Knee ligaments are the unsung heroes of mobility, acting as strong fibrous connective tissues that bind bones together and provide crucial stability to your knee joint. When these ligaments weaken or become injured, everyday movements can become painful challenges. Fortunately, there are natural, non-invasive ways to strengthen these vital structures. This guide explores science-backed methods to strengthen knee ligaments naturally, helping you maintain mobility and prevent injuries without resorting to surgery or medications.
Understanding Knee Ligaments and Their Function
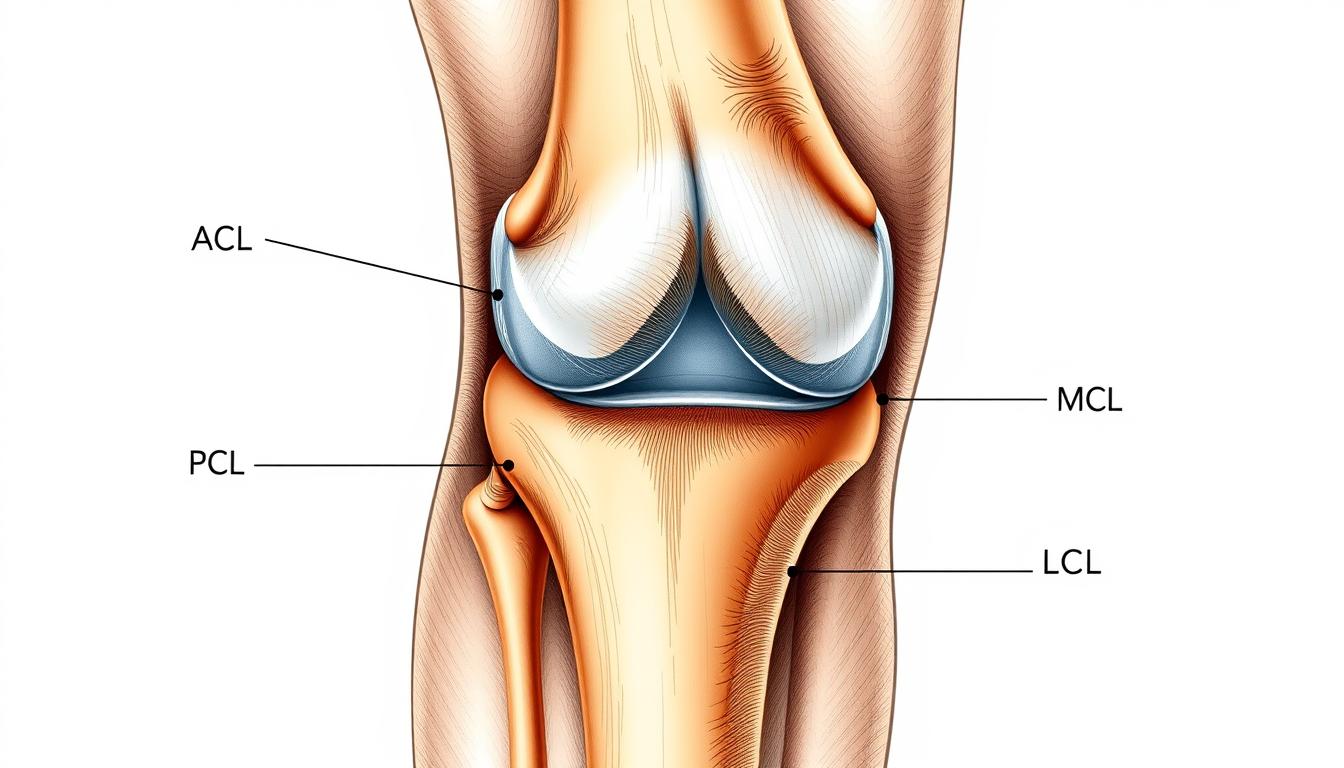
Think of knee ligaments as nature’s stabilizing cables. Your knee has four main ligaments: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). Each plays a specific role in keeping your knee stable during different movements. When these ligaments are strong and healthy, they allow for smooth, pain-free motion while preventing excessive movement that could damage the joint.
Unlike muscles, ligaments have limited blood supply, which means they heal slowly after injury. This makes prevention and natural strengthening particularly important. By focusing on natural methods to strengthen knee ligaments, you can avoid the lengthy recovery times associated with ligament injuries and the potential complications of surgical interventions.
Targeted Exercises to Strengthen Knee Ligaments
The foundation of natural knee ligament strengthening lies in specific exercises that build the supporting muscles around the knee. Strong muscles take pressure off ligaments, providing better joint stability and reducing injury risk. Here are effective, low-impact exercises that research has shown to strengthen the knee complex:
1. Leg Lifts for Quadriceps Strength
- Lie flat on your back on a comfortable surface.
- Keep one leg straight and bend the other slightly at the knee.
- Engage your core by pulling your belly button toward your spine.
- Slowly lift the straight leg about 12 inches off the floor without bending the knee.
- Hold for 5 seconds, then slowly lower.
- Complete 3 sets of 10 repetitions for each leg.
This exercise strengthens the quadriceps, which are crucial for knee stability. A 2019 study in the Journal of Exercise Rehabilitation found that straight leg raises significantly improved knee function in patients with knee osteoarthritis.
2. Standing Hamstring Curls

- Stand straight with feet hip-width apart, holding onto a chair or wall for balance.
- Slowly bend one knee, bringing your heel toward your buttocks.
- Keep your thighs aligned and knees close together.
- Hold for 5 seconds at the top of the movement.
- Lower slowly and repeat 10 times before switching legs.
- Complete 3 sets for each leg.
This exercise targets the hamstrings, which work in tandem with the ACL to prevent forward sliding of the tibia (shin bone). Research published in the American Journal of Sports Medicine indicates that balanced hamstring-to-quadriceps strength ratios reduce ACL injury risk.
3. Wall Squats for Overall Knee Stability

- Stand with your back against a wall, feet about 24 inches away from the wall.
- Slowly slide your back down until your knees are bent at approximately 90 degrees.
- Ensure your knees don’t extend past your toes.
- Hold this position for 5-10 seconds.
- Slowly slide back up to the starting position.
- Repeat 10 times for 2-3 sets.
Wall squats build strength in multiple muscle groups that support the knee joint. A controlled environment reduces the risk of improper form that could stress ligaments.
4. Resistance Band Exercises

Resistance bands provide an excellent way to strengthen the muscles around the knee without putting excessive stress on the joint. The “monster walk” is particularly effective:
- Place a resistance band just above your ankles or knees.
- Stand with feet hip-width apart, knees slightly bent.
- Step sideways while maintaining tension in the band.
- Take 10-15 steps in one direction, then reverse.
- Complete 3 sets in each direction.
A study in the Journal of Physical Therapy Science found that resistance band exercises significantly improved knee stability in patients with mild knee osteoarthritis by strengthening the hip abductors that support proper knee alignment.
Nutrition for Ligament Health

What you eat plays a crucial role in maintaining and strengthening knee ligaments. Certain nutrients are particularly important for ligament health:
Collagen-Rich Foods
Ligaments are primarily made of collagen, so consuming collagen-rich foods can help provide the building blocks needed for repair and strengthening. Include these in your diet:
- Bone broth (simmered for at least 12 hours to extract collagen)
- Chicken skin and cartilage
- Fish with edible bones (sardines, salmon)
- Pork or beef tendon
Vitamin C for Collagen Synthesis
Vitamin C is essential for collagen production. Without adequate vitamin C, your body cannot effectively create new collagen. Research published in the Journal of Biological Chemistry confirms vitamin C’s critical role in collagen synthesis. Include these vitamin C-rich foods:
- Citrus fruits (oranges, grapefruits, lemons)
- Bell peppers
- Strawberries
- Kiwi
- Broccoli
Omega-3 Fatty Acids for Inflammation Control
Omega-3 fatty acids help reduce inflammation that can damage ligaments over time. A study in the Journal of the American College of Nutrition found that omega-3 supplementation reduced joint pain and increased grip strength in patients with rheumatoid arthritis. Good sources include:
- Fatty fish (salmon, mackerel, sardines)
- Walnuts
- Flaxseeds and chia seeds
- Algal oil (plant-based option)
Hydration for Ligament Function
Water makes up about 70% of ligament tissue. Dehydration can make ligaments less elastic and more prone to injury. Aim to drink at least 8 glasses of water daily, more if you’re active or in hot weather. A study in the Journal of Athletic Training found that even mild dehydration negatively affected joint proprioception, potentially increasing injury risk.
Lifestyle Adjustments for Stronger Knee Ligaments

Weight Management
Excess weight places additional stress on knee ligaments. Research published in Arthritis & Rheumatism found that for every pound of weight loss, there is a four-pound reduction in knee joint load. Maintaining a healthy weight through balanced nutrition and regular exercise significantly reduces strain on knee ligaments.
Proper Posture and Alignment
Poor posture doesn’t just affect your back—it changes how weight is distributed through your knees. Practice these alignment principles:
- Keep knees in line with toes when squatting or climbing stairs
- Avoid sitting with legs crossed for extended periods
- Use proper form during all exercises
- Consider consulting with a physical therapist for personalized posture correction
Appropriate Footwear
Shoes with proper support help maintain correct knee alignment. A study in the Journal of Foot and Ankle Research found that appropriate footwear can reduce knee adduction moment, a key factor in knee osteoarthritis progression. Look for shoes with:
- Good arch support
- Cushioning for shock absorption
- Proper fit (not too tight or too loose)
- Replacement every 300-500 miles if used for running
Avoiding High-Risk Activities
While staying active is important, certain activities place excessive stress on knee ligaments. Consider limiting or modifying:
- Deep squats with heavy weights
- High-impact activities on hard surfaces
- Sudden direction changes in sports without proper training
- Excessive downhill running
Instead, incorporate low-impact activities like swimming, cycling, or elliptical training that strengthen muscles without stressing ligaments.
Natural Supplements for Ligament Support

Certain supplements may help strengthen knee ligaments naturally. Always consult with a healthcare provider before starting any supplement regimen, especially if you have existing health conditions or take medications.
Turmeric (Curcumin)
Turmeric contains curcumin, a compound with powerful anti-inflammatory properties. A 2016 systematic review published in the Journal of Medicinal Food found that turmeric extract was as effective as ibuprofen for knee osteoarthritis pain. Typical dosage: 500-1000mg of curcumin daily, preferably with black pepper extract (piperine) to enhance absorption.
Ginger
Like turmeric, ginger has anti-inflammatory properties that may help reduce knee pain and improve function. Research in Arthritis & Rheumatism showed that ginger extract reduced pain and stiffness in people with osteoarthritis. Typical dosage: 250-500mg, 2-3 times daily.
Glucosamine and Chondroitin
These compounds are natural components of cartilage. While research results are mixed, some studies suggest they may help maintain joint health and reduce pain, particularly when taken together. A large-scale study called GAIT (Glucosamine/Chondroitin Arthritis Intervention Trial) found that the combination helped people with moderate-to-severe knee pain. Typical dosage: 1500mg glucosamine and 1200mg chondroitin daily.
Collagen Supplements
Hydrolyzed collagen supplements may support ligament health. A 2017 review in the Journal of Sports Science & Medicine found that collagen peptide supplementation improved joint pain and function in athletes. Typical dosage: 10-15g daily.
Important: Supplements are not regulated as strictly as medications. Choose products from reputable manufacturers, and always discuss supplement use with your healthcare provider, especially if you have existing health conditions or take medications.
Precautions and When to Seek Professional Help

While natural methods can be effective for strengthening knee ligaments, it’s important to approach them with caution and know when professional help is needed.
Warning Signs That Require Medical Attention
- Sudden, severe pain following an injury
- Audible popping sound at the time of injury
- Inability to bear weight on the affected leg
- Visible deformity or significant swelling
- Joint instability or feeling that the knee “gives way”
- Pain that persists or worsens despite rest and home treatment
Avoiding Overexertion
When strengthening knee ligaments, more is not always better. Overexertion can lead to injury or worsen existing conditions. Follow these guidelines:
- Start with low intensity and gradually increase
- Allow 48 hours of recovery between strength training sessions for the same muscle groups
- Listen to your body—pain beyond mild muscle soreness is a warning sign
- Modify exercises if they cause pain
The Value of Professional Guidance
A physical therapist or sports medicine specialist can provide:
- Personalized exercise programs based on your specific needs
- Proper technique instruction to maximize benefits and prevent injury
- Progressive advancement of exercises as your strength improves
- Complementary treatments like manual therapy or taping techniques
Get Personalized Knee Strengthening Guidance
For a customized program tailored to your specific knee condition, consider consulting with a physical therapist who specializes in knee rehabilitation.
Implementation Plan: Putting It All Together
Creating a sustainable routine is key to strengthening knee ligaments naturally. Here’s a sample 8-week plan that incorporates all the elements discussed:
Weeks 1-2: Foundation Building
- Exercise: 2-3 days per week of basic exercises (leg lifts, wall sits) with low repetitions
- Nutrition: Begin incorporating collagen-rich foods and increase water intake
- Lifestyle: Assess and correct posture during daily activities
Weeks 3-4: Progressive Development
- Exercise: Increase to 3-4 days per week, add resistance band exercises
- Nutrition: Add vitamin C-rich foods to enhance collagen synthesis
- Supplements: Consider introducing one supplement (after consulting healthcare provider)
Weeks 5-6: Advancing Strength
- Exercise: Increase repetitions and sets, add more challenging variations
- Nutrition: Ensure balanced intake of all supportive nutrients
- Lifestyle: Implement proper footwear and activity modifications
Weeks 7-8: Maintenance and Progress
- Exercise: Full program 3-4 days per week with appropriate progression
- Evaluation: Assess improvements in pain, stability, and function
- Adjustment: Modify program based on progress and challenges
“Consistency, not intensity, is the key to strengthening knee ligaments naturally. Small, regular efforts yield greater results than occasional intense sessions.”
Conclusion: The Path to Stronger Knee Ligaments
Strengthening knee ligaments naturally is a journey that combines targeted exercises, proper nutrition, lifestyle adjustments, and potentially beneficial supplements. By taking a comprehensive approach, you can improve knee stability, reduce pain, and enhance your overall quality of life without resorting to invasive procedures.
Remember that natural strengthening takes time—ligaments respond slowly to interventions due to their limited blood supply. Be patient with your progress and consistent with your efforts. Small improvements add up to significant changes over time.
Most importantly, listen to your body throughout this process. Pain is a signal that something isn’t right. If you experience persistent or worsening pain, consult with a healthcare professional for personalized guidance.
By implementing the science-backed methods outlined in this guide, you’re taking an important step toward healthier, stronger knee ligaments that will support your mobility and active lifestyle for years to come.
Ready to Start Your Knee Strengthening Journey?
Download our free printable exercise guide with detailed instructions and progress tracking tools.
Frequently Asked Questions
How long does it take to strengthen knee ligaments naturally?
Ligaments respond more slowly than muscles due to their limited blood supply. Most people begin to notice improvements in knee stability and reduced pain after 6-8 weeks of consistent exercise and proper nutrition. However, significant strengthening may take 3-6 months of dedicated effort. Individual results vary based on age, overall health, and the current condition of your ligaments.
Can damaged knee ligaments heal completely without surgery?
Minor ligament sprains (Grade I and some Grade II injuries) can often heal without surgery through proper rest, rehabilitation exercises, and natural strengthening methods. However, complete tears (Grade III injuries) typically require surgical intervention. Always consult with a healthcare provider for proper diagnosis and treatment recommendations for ligament injuries.
Is it safe to strengthen knee ligaments naturally if I already have knee pain?
Mild to moderate knee pain can often improve with appropriate strengthening exercises. However, you should first get a proper diagnosis from a healthcare provider to understand the cause of your pain. They can recommend specific exercises that are safe for your condition. Never push through sharp or increasing pain during exercises, as this could indicate you’re causing further damage.