Arthritis is a leading cause of pain and disability worldwide. At [Your Brand Name], we understand the challenges of managing osteoarthritis pain, especially when sitting for prolonged periods. That’s why we’ve compiled a list of effective strategies to help you reduce pain and discomfort and improve your overall quality of life.
When it comes to managing osteoarthritis pain while sitting, knowledge is power. Understanding your condition and its impact on joint health is crucial. This information empowers you to make informed decisions and seek appropriate support from healthcare professionals and loved ones.
In addition to gaining knowledge, there are several practical tips you can implement to alleviate osteoarthritis pain when sitting:
- Promote joint movement: Engage in gentle exercises and stretches specifically designed to maintain joint flexibility and reduce stiffness.
- Maintain good posture: Correct posture can help minimize the strain on your joints while sitting. Make sure to use ergonomic chairs or cushions that support your spine.
- Balance activity and rest: Find the right balance between staying active and allowing your joints to rest. Alternate between periods of physical activity and periods of rest to prevent excessive strain on your joints.
- Manage weight: Maintaining a healthy weight is essential for relieving pressure on your joints. Consistently following a balanced diet and engaging in regular exercise can help achieve and maintain a healthy weight.
- Quit smoking: Smoking has been linked to increased inflammation and a higher risk of developing arthritis. Quitting smoking can significantly improve your overall joint health and reduce osteoarthritis pain.
- Engage in appropriate exercises: Participating in low-impact exercises, such as swimming or bicycling, can help improve joint mobility and strengthen the surrounding muscles.
In addition to these lifestyle changes, various medications and therapies can provide relief from osteoarthritis pain when sitting. Consider discussing with your healthcare professional options such as cognitive-behavioral therapy, relaxation therapy, acupuncture, and heat/cold therapy that may suit your unique needs.
Remember, addressing both the physical and emotional aspects of pain is vital for effectively managing osteoarthritis pain when sitting. By implementing these strategies and seeking appropriate support, you can find relief and improve your comfort while sitting. Stay tuned for the next section of our article, where we will provide more tips for managing osteoarthritis pain when sitting.
Tips for Managing Osteoarthritis Pain When Sitting
When sitting for extended periods with osteoarthritis pain, it can be challenging to find relief. However, there are several strategies you can implement to alleviate discomfort and improve your sitting experience.
1. Regular Movement
One of the most effective ways to manage sitting-related osteoarthritis pain is to take regular breaks and move around. Aim to get up and walk around for at least five minutes every half hour. This helps to reduce stiffness, increase circulation, and relieve pressure on the joints.
2. Strengthening Exercises
Engaging in gentle exercises that target the muscles around painful joints can provide significant relief. Consult with a healthcare professional or physical therapist to develop an appropriate exercise routine. Strengthening the muscles can help support the joints and reduce discomfort while sitting.
3. Non-Impact Cardio Exercises
Cardio exercises that are low-impact, such as cycling or swimming, can help improve joint flexibility and reduce pain. These activities provide cardiovascular benefits without putting excessive strain on the joints. Incorporate these exercises into your routine to support overall joint health.
4. Mindful Physical Activity
When you have osteoarthritis pain, it’s essential to be mindful of physical activities that may worsen the pain. Avoid high-impact activities that put excessive stress on the joints, such as running or jumping. Instead, focus on exercises that are gentle on the joints, such as yoga or tai chi.
5. Over-the-Counter Medications and Topical Creams
In some cases, over-the-counter pain medications or topical creams can offer temporary relief from sitting-induced osteoarthritis pain. Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and alleviate discomfort. Topical creams containing capsaicin may also provide relief when applied to the affected area.
6. Heat and Cold Therapy
Applying heat or cold therapy to the affected joints can help relieve pain and reduce inflammation. Use a heating pad or warm towel to apply heat to the area. Alternatively, you can use ice packs or cold compresses for a numbing effect. Experiment with both heat and cold therapy to determine which works best for you.
7. Mobility Aids
If sitting-related osteoarthritis pain is severe, using mobility aids like canes or walkers can provide additional support and relieve pressure on the joints. Consult with a healthcare professional to determine if mobility aids are suitable for your condition.
8. Weight Management
Maintaining a healthy weight is crucial for managing osteoarthritis pain. Excess weight puts additional strain on the joints, leading to increased discomfort. Follow a balanced diet, engage in regular exercise, and consult with a healthcare professional for guidance on weight management.
9. Home Safety
Remove hazards in your home that could lead to falls or exacerbate your osteoarthritis pain. Ensure that walkways are clear, rugs are secured, and handrails are in place where necessary. Taking proactive measures to improve home safety can prevent injuries and further discomfort.
10. Overall Well-Being
Remember to take care of your overall well-being to manage osteoarthritis pain effectively. Utilize relaxation techniques such as meditation or deep breathing to reduce stress, which can exacerbate pain. Engage in activities that bring you joy and prioritize self-care to improve your overall quality of life.

Implementing these tips can help you find relief from sitting-induced osteoarthritis pain and enhance your sitting experience. Remember to consult with a healthcare professional for personalized advice tailored to your specific needs. By taking a proactive approach to managing your osteoarthritis pain, you can improve your comfort and overall well-being.
Recommendations for Managing Arthritis Pain at Home
Orthopedic experts provide valuable strategies for managing arthritis pain at home, especially when sitting for extended periods.
Strengthen Muscles Around Painful Joints
Perform gentle exercises to strengthen the muscles surrounding painful joints. This can help provide better support and stability, reducing discomfort while sitting.
Engage in Non-Impact Cardio Exercises
Participate in non-impact cardio exercises such as cycling or walking. These activities can improve circulation, promote joint mobility, and alleviate sitting-related arthritis pain.
Mindful Physical Activity and Rest
Be mindful of physical activity levels and avoid overexertion, which can exacerbate arthritis pain. Balancing activity with sufficient rest periods is essential for managing pain while sitting.
Reduce Stair Usage
Cutting down on the number of trips up and down stairs can relieve stress on the joints, particularly when sitting for extended periods.
Over-The-Counter Pain Medication and Heat/Cold Therapy
Consult with a healthcare professional or pharmacist about over-the-counter pain medication suitable for managing sitting-related arthritis pain. Additionally, heat and cold therapy, such as using heating pads or ice packs, can provide localized relief to painful joints.
Utilize Mobility Aids
Consider using mobility aids like canes or walkers to reduce pressure on the joints while sitting and moving around the house. These aids can provide additional support and stability.
Maintain a Healthy Diet and Weight
Adopting a healthy diet and maintaining an appropriate weight can decrease the strain on joints, contributing to better pain management while sitting.
Remove Hazards to Prevent Falls
Remove potential hazards in the home, such as loose rugs or cluttered pathways, to minimize the risk of falls that can lead to further joint pain and injury.
Practice Stress-Relief Techniques
Engage in stress-relief techniques like meditation or deep breathing exercises. Managing stress can help alleviate tension in the body and reduce overall arthritis pain.

Incorporating these tried-and-true strategies into your daily routine can significantly improve the management of osteoarthritis pain while sitting at home. By actively implementing these recommendations, individuals can experience relief and enhance their overall comfort level, contributing to a better quality of life.
Tips to Ease Joint Pain Throughout the Body
Joint pain can affect various parts of the body, and there are specific tips to ease pain in each area.
Neck Pain:
For neck pain, try using moist heat, practicing range-of-motion exercises, and maintaining good posture to help relieve discomfort.
Jaw Pain:
If you experience jaw pain, consider eating softer foods, using moist heat or cold therapy, and avoiding activities that worsen the pain.
Elbow Pain:
To manage elbow pain, focus on exercises that strengthen the muscles surrounding the joint.
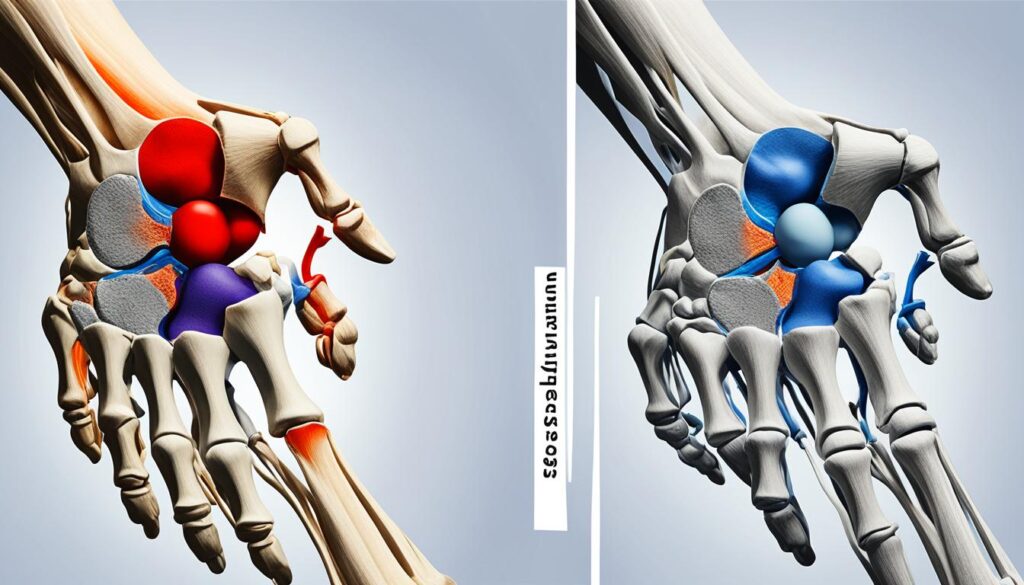
Wrist Pain:
Relieve wrist pain by utilizing functional splints and performing specific exercises to improve strength and flexibility.
Finger Pain:
To alleviate finger pain, use pens or pencils with soft grip covers, minimize handwriting when possible, and engage in hand exercises.
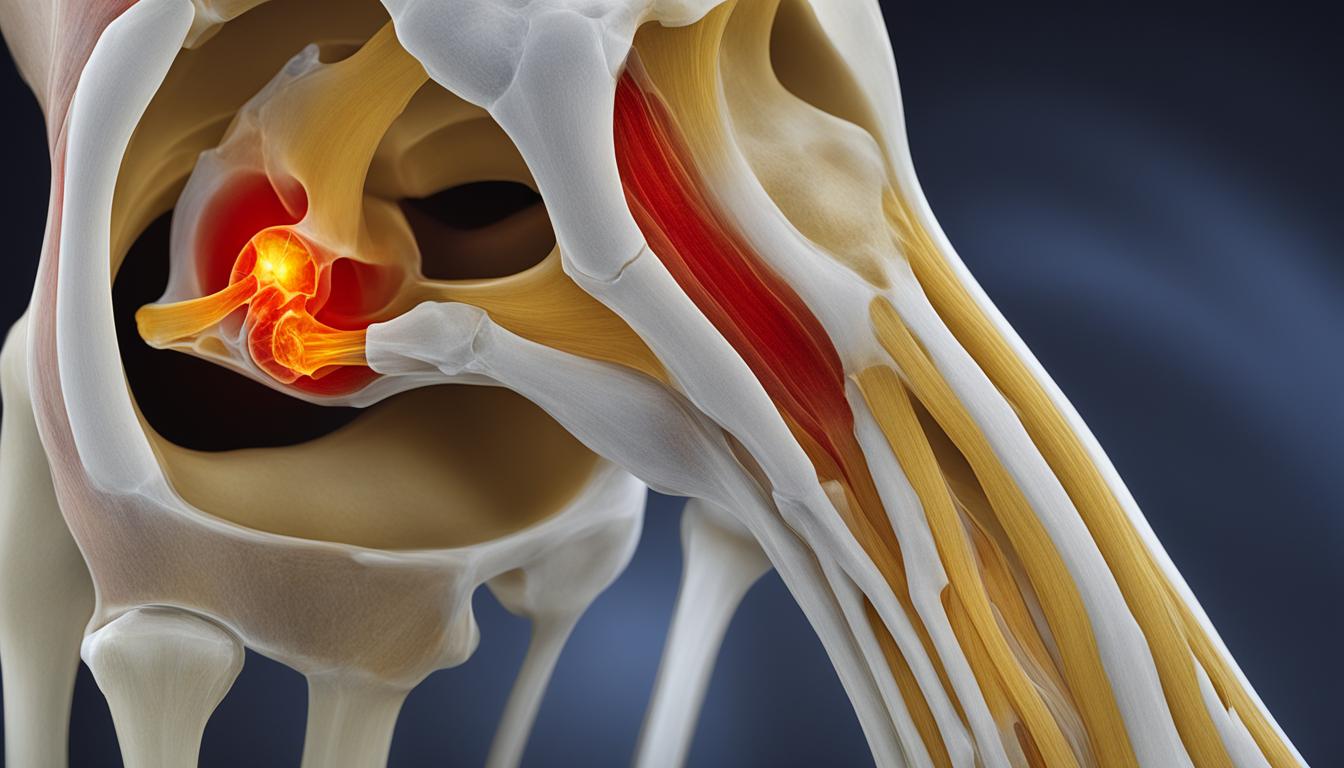
Hip Pain:
Manage hip pain with gentle range-of-motion exercises, warm baths, and maintaining a healthy level of activity.
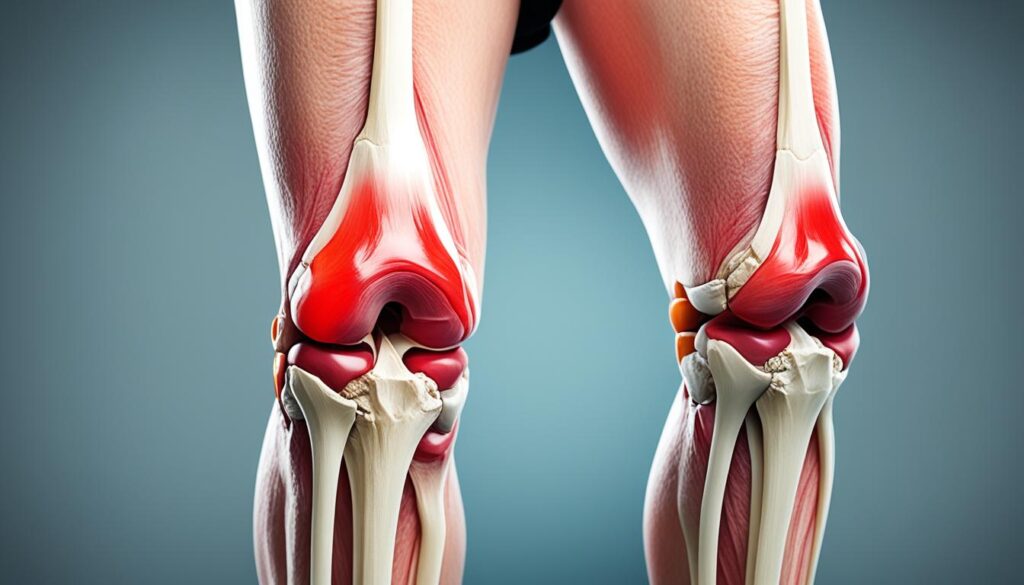
Knee Pain:
Relieve knee pain by taking rest breaks, using mobility aids as needed, and incorporating targeted exercises to strengthen the surrounding muscles.
Ankle and Foot Pain:
Address ankle and foot pain by utilizing orthotics, engaging in exercises that strengthen the supporting muscles, and wearing proper footwear.
| Body Area | Tips for Pain Relief |
|---|---|
| Neck | Moist heat, range-of-motion exercises, good posture |
| Jaw | Softer foods, moist heat or cold therapy, avoiding aggravating activities |
| Elbow | Exercises for muscle strengthening |
| Wrist | Functional splints, specific exercises |
| Fingers | Soft grip covers, minimizing handwriting, hand exercises |
| Hip | Range-of-motion exercises, warm baths, activity maintenance |
| Knee | Rest breaks, mobility aids, targeted exercises |
| Ankle and Foot | Orthotics, muscle-strengthening exercises, proper footwear |
Conclusion
Managing osteoarthritis pain while sitting is crucial for enhancing comfort and improving overall quality of life. By implementing a comprehensive approach that includes strategies for joint movement, posture, physical activity, weight management, pain medication, and therapies, individuals can find relief from sitting-related osteoarthritis pain. Adhering to these tips, consulting with healthcare professionals, and customizing the management plan to suit individual needs can make a significant difference in reducing pain and discomfort caused by osteoarthritis.
It is important to prioritize self-care and take proactive steps to manage sitting discomfort caused by osteoarthritis. By educating oneself about the condition and seeking support from loved ones, individuals can develop a holistic approach to pain management. Balancing activity and rest, managing weight, quitting smoking, and engaging in appropriate exercises can all contribute to reducing pain while sitting. Additionally, considering the use of medications and complementary therapies such as cognitive behavioral therapy, relaxation therapy, acupuncture, and heat/cold therapy can provide further pain relief.
To effectively manage osteoarthritis pain when sitting, it is crucial to address both the physical and emotional aspects of pain. By adopting a proactive and multi-faceted approach, individuals can find strategies that work best for them and achieve long-term relief. With the right combination of lifestyle changes, medical interventions, and self-care practices, it is possible to mitigate sitting-related osteoarthritis pain and improve overall well-being.
FAQ
What are some tips for managing osteoarthritis pain when sitting?
To manage osteoarthritis pain when sitting, you can try learning about your condition, enlisting support from healthcare professionals and loved ones, paying attention to joint movement, using good posture, balancing activity and rest, managing weight, quitting smoking, and engaging in appropriate exercises. Additionally, medications and therapies like cognitive behavioral therapy, relaxation therapy, acupuncture, and heat/cold therapy can provide relief.
How can I alleviate discomfort from osteoarthritis pain when sitting for long periods?
If you experience discomfort from osteoarthritis pain when sitting for long periods, you can try regularly getting up and walking around for at least five minutes every half hour, strengthening the muscles around painful joints through gentle exercises, engaging in non-impact cardio exercises, being mindful of physical activity that can worsen pain, taking over-the-counter pain medications or using topical creams containing capsaicin, and using heat and cold therapy. Using mobility aids like canes or walkers, maintaining a healthy weight, removing hazards in the home to prevent falls, and taking care of overall well-being through relaxation techniques and stress management can also contribute to managing osteoarthritis pain when sitting.
What strategies can I use to manage arthritis pain at home, particularly when sitting?
To manage arthritis pain at home, particularly when sitting, you can try strengthening the muscles around painful joints through gentle exercises, engaging in non-impact cardio exercises like cycling or walking, being mindful of physical activity and avoiding overexertion, making fewer trips up and down stairs, taking over-the-counter pain medication or using cold and heat therapy, using mobility aids to relieve pressure on joints, maintaining a healthy diet and weight, removing hazards in the home to prevent falls, and practicing stress-relief techniques like meditation or deep breathing. These strategies can help relieve osteoarthritis pain specifically when sitting.
Are there specific tips to ease joint pain in different parts of the body?
Yes, there are specific tips to ease joint pain in different parts of the body. For neck pain, using moist heat, practicing range-of-motion exercises, and maintaining good posture can help relieve discomfort. For jaw pain, eating softer foods, using moist heat or cold therapy, and avoiding activities that worsen pain can be beneficial. Elbow pain can be managed through exercises that strengthen the muscles, while wrist pain can be relieved with the help of functional splints and specific exercises. Finger pain can be alleviated by using pens or pencils with soft grip covers, avoiding handwriting when possible, and doing hand exercises. Hip pain can be managed through range-of-motion exercises and warm baths, and knee pain can be relieved with rest, the use of mobility aids, and specific exercises. Ankle and foot pain can be addressed with the use of orthotics, exercises that strengthen the muscles, and proper footwear.