As a physical therapist with over 30 years of experience, I’ve helped countless patients identify and recover from meniscus tears. One of the most common questions I hear is: “What does a torn meniscus look like on the outside?” While diagnosis requires professional assessment, there are indeed visible external signs that can help you recognize a potential meniscus injury. In this comprehensive guide, I’ll walk you through what you might observe from the outside when dealing with this common knee injury.
![Knee Anatomy Showing Meniscus Location] Image suggestion: A clear anatomical diagram showing the knee joint with the medial and lateral meniscus highlighted, along with surrounding structures like femur, tibia, and ligaments.
Understanding the Meniscus: A Foundation for Recognition
Before discussing external appearances, it’s important to understand what we’re looking for. The meniscus is a C-shaped cartilage pad that sits between your femur (thigh bone) and tibia (shin bone). Each knee has two menisci – the medial meniscus on the inner side of the knee and the lateral meniscus on the outer side. These structures act as shock absorbers and help stabilize your knee joint during movement.
When tears occur, they disrupt this cushioning system, leading to changes that can sometimes be visible from the outside. However, it’s important to note that not all meniscus tears present with obvious external signs, especially in the early stages or with minor tears.
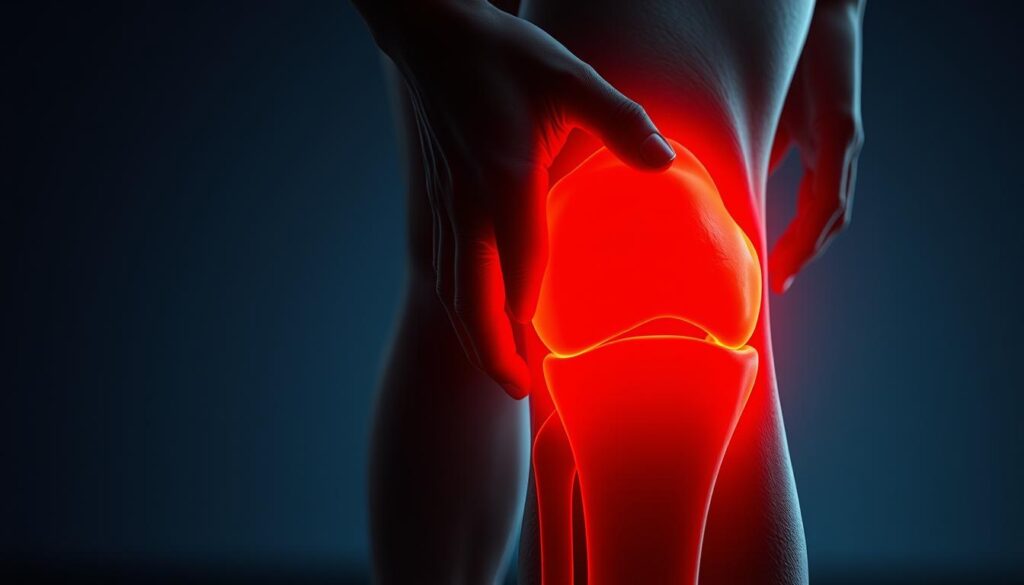
Initial Visual Signs After Injury
The earliest visible sign of a torn meniscus is often swelling around the knee joint. This swelling typically develops gradually over 24-48 hours after the injury, unlike an ACL tear where swelling often appears rapidly. Here’s what you might notice:
Localized Swelling Patterns
The swelling from a meniscus tear tends to be more localized than general knee swelling. For medial (inner) meniscus tears, which are more common, you might notice fullness along the inner joint line of the knee. For lateral (outer) meniscus tears, the swelling may be more prominent along the outer aspect of the knee.
![Knee with Joint Line Swelling] Image suggestion: A photograph showing a side-by-side comparison of a normal knee and one with visible joint line swelling characteristic of a meniscus tear. The image should highlight the subtle fullness along the joint line that indicates potential meniscus involvement.
This localized swelling creates a visible change in the normal contour of the knee. When comparing to the uninjured knee, you may notice that the natural depressions or dimples that normally exist around the knee joint appear filled in or puffier on the injured side.
Changes in Knee Contour
A healthy knee has a certain shape and profile with visible landmarks like the patella (kneecap) and the natural depressions around it. With a torn meniscus, these contours often change in subtle but noticeable ways:
- The joint line (where the thigh bone meets the shin bone) may appear fuller or more rounded
- The normal hollow areas on either side of the kneecap might appear filled in
- The overall symmetry of the knee compared to the uninjured side is disrupted
In my practice, I often ask patients to compare both knees while standing in front of a mirror – the differences in contour can sometimes be quite apparent even to untrained eyes.
Visual Differences Based on Tear Type
Different types of meniscus tears can present with varying external appearances:
[GRAPHIC: Types of Meniscus Tears and Their External Appearance] Graphic suggestion: An informative chart showing different types of meniscus tears (bucket handle, flap, radial, horizontal, degenerative) with corresponding illustrations of how each might affect the external appearance of the knee. Include brief bullet points of key visual indicators for each type.
Bucket Handle Tears: The Locked Knee Appearance
One of the most visually distinctive meniscus injuries is the bucket handle tear, where a large portion of the meniscus displaces into the joint. When this happens, the knee may become “locked,” unable to fully extend. From the outside, you might observe:
- The knee stuck in a slightly bent position, typically at about 15-30 degrees of flexion
- An inability to straighten the leg completely
- The quadriceps muscle appearing more tense on the affected side
- A noticeable difference in leg alignment when standing (if able to bear weight)
This locked position creates a very visible asymmetry between the legs that even untrained observers can often notice.
Degenerative Tears: Subtle Progressive Changes
Unlike traumatic tears that happen suddenly, degenerative meniscus tears develop gradually over time, usually in older adults. The external signs tend to be more subtle:
- Mild, intermittent swelling that comes and goes with activity
- Gradual changes in knee contour over weeks or months
- Less dramatic joint line fullness
- Occasional visible fluid accumulation after increased activity
These tears may not present with obvious external changes until they’ve progressed significantly, making them easier to miss by simply observing from the outside.
Functional Visual Signs in Daily Activities
Sometimes the most telling external signs of a meniscus tear appear during movement rather than at rest. As you observe someone with a suspected meniscus tear, you might notice:
![Person Demonstrating Difficulty with Stairs] Image suggestion: A photograph showing someone with a meniscus tear navigating stairs with visible compensatory movements, such as leading with the unaffected leg when descending or using a handrail for additional support.
Gait Changes
- A hesitation or shortened stance phase on the affected leg
- Reduced knee flexion during the swing phase of walking
- A tendency to rotate the foot outward on the affected side to reduce pressure on the torn meniscus
- Subtle limping, especially after sitting for prolonged periods
Difficulty with Specific Movements
Certain activities can make torn meniscus symptoms visibly apparent:
- Struggle to fully squat down (you might see the person compensate by shifting weight to the unaffected side)
- Difficulty with stair climbing, especially descending stairs
- Visible hesitation when transitioning from sitting to standing
- Tendency to keep the knee slightly bent when standing still
During my years as a physical therapist, I’ve observed that many patients unconsciously develop these movement adaptations to avoid pain, creating visible patterns that help indicate the presence of a meniscus injury.
Comparing with Other Knee Injuries
It can be challenging to differentiate a meniscus tear from other knee injuries based solely on external appearance. Here are some distinguishing features:
Meniscus Tear vs. ACL Tear
Meniscus Tear:
- More localized swelling, often along the joint line
- Swelling develops more gradually (24-48 hours)
- May have specific positions where the knee catches or locks
- Often can still bear weight, though with pain
ACL Tear:
- More diffuse, general knee swelling
- Rapid swelling development (within hours)
- Less likely to have mechanical locking
- Often more difficulty with weight bearing initially
Meniscus Tear vs. MCL Injury
Meniscus Tear:
- Swelling concentrated around the joint line
- Rarely shows visible bruising
- May demonstrate mechanical symptoms like locking or catching
MCL Injury:
- Swelling and potential bruising along the inner side of the knee
- Sometimes visible laxity with valgus (inward) stress
- Pain more concentrated along the ligament rather than the joint line
Visible Changes Over Time
The external appearance of a meniscus tear evolves over time:
![Timeline of Meniscus Tear Appearance] Image suggestion: A series of photographs showing the progression of how a knee with a meniscus tear appears at different stages – acute phase (1-3 days post-injury), subacute phase (1-3 weeks), and chronic phase (1+ months), highlighting how swelling patterns and visual indicators change.
Acute Phase (First Few Days)
- Initial swelling development
- Possible slight redness or warmth
- Protective posturing of the leg
Subacute Phase (Days to Weeks)
- Peak swelling that gradually subsides
- Development of muscle guarding patterns
- Compensatory movement patterns become more established
Chronic Phase (Weeks to Months)
- Possible visual signs of quadriceps atrophy (muscle wasting)
- Established movement compensations
- Periodic episodes of increased swelling with certain activities
- Joint line changes that become more permanent
In my practice, I’ve observed that untreated meniscus tears often lead to visible quadriceps atrophy (muscle shrinking) on the affected side after several weeks. This creates an asymmetrical appearance when comparing both legs, with the thigh of the injured leg appearing slightly smaller or flatter.
Documentation for Medical Visits
If you suspect a meniscus tear and plan to see a healthcare provider, documenting the external appearance can be helpful:
- Take photos of both knees from the front, side, and above for comparison
- Record a video of your walking pattern
- Note when swelling increases or decreases
- Document which activities produce visible changes in your knee
These visual records can help your healthcare provider make a more accurate assessment and track changes over time.
When the Outside Doesn’t Tell the Full Story
It’s crucial to understand that not all meniscus tears have obvious external signs. In fact, many smaller tears or those in less vascularized regions of the meniscus might show minimal external changes while still causing significant internal disruption and pain.
Some patients with severe tears show surprisingly little external evidence, while others with minor tears may develop significant swelling and visible changes. This variability is why professional diagnosis that includes imaging (usually MRI) is essential for confirming a torn meniscus.
Red Flag Visual Signs Requiring Immediate Attention
While most meniscus tears don’t constitute medical emergencies, certain visual signs warrant immediate medical attention:
- Severe deformity of the knee
- Inability to bear any weight on the affected leg
- Dramatic swelling that develops very rapidly (within an hour or two)
- Visible bruising that spreads quickly
- Redness and warmth accompanied by fever (could indicate infection)
These signs might indicate a more serious injury or complication beyond a simple meniscus tear.
Non-Surgical Management and Healing Signs
With proper treatment, the external appearance of a knee with a meniscus tear should gradually normalize. Positive visual signs of healing include:
- Reduction in swelling with joint line contours returning to normal
- Restoration of symmetrical appearance compared to the uninjured knee
- Improved gait pattern with less visible compensation
- Return of normal muscle definition as protective guarding subsides
- Ability to perform movements like squatting with more normal appearance
Physical therapy plays a crucial role in this normalization process. Through targeted exercises, manual techniques, and modalities, we work to reduce swelling, restore normal movement patterns, and strengthen supporting muscles. Many of my patients are surprised at how much better their knee looks from the outside after completing a rehabilitation program, even without surgical intervention.
Post-Surgical Appearance
If surgical intervention is required, the external appearance will naturally change during recovery:
![Post-Arthroscopic Knee] Image suggestion: A photograph showing a knee shortly after arthroscopic meniscus repair, with small portal incisions visible, to help patients understand what to expect after surgical intervention. Include the typical placement of the 2-3 small incisions.
- Initial surgical dressings and bandages
- Temporary increase in swelling post-procedure
- Small arthroscopic portal scars (typically 2-3 small incisions)
- Gradual return to normal contours as rehabilitation progresses
Most arthroscopic meniscus procedures result in minimal long-term changes to the external appearance of the knee. The small surgical scars typically fade significantly within a year.
Conclusion: The Importance of Professional Assessment
While recognizing the external signs of a meniscus tear can help alert you to a potential problem, these visual cues should never replace professional medical evaluation. The outside appearance provides just one set of clues in the diagnostic puzzle.
In my three decades as a physical therapist, I’ve learned that combining careful observation of external signs with a thorough clinical examination and appropriate imaging is the most reliable approach to diagnosing meniscus injuries. If you notice any of the signs we’ve discussed, I encourage you to seek professional medical advice for proper diagnosis and treatment.
Remember that early intervention for meniscus tears often leads to better outcomes, so don’t delay seeking care if you suspect this injury. With proper treatment, most patients can return to pain-free movement with little to no lasting visible changes to their knee.

![[Image 1: Hero image showing person wearing smartwatch while experiencing knee pain, with data visualization overlay]](https://kneehurt.com/wp-content/uploads/2025/06/download-7.jpeg)
![[Image 2: Split-screen comparison showing traditional pain diary vs. smartwatch data dashboard]](https://kneehurt.com/wp-content/uploads/2025/06/download-4.jpeg)

![[Image 4: Smartphone screen showing multiple pain tracking apps with smartwatch companion displays]](https://kneehurt.com/wp-content/uploads/2025/06/download-5.jpeg)
![[Image 5: Dashboard screenshot showing comprehensive pain tracking data with highlighted patterns and insights]](https://kneehurt.com/wp-content/uploads/2025/06/download-17.png)
![[Image 6: Futuristic concept image showing advanced smartwatch features and AI-powered health insights]](https://kneehurt.com/wp-content/uploads/2025/06/download-6.jpeg)
![[Image 7: Before/after comparison charts showing pain reduction and improvement metrics for each case study]](https://kneehurt.com/wp-content/uploads/2025/06/download-18.png)