Have you ever wondered why knee pain occurs when you sit cross-legged? This common position can put unexpected stress on your knees, leading to discomfort and pain. We will explore the reasons behind this phenomenon and discuss the structures within the knee that are affected by this sitting position.
Many individuals experience pain in their knees when sitting cross-legged due to various factors, including muscle imbalances, poor alignment, and previous injuries. Understanding the causes of this discomfort is crucial for effective management and relief.
We will examine the symptoms associated with knee pain in this position and outline when it is necessary to seek medical attention. By introducing various management strategies, we aim to help you differentiate between temporary discomfort and more serious underlying conditions.
Key Takeaways
- Common causes of knee pain when sitting cross-legged
- Structures in the knee affected by this position
- Factors contributing to pain, such as muscle imbalances and previous injuries
- Symptoms associated with knee pain and when to seek medical help
- Management strategies for effective pain relief
Understanding Knee Pain When Sitting Cross-Legged
The cross-legged sitting position is known to cause stress on the knee joint. This stress can lead to discomfort and pain in the knee area. We will explore the reasons behind this phenomenon and the common symptoms associated with it.
Why Cross-Legged Sitting Causes Discomfort
When sitting cross-legged, the knee joint is subjected to unusual stress. This position can compress certain areas of the knee while stretching others, leading to an imbalance that may cause pain. The patella (kneecap) and surrounding soft tissues are particularly affected.
Prolonged sitting in this position can exacerbate existing knee conditions or create new problems through repetitive stress.
Common Symptoms to Recognize
Common symptoms of knee pain from cross-legged sitting include dull aching, stiffness when standing up, and discomfort that worsens with time. It’s essential to distinguish between normal discomfort from sitting positions and pain that might indicate an underlying problem requiring attention.
| Factor | Influence on Knee Pain |
|---|---|
| Age | Increased age can lead to reduced flexibility and more pronounced knee pain. |
| Flexibility | Lower flexibility can increase the stress on the knee joint, leading to more discomfort. |
| Previous Knee Injuries | Pre-existing injuries can make the knee more susceptible to pain when sitting cross-legged. |
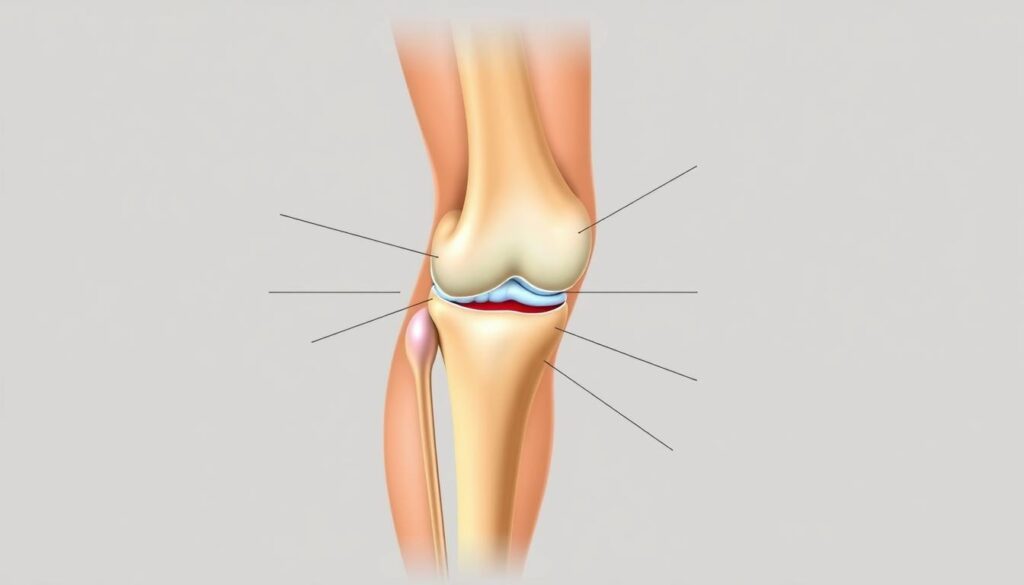
Anatomy of the Knee Joint
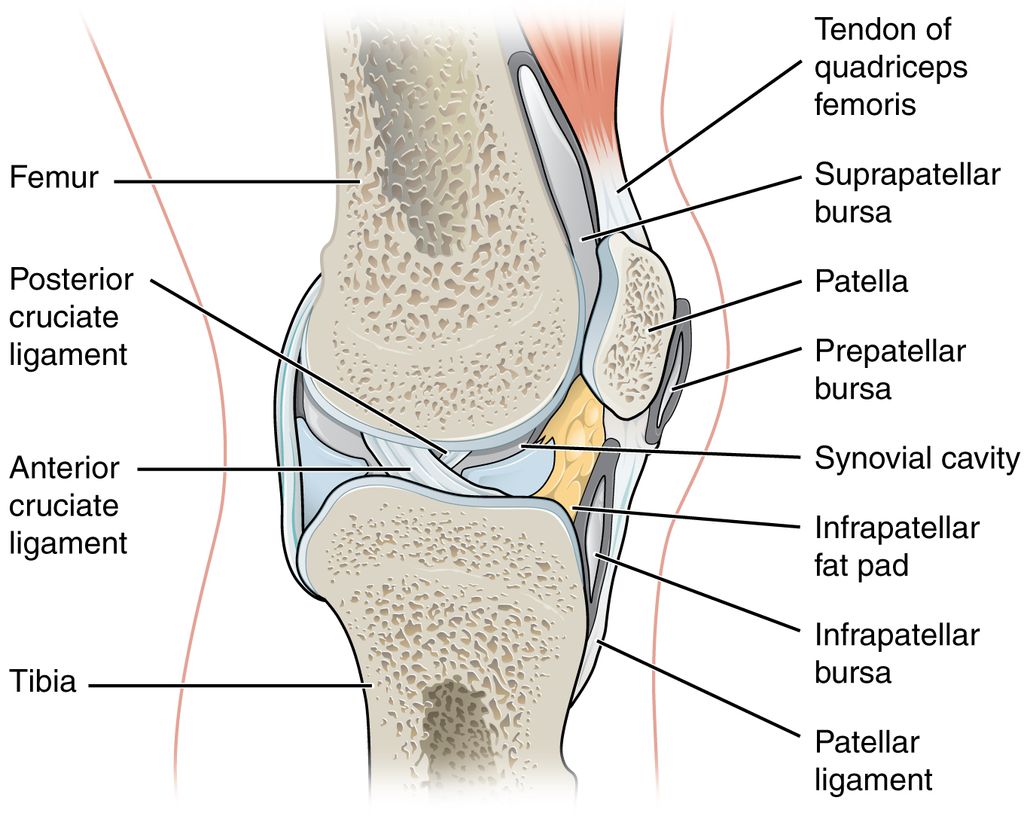
The complex structure of the knee joint, comprising bones, ligaments, tendons, and cartilage, works together to provide support and facilitate movement. The knee is the largest and strongest joint in the human body, playing a vital role in our daily activities.
Key Structures of the Knee
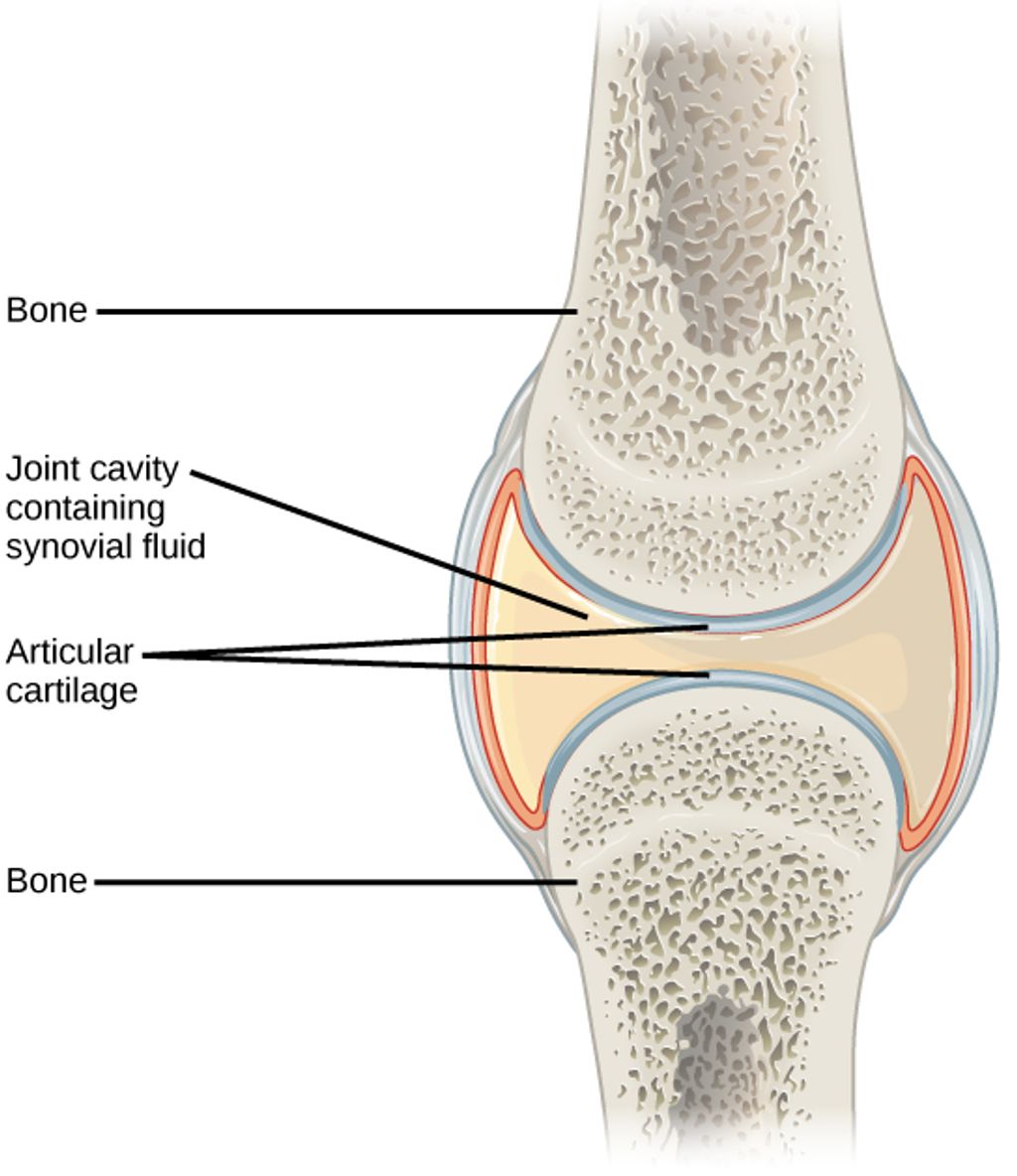
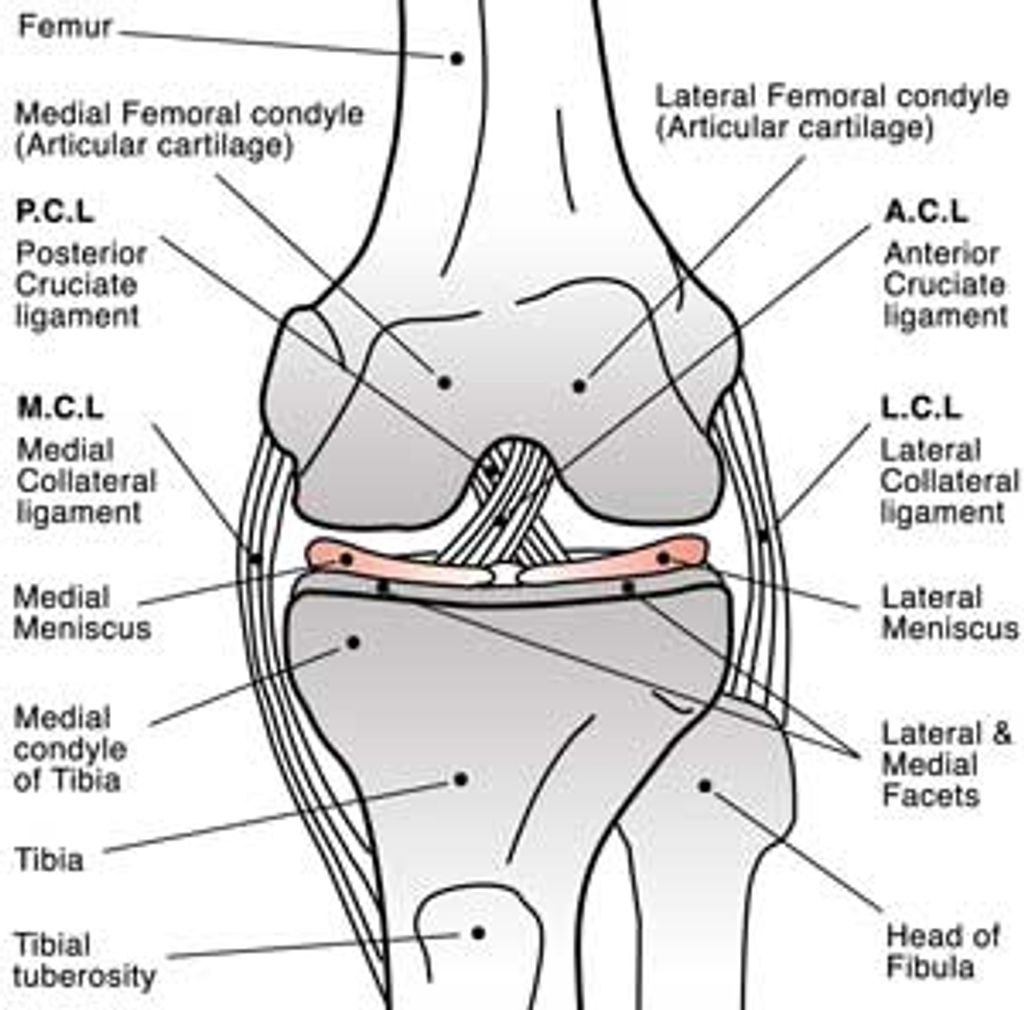
The knee joint is made up of three bones: the femur (thighbone), tibia (shinbone), and patella (kneecap). The ends of these bones are covered with articular cartilage, a smooth substance that protects and cushions them as we bend and straighten our knee. Ligaments connect bones to other bones, while tendons connect muscles to bones. The quadriceps tendon and patellar tendon are crucial for knee movement.
| Structure | Description | Function |
|---|---|---|
| Femur, Tibia, Patella | Bones forming the knee joint | Provide the framework for the knee |
| Articular Cartilage | Smooth, slippery substance covering bone ends | Cushions and protects bones during movement |
| Ligaments (ACL, PCL, MCL, LCL) | Connect bones to other bones | Provide stability to the knee joint |
| Tendons (Quadriceps, Patellar) | Connect muscles to bones | Enable knee movement and strength |
How These Structures Work Together
The knee’s various structures work in harmony to provide a wide range motion while supporting the body’s weight. Proper alignment of these structures is crucial for pain-free knee function. Misalignment or damage to any of these components can lead to discomfort and increase the risk of injuries. The synovial fluid in the knee joint provides lubrication and nutrition to the joint surfaces, further facilitating smooth movement.
Common Causes of Knee Pain When Sitting Cross-Legged
Various factors can contribute to knee pain when adopting a cross-legged sitting position. The knee joint is complex and involves multiple structures that can be affected by different conditions.
Arthritis and Inflammatory Conditions
Arthritis is a common cause of knee pain. Osteoarthritis, the most prevalent form, results from cartilage breakdown, leading to bone-on-bone contact and pain. Inflammatory arthritis, including rheumatoid arthritis and psoriatic arthritis, causes joint inflammation and can exacerbate pain when sitting cross-legged.
| Type of Arthritis | Cause of Pain | Effect on Knee |
|---|---|---|
| Osteoarthritis | Cartilage breakdown | Bone-on-bone contact |
| Inflammatory Arthritis | Joint inflammation | Swelling and pain |
Patellofemoral Pain Syndrome (Runner’s Knee)
Patellofemoral pain syndrome, also known as Runner’s Knee, is characterized by pain around or behind the kneecap. This condition is often due to improper tracking of the patella and can be aggravated by sitting cross-legged.
Tendonitis and IT Band Syndrome
Tendonitis occurs when the tendons supporting the knee become inflamed. The iliotibial (IT) band syndrome causes a burning pain on the outside of the knee. Both conditions can be irritated by the cross-legged position, leading to discomfort.
Understanding these common causes can help in addressing knee pain effectively. It’s essential to identify the underlying condition to apply the appropriate treatment.
Additional Factors Contributing to Knee Pain
Beyond the obvious causes, several additional factors can contribute to knee pain when sitting cross-legged. The complex interplay of muscles, alignment, and activity level can all impact the knee joint.
Muscle Imbalances and Weakness
Muscle imbalances, particularly between the quadriceps and hamstrings, can significantly contribute to knee pain. Weakness in the quadriceps muscles can lead to poor tracking of the kneecap, causing discomfort. Additionally, weak hip muscles, such as the gluteus medius, can result in poor knee alignment, increasing stress on the joint.
Poor Alignment and Posture
Poor posture and alignment throughout the kinetic chain, from feet to spine, can impact knee function and comfort. When the body is not properly aligned, it can put additional stress on the knee joint, leading to pain when sitting cross-legged. For more information on how alignment affects knee health, visit https://kneehurt.com/knee-hurts/.
Overuse and Training Errors
Overuse from repetitive activities or sudden increases in activity level can create microscopic damage to knee structures, making them more sensitive to stress. Improper training techniques, inadequate warm-up, or inappropriate footwear can also contribute to knee pain. It’s essential to be mindful of these factors to prevent and manage knee pain effectively.

Diagnosing the Source of Your Knee Pain
Diagnosing knee pain when sitting cross-legged involves a comprehensive approach to identify the underlying cause. We will guide you through the process of determining the source of your knee pain.
When to See a Healthcare Provider
If your knee pain persists and interferes with your daily activities, it’s time to consult a healthcare provider. Key indicators include persistent pain, swelling, instability, or pain that affects your daily routine.Don’t ignore these signs; seeking medical attention can prevent further complications.
What to Expect During Examination
During the physical examination, your doctor will assess various aspects of your knee and surrounding areas. This includes checking the alignment of the lower leg and the position of the kneecap, knee stability, hip rotation, and range of motion of knees and hips. Your doctor will also examine the kneecap for signs of tenderness and evaluate the strength, flexibility, and tone of your thigh muscles.
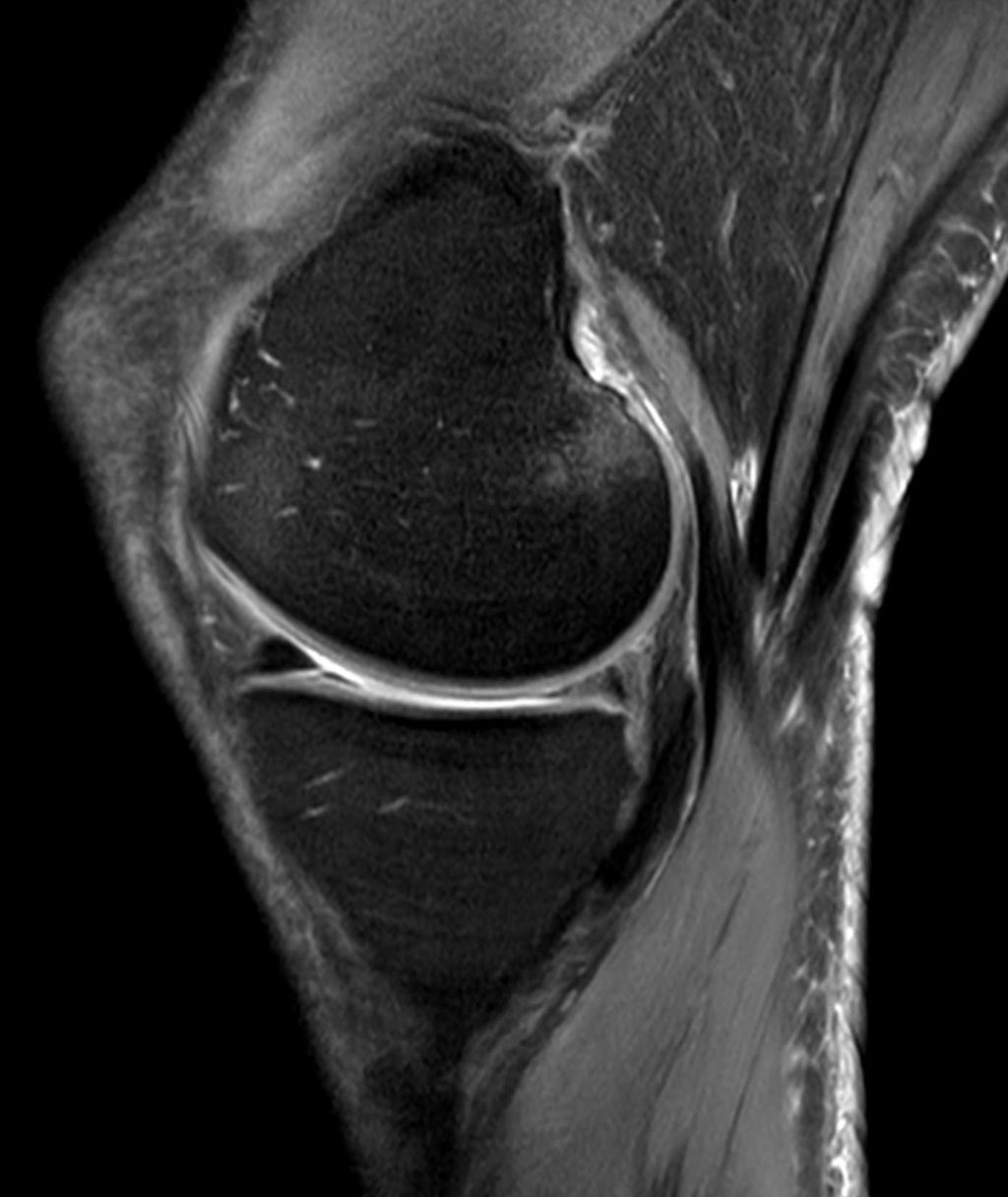
Diagnostic Tests and Procedures
To accurately diagnose the cause of your knee pain, your doctor may order diagnostic tests. These can include X-rays to evaluate bone structure and alignment, MRI scans to assess soft tissue damage, or ultrasound to visualize inflammation. A comprehensive diagnosis often involves ruling out various conditions through a combination of patient history, physical examination, and diagnostic imaging.
As noted by medical professionals, “A thorough diagnosis is crucial for developing an effective treatment plan.” This involves differentiating between various causes of knee pain, from simple muscle tightness to more serious structural problems.
| Diagnostic Test | Purpose |
|---|---|
| X-rays | Evaluate bone structure and alignment |
| MRI Scans | Assess soft tissue damage |
| Ultrasound | Visualize inflammation |
Accurate diagnosis is essential for effective treatment. By understanding the cause of your knee pain, you can work with your healthcare provider to develop a tailored treatment plan.
Effective Treatment Options for Knee Pain
Effective management of knee pain involves a multi-faceted approach, including several treatment options. When experiencing knee pain, especially when sitting cross-legged, it’s crucial to consider various strategies to alleviate the discomfort.
Rest and Activity Modification
One of the first steps in treating knee pain is to modify or avoid activities that exacerbate the condition. Switching to low-impact activities like biking, swimming, or yoga can help reduce stress on the knee joint. Resting the knee and changing the training routine can significantly relieve pain.
Ice and Heat Therapy
Applying ice after physical activity can help relieve discomfort. It’s essential to wrap the ice pack in a towel to avoid direct contact with the skin and apply it for about 20 minutes at a time. Heat therapy can also be beneficial, particularly for chronic pain, by increasing blood flow to the area.
Medications for Pain Relief
Over-the-counter medications such as ibuprofen and naproxen can help relieve knee pain. These medications reduce inflammation and alleviate pain, making it easier to perform daily activities.
Physical Therapy Approaches
Physical therapy plays a crucial role in treating knee pain. Targeted exercises can improve the range of motion, strength, and endurance. Focusing on strengthening the quadriceps is particularly important as these muscles are key stabilizers of the kneecap.
A comprehensive treatment plan may include a combination of these approaches. Consulting with a healthcare provider or a physical therapist can help determine the most effective treatment strategy for individual cases of knee pain.
Therapeutic Exercises to Relieve Knee Pain When Sitting Cross-Legged
Therapeutic exercises play a crucial role in relieving knee pain when sitting cross-legged. These exercises are designed to improve range of motion, strength, and endurance, ultimately helping to alleviate discomfort and support knee health.
Quadriceps Strengthening Exercises
Strengthening the quadriceps muscles is essential for stabilizing the kneecap and reducing pain. Effective exercises include straight leg raises, wall sits, and mini-squats. For example, straight-leg raises involve lying on your back, tightening your quadriceps, and lifting your leg about 12 inches off the ground before slowly lowering it back down.
Hamstring and Hip Flexibility Exercises
Improving hamstring and hip flexibility can reduce stress on the knee joint and enhance overall mobility. Various stretches and mobility drills can be beneficial, such as hamstring stretches and hip flexor stretches. These exercises help maintain or improve range of motion, making it easier to sit comfortably without exacerbating knee pain.
Balance and Stability Training
Balance and stability training exercises are vital for improving proprioception and neuromuscular control around the knee. This type of training helps prevent pain during various sitting positions by enhancing the body’s ability to maintain proper knee alignment.
Proper Form and Technique
Maintaining proper form and technique during therapeutic exercises is crucial for their effectiveness and safety. It’s essential to avoid common mistakes and progress gradually to more challenging exercises as symptoms improve. Consulting with a physical therapist can provide personalized guidance and help create a comprehensive exercise routine.
Prevention Strategies for Long-Term Knee Health
Preventing knee pain requires a multifaceted approach that includes proper exercise, weight management, and awareness of sitting ergonomics. We can reduce the risk of knee pain by maintaining a healthy body weight, practicing proper sitting ergonomics, and engaging in regular low-impact exercises like swimming and cycling. Incorporating stretching and strengthening routines into daily life and wearing proper footwear also play crucial roles. By adopting these habits and being mindful of our activity levels, we can promote long-term knee health and reduce the risk of knee pain.
FAQ
What are the common causes of knee discomfort when sitting cross-legged?
We often experience knee discomfort due to various factors, including arthritis, patellofemoral pain syndrome, and tendonitis. These conditions can be triggered by muscle imbalances, poor alignment, and overuse.
How can I relieve knee pain caused by sitting cross-legged?
We can alleviate knee pain by modifying our activities, applying ice and heat therapy, and using physical therapy approaches. Strengthening our quadriceps and hamstring muscles through exercises can also help.
What are the benefits of physical therapy for knee pain?
Physical therapy can help us identify and address underlying issues, such as muscle imbalances and poor posture. Our physical therapist can create a personalized exercise program to improve our knee joint mobility and strength.
Can knee pain be prevented?
Yes, we can take steps to prevent knee pain by maintaining a healthy weight, engaging in regular exercise, and using proper techniques when performing activities. We can also incorporate exercises that improve our balance and stability.
When should I see a healthcare provider for knee pain?
We should consult a healthcare provider if our knee pain persists or worsens over time, or if we experience swelling, stiffness, or limited mobility. A proper diagnosis and treatment plan can help us address the underlying cause of our knee pain.
What diagnostic tests may be used to determine the cause of knee pain?
Our healthcare provider may use various diagnostic tests, including X-rays, MRI, or CT scans, to determine the underlying cause of our knee pain. These tests can help identify conditions such as arthritis, tendonitis, or ligament sprains.