Welcome to our comprehensive guide on knee osteoarthritis. If you are experiencing knee pain, it’s important to understand the signs that indicate when to see a doctor. Knee osteoarthritis is a common condition that affects the knee joint, causing symptoms such as pain, stiffness, and swelling. Left untreated, it can worsen over time and impact your daily life. In this article, we will discuss the key indicators that suggest it’s time to seek medical attention for your knees osteoarthritis.
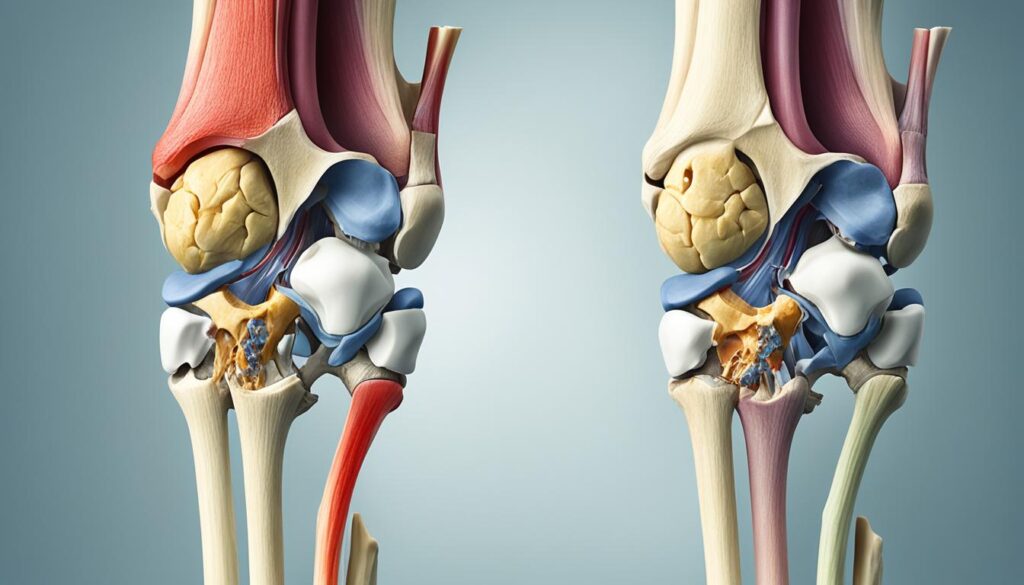
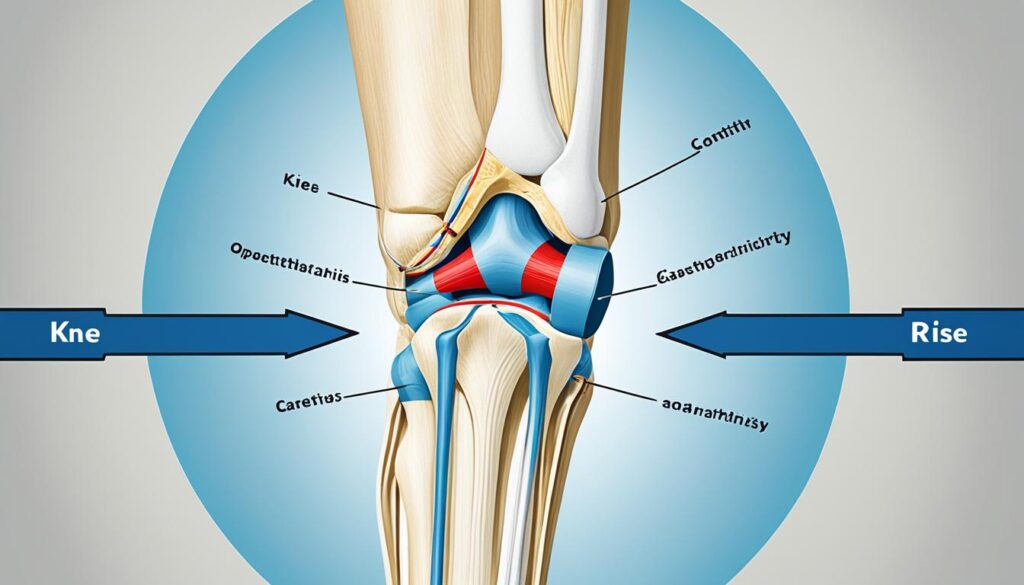
Understanding Knee Osteoarthritis
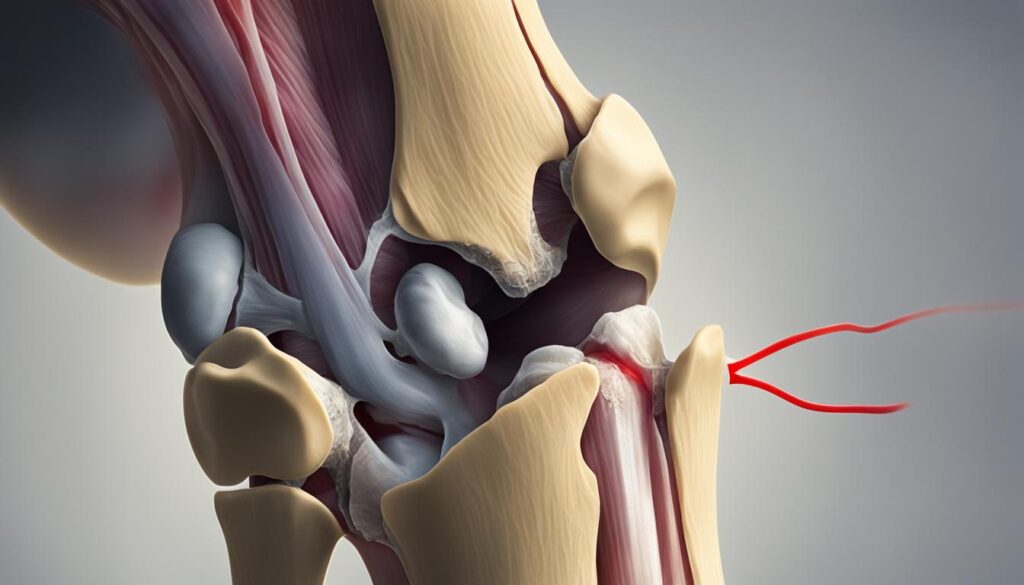
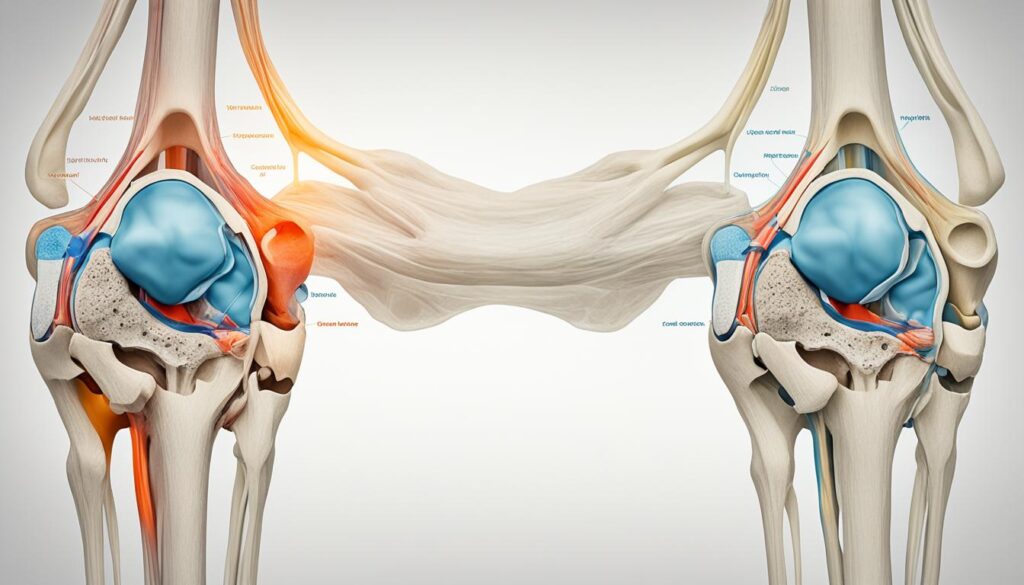
Knee osteoarthritis is a degenerative joint condition that occurs when the cartilage that cushions the ends of the knee joint wears down. This can result in pain, stiffness, swelling, and limited mobility. Understanding the causes and treatment options for knee osteoarthritis can help individuals manage their symptoms and improve their quality of life.
There are several factors that can contribute to the development of knee osteoarthritis. Age-related degeneration, wear and tear on the joint, obesity, joint injuries, repetitive stress, genetics, and certain metabolic diseases can all increase the risk of developing knee osteoarthritis.

Treatment options for knee osteoarthritis aim to alleviate pain, improve joint function, and slow the progression of the disease. These options include:
- Weight loss: Maintaining a healthy weight can reduce stress on the knee joint and ease symptoms.
- Exercise: Specific exercises can help strengthen the surrounding muscles, providing better support to the knee joint. Low-impact activities like swimming, cycling, and tai chi are often recommended.
- Pain relievers: Over-the-counter pain medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage pain and reduce inflammation.
- Injections: Corticosteroid injections can provide short-term pain relief, and hyaluronic acid injections can help lubricate the joint and reduce friction.
- Alternative therapies: Some individuals find relief through complementary treatments like acupuncture, physical therapy, or transcutaneous electrical nerve stimulation (TENS).
- Braces: Wearing knee braces or supports can provide stability and reduce pressure on the affected joint.
- Surgery: In severe cases, surgical interventions such as arthroscopy, osteotomy, or knee replacement may be necessary to restore mobility and alleviate pain.
It’s important to work closely with a healthcare professional to develop an individualized treatment plan that addresses your specific needs and goals. They will be able to assess the severity of your knee osteoarthritis, discuss treatment options, and guide you on the best course of action.
Quote:
“Understanding knee osteoarthritis and its treatment options is crucial for managing symptoms and improving joint function.” – Dr. Emily Davis, Rheumatologist
By adopting healthy lifestyle habits, following a personalized treatment plan, and staying proactive in self-care, individuals with knee osteoarthritis can minimize discomfort and maintain an active, fulfilling life.
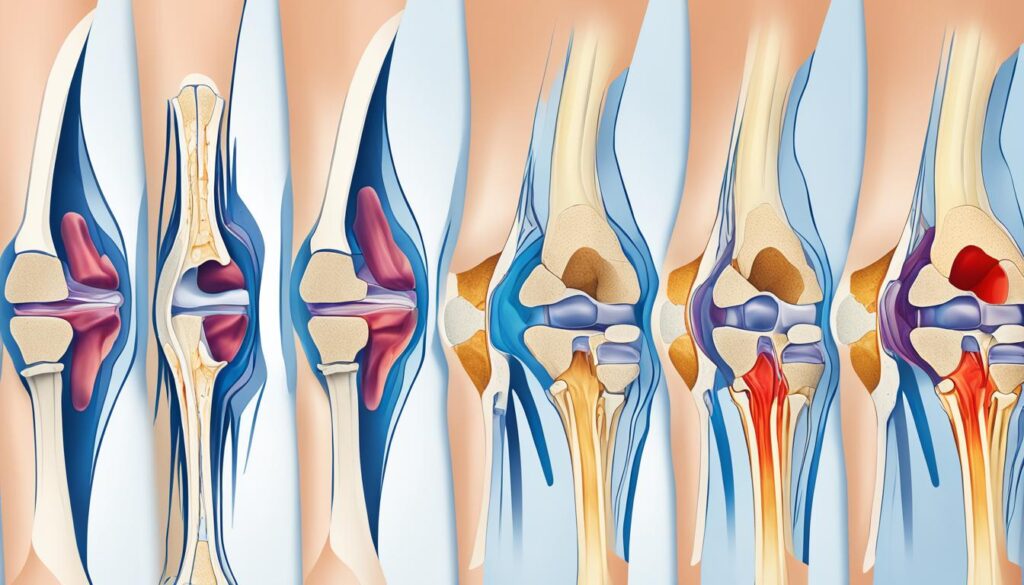
Common Symptoms of Knee Osteoarthritis
Symptoms of knee osteoarthritis often develop gradually and worsen over time. It’s essential to recognize these symptoms to seek timely medical attention. The most common symptoms of knee osteoarthritis include:
- Knee pain that worsens with activity: Pain in the knee joint, especially during movement or weight-bearing activities, is a typical symptom of knee osteoarthritis.
- Swelling: The affected knee may exhibit swelling, resulting from inflammation in the joint.
- Stiffness: Stiffness in the knee joint, particularly after long periods of sitting or in the morning, is a common symptom.
- Limited mobility: Knee osteoarthritis can restrict the range of motion in the affected knee, making it difficult to bend or straighten it fully.
- A creaking or cracking sound during movement: Some individuals may experience a creaking or cracking sensation in the knee joint when moving.
- Joint deformities: In advanced stages of knee osteoarthritis, the joint may undergo structural changes, resulting in visible deformities.
If you experience any of these symptoms for more than six months or if they significantly impact your daily life, it’s crucial to consult a doctor for a proper diagnosis and treatment plan. Early intervention can help manage symptoms and prevent further deterioration of the knee joint.

Note: The image above illustrates the common symptoms of knee osteoarthritis.
Risk Factors for Knee Osteoarthritis
Several factors can increase the risk of developing knee osteoarthritis. It’s important to be aware of these risk factors and take steps to minimize their impact on joint health. The key risk factors for knee osteoarthritis include:
- Age: Older age is a significant risk factor for knee osteoarthritis, as the wear and tear on joints over time can contribute to the development of the condition.
- Weight: Being overweight or obese puts extra stress on the knee joint, increasing the risk of developing osteoarthritis.
- Heredity: Some individuals may have a genetic predisposition to developing osteoarthritis, making them more susceptible to the condition.
- Gender: Women are more likely than men to develop knee osteoarthritis, although the reasons for this difference are not yet fully understood.
- Repetitive Stress Injuries: Engaging in activities that involve repeated stress on the knee joint, such as kneeling or squatting, can increase the risk of osteoarthritis.
- Athletics: Certain sports that place a high demand on the knees, such as soccer or basketball, can contribute to the development of knee osteoarthritis.
- Other Illnesses: Underlying conditions like rheumatoid arthritis or metabolic disorders can also increase the risk of developing knee osteoarthritis.
By understanding these risk factors, individuals can make lifestyle modifications and take preventive measures to reduce their chances of developing knee osteoarthritis. It is important to prioritize joint health through weight management, maintaining a physically active lifestyle, and seeking medical advice when necessary to ensure optimal joint function and overall well-being.
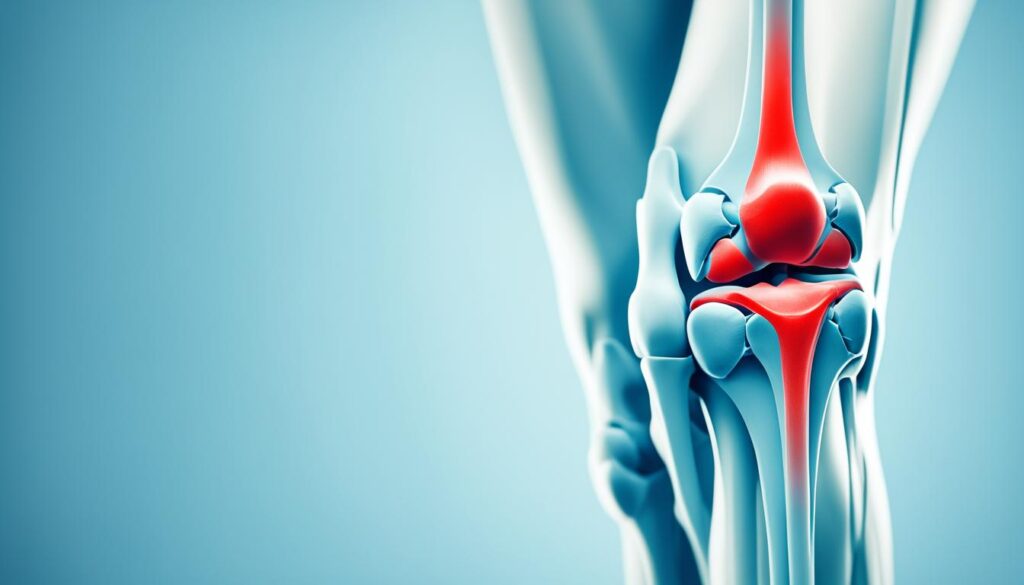
When to See a Doctor for Knee Osteoarthritis
If you have persistent knee pain or stiffness that doesn’t improve with rest or over-the-counter pain relievers, it’s recommended to see a doctor. Your doctor will perform a physical exam, review your medical history, and may order imaging tests such as X-rays or MRIs to confirm a diagnosis of knee osteoarthritis. Early diagnosis and treatment can help manage symptoms and slow the progression of the disease.
When it comes to knee osteoarthritis, it’s important to seek medical attention when:
- You experience persistent knee pain or stiffness that doesn’t improve with rest.
- Over-the-counter pain relievers fail to provide relief.
- Your knee begins to affect your daily activities or quality of life.
- Your symptoms worsen over time, impacting your mobility and flexibility.
By seeking medical advice promptly, you can receive an accurate diagnosis and begin appropriate treatment for knee osteoarthritis. Consulting with a doctor who specializes in joint health will ensure that you receive the most effective care tailored to your specific needs.
Diagnostic Procedures for Knee Osteoarthritis:
Your doctor may use the following diagnostic procedures to confirm knee osteoarthritis:
- Physical examination: Your doctor will assess your knee joint, looking for signs of inflammation, tenderness, or visible deformities.
- Medical history review: Your doctor will ask about your symptoms, previous injuries, and any family history of osteoarthritis.
- Imaging tests: X-rays can reveal joint damage, bone spurs, or narrowing of the joint space, while MRIs provide detailed images of soft tissues and cartilage.
Based on the findings, your doctor will diagnose knee osteoarthritis and develop an individualized treatment plan to address your specific needs.
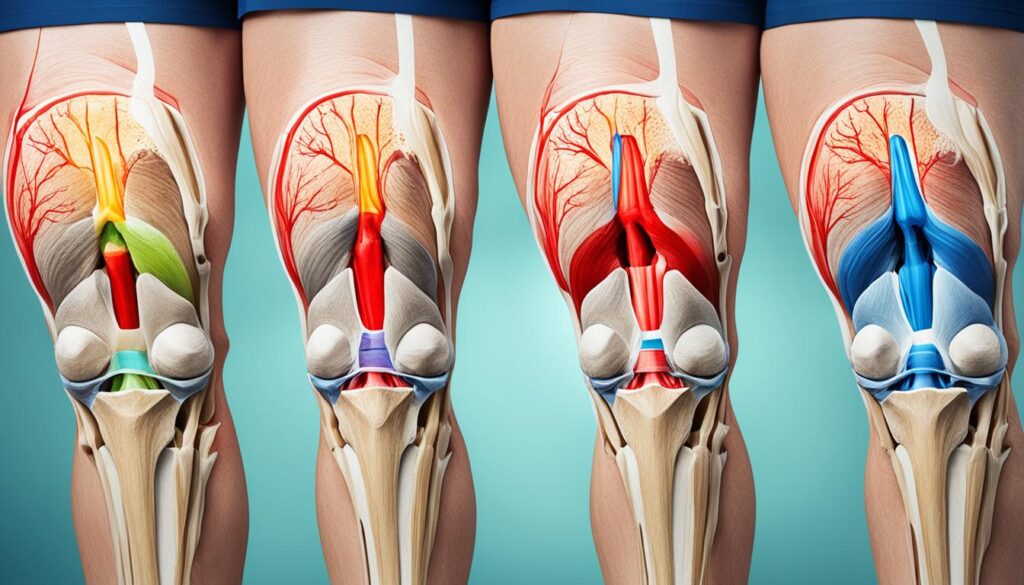
Treatment Options for Knee Osteoarthritis
When it comes to knee osteoarthritis treatment, there are various options available to relieve pain and improve joint function. The specific treatment plan will depend on the individual’s condition and preferences. Here are some common treatment options:
1. Weight Loss
Weight loss can significantly reduce the load on the knee joint, relieving pain and improving mobility. It is especially beneficial for individuals who are overweight or obese. A gradual approach to weight loss through proper diet and exercise is recommended.
2. Exercise
Engaging in regular exercise can help strengthen the muscles around the knee, providing support and stability. Low-impact exercises like swimming, cycling, and tai chi are gentle on the joint while improving flexibility and range of motion. Consult a physical therapist for a customized exercise plan.
3. Pain Relievers
Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage knee pain and reduce inflammation. However, long-term use should be discussed with a healthcare professional.
4. Injections
Injections of corticosteroids or hyaluronic acid may be recommended to provide temporary pain relief and reduce inflammation. Corticosteroids help reduce inflammation, while hyaluronic acid acts as a lubricant and shock absorber in the joint.
5. Alternative Therapies
Some individuals find relief from knee osteoarthritis symptoms through alternative therapies like acupuncture, massage, or the use of topical creams containing capsaicin or menthol. These therapies can help alleviate pain and improve overall well-being.
6. Braces
Braces or orthotic devices can provide support to the knee joint, redistribute forces, and reduce pain. They are commonly used for individuals with mild to moderate knee osteoarthritis and can be customized for a proper fit.
7. Surgery
In severe cases of knee osteoarthritis where conservative treatments have failed, surgery may be considered. Surgical options include arthroscopy to clean out the joint, osteotomy to realign the bones, or joint replacement surgery to replace the damaged joint with an artificial implant.
It’s important to consult with a healthcare professional specializing in knee osteoarthritis to discuss the best treatment options for your specific condition. They will consider factors such as the severity of symptoms, overall health, lifestyle, and personal preferences to create a comprehensive treatment plan.
| Treatment Option | Description |
|---|---|
| Weight Loss | Reduce load on the knee joint by losing excess weight through diet and exercise. |
| Exercise | Engage in low-impact exercises to strengthen knee muscles and improve joint flexibility. |
| Pain Relievers | Use over-the-counter pain relievers or prescribed NSAIDs to manage knee pain and reduce inflammation. |
| Injections | Receive corticosteroid or hyaluronic acid injections to relieve pain and inflammation. |
| Alternative Therapies | Explore non-traditional treatments like acupuncture or topical creams for pain relief. |
| Braces | Utilize braces or orthotic devices to support the knee joint and reduce pain. |
| Surgery | Consider surgical options such as arthroscopy, osteotomy, or joint replacement for severe cases. |
Self-Care and Prevention Tips for Knee Osteoarthritis
When it comes to knee osteoarthritis, self-care plays a crucial role in managing symptoms and preventing further deterioration. By adopting a few simple practices, individuals can promote joint health and improve their quality of life. Here are some effective self-care and prevention tips:
- Regular Exercise: Engaging in regular exercise, especially low-impact activities like swimming or cycling, can help strengthen the muscles around the knee and improve joint function. Exercise also helps in maintaining flexibility and reducing stiffness, promoting overall mobility.
- Maintain a Healthy Weight: Excess weight puts additional stress on the knee joint, increasing the risk of pain and discomfort. By maintaining a healthy weight through a balanced diet and portion control, individuals can reduce the pressure on their knees and minimize the progression of knee osteoarthritis.
- Joint Protection Techniques: When participating in physical activities or sports, it’s important to use proper joint protection techniques. Wearing supportive shoes and knee pads can help prevent injuries and reduce strain on the knee joint.
In addition to these self-care measures, consulting with healthcare professionals can provide personalized guidance and support in effectively managing knee osteoarthritis.
Conclusion
In conclusion, knee osteoarthritis is a common condition that impacts millions of individuals around the world. It is important to recognize the symptoms associated with knee osteoarthritis and understand when to seek medical attention. By consulting with healthcare professionals, individuals with knee osteoarthritis can obtain an early diagnosis and access appropriate treatment options.
Working together with healthcare providers, patients can effectively manage their symptoms, improve their joint function, and maintain a good quality of life. It is crucial to listen to your body, be proactive in seeking medical advice when needed, and take necessary steps to care for your knees.
If you experience persistent knee pain, stiffness, or any other symptoms related to knee osteoarthritis, do not hesitate to schedule an appointment with your doctor. Early intervention can make a significant difference in managing the condition and preventing further deterioration. Take control of your knee health and prioritize your overall well-being.
FAQ
When should I see a doctor for knee osteoarthritis?
It is recommended to see a doctor if you have persistent knee pain or stiffness that does not improve with rest or over-the-counter pain relievers.
What are the symptoms of knee osteoarthritis?
Common symptoms of knee osteoarthritis include knee pain, swelling, stiffness (especially in the morning or after prolonged sitting), limited mobility, a creaking or cracking sound during movement, and joint deformities.
What are the risk factors for knee osteoarthritis?
Risk factors for knee osteoarthritis include older age, being overweight or obese, hereditary factors, being female, having a history of joint injuries, engaging in repetitive stress activities, participating in certain sports, and having certain underlying illnesses such as rheumatoid arthritis or metabolic disorders.
How is knee osteoarthritis diagnosed?
To diagnose knee osteoarthritis, your doctor will perform a physical exam, review your medical history, and may order imaging tests such as X-rays or MRIs.
What are the treatment options for knee osteoarthritis?
Treatment options for knee osteoarthritis include weight loss, exercise to strengthen the muscles around the knee, pain relievers, injections of corticosteroids or hyaluronic acid, alternative therapies such as acupuncture or topical creams, braces, and surgery.
What can I do to manage knee osteoarthritis and prevent further deterioration?
Self-care measures for knee osteoarthritis include regular exercise, maintaining a healthy weight, using proper joint protection techniques, and following a comprehensive approach to knee health.
What is the most common form of arthritis?
Osteoarthritis is the most common form of arthritis.
What are the main joints affected by osteoarthritis?
Osteoarthritis mainly affects joints in the hands, knees, hips, and spine.