detailed visualization of joint structures | Expensive, may not be necessary in all cases |
| Joint Fluid Analysis | Confirm diagnosis, rule out other causes of joint pain | Direct examination of joint fluid for markers of osteoarthritis | Invasive, risk of infection or bleeding |
Conclusion
Knee osteoarthritis is a common condition that can significantly impact one’s daily life. However, there are several effective treatment options available to help manage the symptoms and improve joint function. From physical therapy and medications to injections, surgery, and alternative therapies, there is a range of approaches to consider.
The choice of treatment depends on various factors such as the severity of the symptoms, individual preferences, and overall health. It is crucial to consult with a healthcare professional who can assess your specific situation and develop a personalized treatment plan tailored to your needs and goals for managing knee osteoarthritis.
By working closely with a healthcare professional, you can explore the different treatment options available and determine the most suitable approach to address your knee osteoarthritis. Remember, managing this condition is a collaborative effort, and together, we can find the most effective ways to alleviate pain, improve function, and enhance your overall quality of life.
FAQ
What are the treatment options for knee osteoarthritis?
The treatment options for knee osteoarthritis include physical therapy, medications, injections, surgery, and alternative therapies.
How does physical therapy help in managing knee osteoarthritis?
Physical therapy for knee osteoarthritis involves exercises and techniques that aim to strengthen the muscles supporting the knee, increase flexibility, and reduce pain.
What medications are used for knee osteoarthritis?
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen can provide pain relief and help manage symptoms of knee osteoarthritis.
What role do injections play in treating knee osteoarthritis?
Injections, such as corticosteroid injections and hyaluronic acid injections, can provide pain relief and reduce inflammation in the knee joint for individuals with knee osteoarthritis.
What are the surgical options for knee osteoarthritis?
Surgical treatment options for knee osteoarthritis include knee replacement surgery, arthroscopy, and osteotomy depending on the severity of the condition.
Can alternative therapies be effective in managing knee osteoarthritis?
Complementary and alternative medicine therapies, such as acupuncture, glucosamine and chondroitin supplements, and avocado-soybean unsaponifiables, have shown promise in reducing pain and improving joint function in knee osteoarthritis.
How is knee osteoarthritis diagnosed?
The diagnosis of knee osteoarthritis is based on a combination of clinical evaluation, including physical examination and medical history, and diagnostic tests such as X-rays, MRI, and joint fluid analysis.
What should I do to manage knee osteoarthritis?
It is important to work with a healthcare professional to develop a personalized treatment plan that addresses your specific needs and goals for managing knee osteoarthritis.