Welcome to our article on knee osteoarthritis and the various sensations associated with this condition. Knee osteoarthritis is a common form of arthritis that affects millions of people around the world. It occurs when the protective cartilage that cushions the ends of the bones in the knee joint wears down over time. This can lead to symptoms such as knee pain, joint inflammation, knee stiffness, knee swelling, knee grinding, knee crackling, knee weakness, knee instability, and knee discomfort.
These sensations can vary from person to person and may have a significant impact on daily activities and quality of life. In the following sections, we will explore the symptoms of knee osteoarthritis in detail, discuss the risk factors associated with this condition, delve into the diagnostic process, and explore the various treatment options available.
If you or someone you know is living with knee osteoarthritis, it’s crucial to understand the sensations associated with the condition and how they can be managed. By arming yourself with knowledge, you can take proactive steps to improve your comfort and overall well-being.
Understanding Knee Osteoarthritis Symptoms
When it comes to knee osteoarthritis, understanding the symptoms is crucial for effective management. The condition typically develops slowly and worsens over time, leading to various sensations that can significantly impact daily life. Let’s explore the common symptoms associated with knee osteoarthritis:
Pain
Knee pain is a hallmark symptom of knee osteoarthritis and can occur during or after movement. Individuals may experience pain while walking, climbing stairs, or even at rest. The severity of the pain can vary, ranging from mild discomfort to more intense sensations.
Joint Stiffness
Joint stiffness is another prevalent symptom, often most noticeable upon awakening or after being inactive for a prolonged period. People with knee osteoarthritis may find it challenging to bend or straighten the affected knee, leading to limitations in mobility.
Tenderness
Knee osteoarthritis can cause tenderness in the joint when pressure is applied. The affected area may feel sensitive and painful to touch, further exacerbating discomfort.
Loss of Flexibility and Range of Motion
As knee osteoarthritis progresses, individuals may experience a loss of flexibility and range of motion in the affected knee. This limitation can hinder basic movements, such as squatting or kneeling, making everyday activities more challenging.
Grating Sensation or Crackling Noise
One characteristic symptom is a grating sensation or crackling noise when using the knee joint. This sensation, often referred to as crepitus, can occur due to the roughening of cartilage or the formation of bone spurs around the affected joint.
Swelling
Soft tissue inflammation can lead to swelling in the knee affected by osteoarthritis. The accumulation of fluid in and around the joint can cause visible enlargement and contribute to discomfort.
Understanding these symptoms is vital for early detection and intervention. If you experience any of these sensations, it is essential to consult with a healthcare professional for an accurate diagnosis.
Through a combination of medical assessments, physical examinations, and imaging tests, healthcare providers can determine the most appropriate treatment plan for managing knee osteoarthritis.
Risk Factors for Knee Osteoarthritis
Several factors can increase the risk of developing knee osteoarthritis. It is important to understand these risk factors in order to take preventive measures and manage the condition more effectively.
Advancing Age
As individuals get older, the risk of developing knee osteoarthritis increases. Age-related changes in the cartilage and joint tissues can lead to wear and tear, making the knee more susceptible to osteoarthritis.
Gender
Women are more likely to develop knee osteoarthritis than men. Although the exact reasons for this gender difference are not fully understood, hormonal factors and differences in joint structure and mechanics may play a role.
Obesity
Obesity puts extra stress on the weight-bearing joints, including the knees. The increased load on the knees can accelerate the breakdown of the cartilage and contribute to the development of knee osteoarthritis.
Joint Injuries
Previous joint injuries, such as fractures or ligament tears, can increase the risk of developing knee osteoarthritis later in life. Damage to the joint structures can lead to abnormal wear and tear, causing osteoarthritis to develop.
Repetitive Stress
Repetitive stress on the knee joint, often due to certain occupations or sports activities, can contribute to the development of knee osteoarthritis. Activities that involve repetitive motions or prolonged periods of kneeling or squatting can increase the risk.
Genetics
Some individuals may inherit a predisposition to developing osteoarthritis. Certain genetic factors can influence the structure and function of the joints, making them more vulnerable to the degenerative changes associated with knee osteoarthritis.
Metabolic Diseases
Metabolic diseases, such as diabetes and hemochromatosis, are associated with an increased risk of developing knee osteoarthritis. These conditions can affect joint health and contribute to the degeneration of the cartilage in the knees.
By understanding and addressing these risk factors, individuals can take proactive steps to reduce their risk of developing knee osteoarthritis. Maintaining a healthy weight, avoiding repetitive stress on the knees, protecting the joints during physical activities, and managing underlying metabolic conditions can all play a role in preventing or managing knee osteoarthritis.
| Risk Factor | Description |
|---|---|
| Advancing Age | The risk increases as individuals get older. |
| Gender | Women are more likely to develop knee osteoarthritis. |
| Obesity | Excess weight puts extra stress on the knees. |
| Joint Injuries | Previous injuries can contribute to knee osteoarthritis. |
| Repetitive Stress | Jobs or activities that involve repetitive knee movements or prolonged kneeling/squatting increase the risk. |
| Genetics | Some individuals have a genetic predisposition to developing knee osteoarthritis. |
| Metabolic Diseases | Conditions like diabetes and hemochromatosis are associated with an increased risk. |
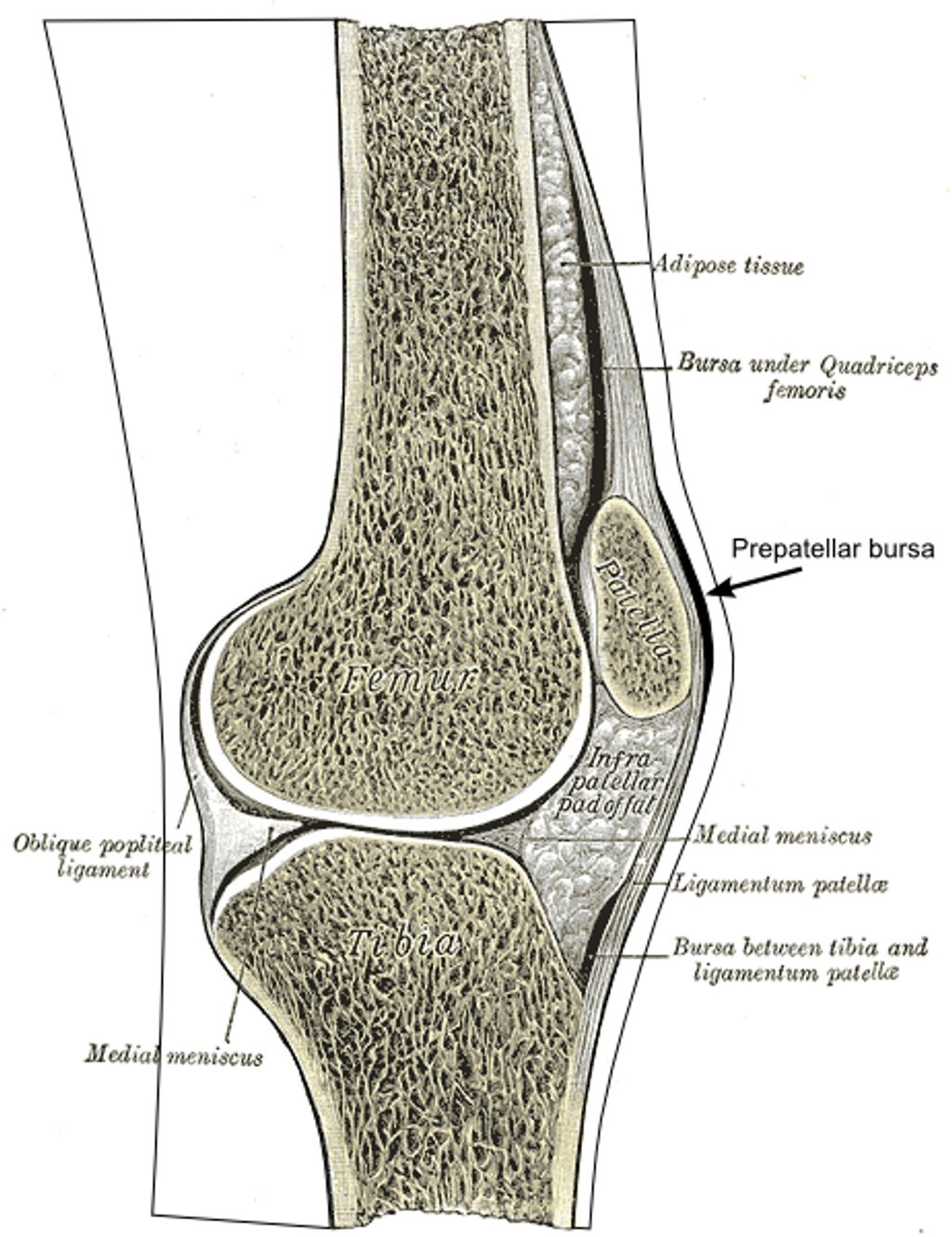
Diagnosing Knee Osteoarthritis
Diagnosing knee osteoarthritis involves a comprehensive evaluation of the patient’s medical history, a thorough physical examination, and the use of imaging tests. The goal is to gather relevant information that will aid in the accurate diagnosis and development of an appropriate treatment plan.
During the medical history evaluation, the healthcare provider will inquire about the patient’s symptoms, medical conditions, prior injuries, and medication use. This information helps establish a baseline understanding of the patient’s overall health and potential risk factors for knee osteoarthritis.
The next step is the physical examination, where the healthcare provider will assess various aspects of the knee joint. They will evaluate the range of motion, looking for signs of stiffness or limitations in movement. The provider will also check for joint tenderness, as well as any other indications of osteoarthritis, such as swelling or deformities.
To confirm the diagnosis and gather further insights, imaging tests are often employed. X-rays are commonly used to visualize joint and bone damage, such as narrowing of the joint space, the presence of bone spurs, or changes in bone density. This can provide valuable information about the severity and progression of knee osteoarthritis.
For a more detailed view of the knee joint structures, an MRI (Magnetic Resonance Imaging) scan may be recommended. MRI scans use powerful magnets and radio waves to generate detailed images of the cartilage, ligaments, tendons, and other soft tissues. This allows healthcare providers to assess the extent of cartilage damage and identify any associated structural abnormalities.
In some cases, joint aspiration may be performed to analyze the synovial fluid within the knee joint. This involves using a thin needle to remove a small sample of fluid, which can be examined for signs of infection or other conditions that may be contributing to symptoms.
A comprehensive diagnosis of knee osteoarthritis, based on medical history, physical examination, and imaging tests, enables healthcare providers to develop a tailored treatment plan that addresses the specific needs of the patient.
Treating Knee Osteoarthritis
While there is no cure for knee osteoarthritis, there are various treatment options available to help manage symptoms and improve quality of life:
- Medication:
- Non-drug therapies:
- Surgery:
Medications such as analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids can help relieve pain and inflammation.
Non-drug therapies such as exercise, weight loss, physical therapies like physical therapy, and the use of assistive devices can also be beneficial.
In severe cases, joint surgery may be considered, including joint fusion or replacement.
Medication for Knee Osteoarthritis
The use of medication is a common approach to managing knee osteoarthritis. Different types of medications can help alleviate pain and reduce inflammation in the affected joint.
“Medications such as analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids can provide relief from knee osteoarthritis symptoms.”
Analgesics are pain relievers that can be used to alleviate mild to moderate pain associated with knee osteoarthritis. NSAIDs, such as ibuprofen and naproxen, help reduce pain and inflammation in the joint. Corticosteroids, which can be given orally or injected into the joint, can also provide temporary relief from pain and inflammation.
Non-Drug Therapies for Knee Osteoarthritis
Non-drug therapies are an essential part of knee osteoarthritis management. These therapies focus on improving joint function, reducing pain, and maintaining or improving mobility.
“Exercise, weight loss, physical therapies like physical therapy, and assistive devices can be effective in managing knee osteoarthritis.”
Exercise, such as strength training and low-impact activities like swimming and cycling, can help improve joint flexibility, strengthen the surrounding muscles, and reduce pain. Weight loss can also alleviate pressure on the knee joint, resulting in decreased pain and improved function.
Physical therapies, including physical therapy sessions and targeted exercises, can help improve joint stability, reduce pain, and increase range of motion. The use of assistive devices, such as braces, orthotics, and canes, can provide support and improve mobility for individuals with knee osteoarthritis.
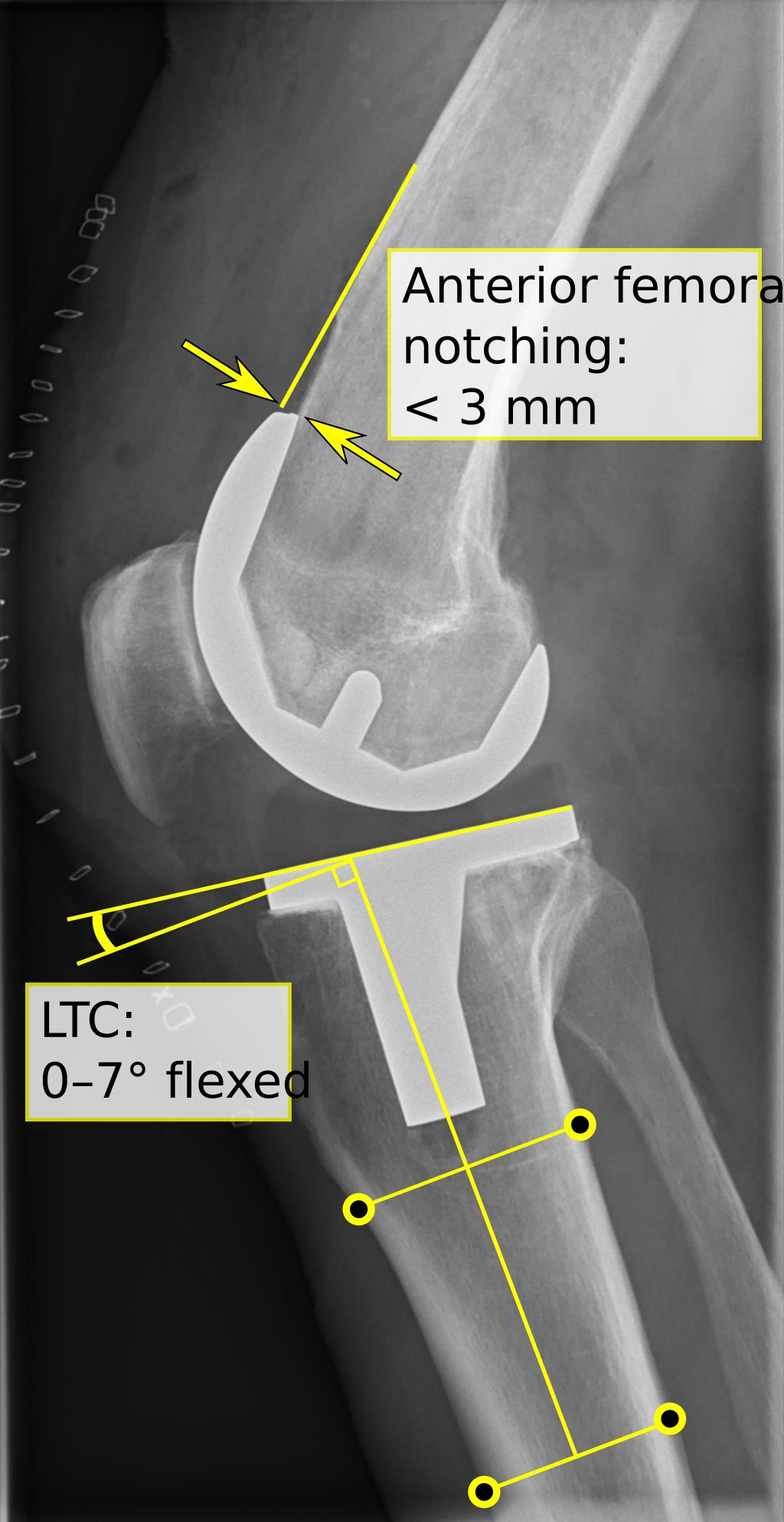
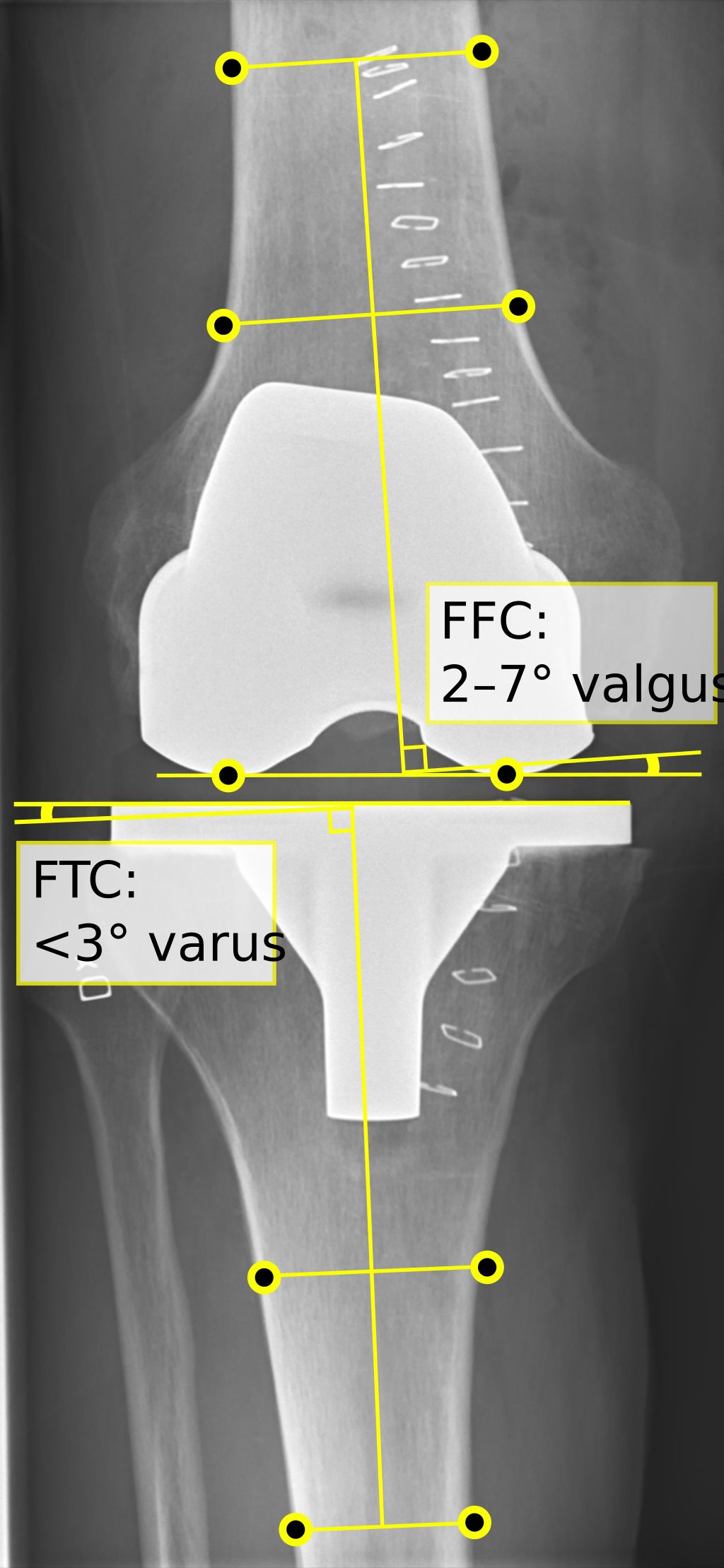
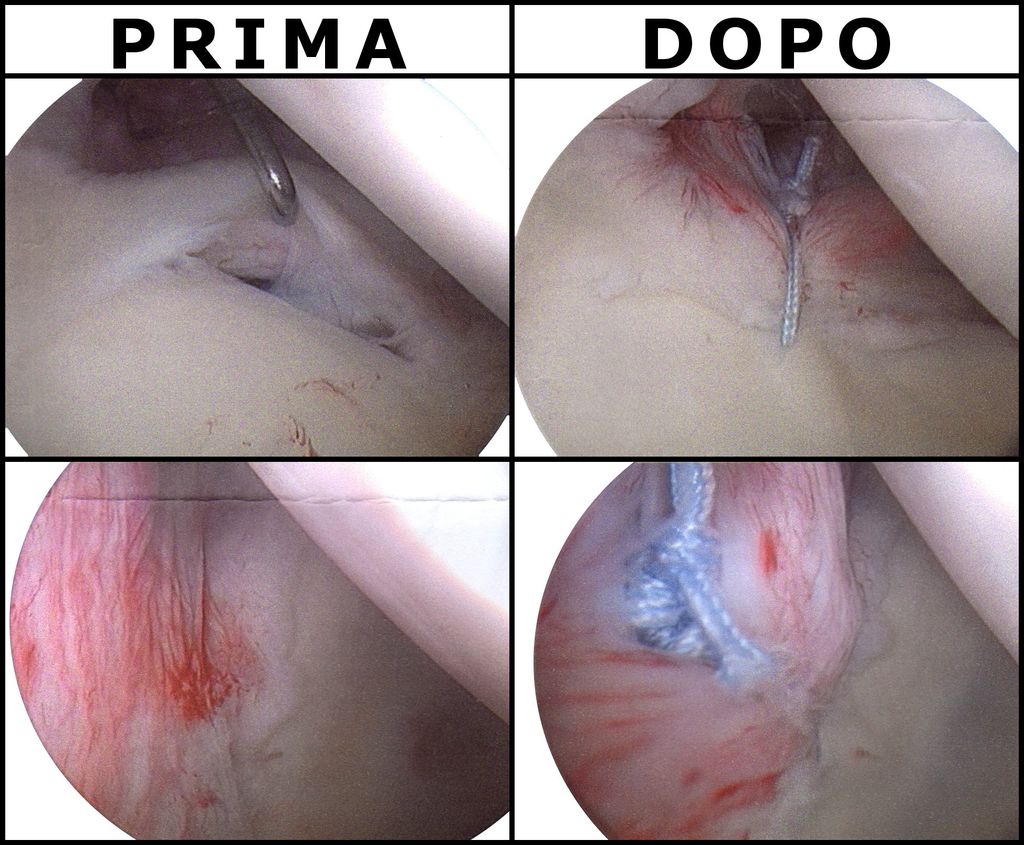
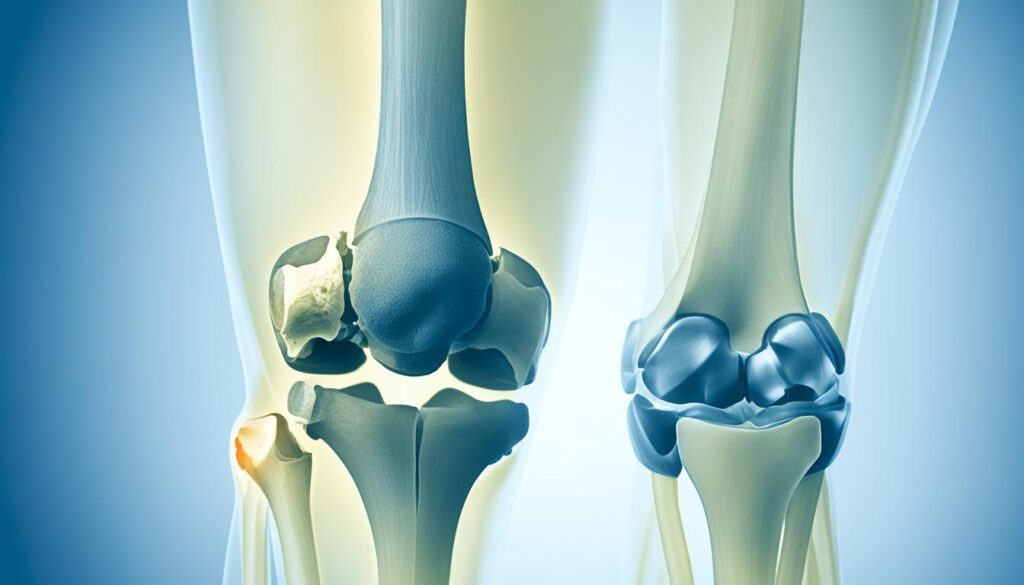
Surgery for Knee Osteoarthritis
In severe cases of knee osteoarthritis where non-drug therapies and medications are not providing sufficient relief, surgery may be considered as a treatment option.
“Joint surgery, including joint fusion or replacement, can be an effective solution for advanced knee osteoarthritis.”
Joint fusion involves permanently connecting the bones of the joint to reduce pain and improve stability. Joint replacement, such as total knee replacement, replaces the damaged joint surfaces with artificial parts, providing long-lasting pain relief and improved function.
It is important to note that the choice of treatment for knee osteoarthritis depends on various factors, including the severity of symptoms, individual preferences, and lifestyle. Consulting with a healthcare provider is crucial in determining the most appropriate treatment approach.
Conclusion
Knee osteoarthritis is a common condition that affects the joints, leading to pain, stiffness, and limited mobility. Although there is no cure for knee osteoarthritis, there are various treatment options available to manage symptoms and improve the quality of life for individuals affected by this condition.
It is crucial for individuals with knee osteoarthritis to work closely with their healthcare providers to develop a personalized management plan. This plan may include a combination of medication, non-drug therapies, and, in some cases, surgery. By effectively managing their condition, individuals can experience a reduction in pain, an increase in mobility, and an overall improvement in their quality of life.
Various treatment approaches can be employed to manage knee osteoarthritis, including the use of over-the-counter or prescription medications to alleviate pain and reduce inflammation. Non-drug therapies like exercise, weight loss, and physical therapies aim to strengthen the muscles surrounding the knee joint and improve joint stability. Assistive devices such as knee braces or walking aids may also be recommended to alleviate stress on the knee joint during daily activities.
In severe cases where other treatments have been ineffective, joint surgery, such as joint fusion or replacement, may be considered. These surgical procedures can help restore mobility and alleviate pain in individuals with advanced osteoarthritis.
FAQ
What are the common sensations associated with knee osteoarthritis?
Common sensations include knee pain, joint stiffness, tenderness, loss of flexibility, grating sensation, and swelling.
What factors increase the risk of developing knee osteoarthritis?
Risk factors for knee osteoarthritis include advancing age, being female, obesity, joint injuries, repetitive stress, genetics, and certain metabolic diseases.
How is knee osteoarthritis diagnosed?
Diagnosis of knee osteoarthritis typically involves a medical history evaluation, physical examination, and imaging tests such as X-rays and MRI. In some cases, joint aspiration may be performed.
What are the treatment options for knee osteoarthritis?
Treatment options for knee osteoarthritis include medications (analgesics, NSAIDs, corticosteroids), non-drug therapies (exercise, weight loss, physical therapy, assistive devices), and in severe cases, joint surgery.
Can knee osteoarthritis be cured?
There is no cure for knee osteoarthritis, but symptoms can be managed through various treatment options to improve quality of life.