Welcome to our comprehensive guide on managing hypermobile knees. In this article, we will provide you with valuable tips and information on how to effectively deal with knee instability and hypermobility, as well as ways to alleviate knee pain and promote joint health.
Key Takeaways:
- Hypermobile knees can cause pain and instability due to very flexible joints and joint laxity.
- Common symptoms include fatigue, recurrent sprains, joint dislocations, and poor balance.
- A doctor can diagnose hypermobile knees using the Beighton scoring system.
- Treatment involves improving muscle strength, pain relief, and self-care measures.
- Prioritizing joint protection and following healthcare professionals’ advice is crucial for effective management.
What is Joint Hypermobility Syndrome?
Joint hypermobility syndrome is a condition characterized by very flexible joints that can cause pain, stiffness, and other symptoms. It is often diagnosed in children and young people and is usually not accompanied by any other underlying conditions.
Common symptoms of joint hypermobility syndrome include:
- Fatigue
- Joint and muscle pain and stiffness
- Recurrent sprains and strains
- Joint dislocations
- Poor balance and coordination
- Thin and stretchy skin
- Bladder or bowel problems
To diagnose joint hypermobility syndrome, a GP will typically use the Beighton scoring system to assess joint flexibility. This involves evaluating a number of specific joint movements, such as bending the pinky finger backward beyond 90 degrees, touching the floor with palms while keeping knees straight, and more.
“Joint hypermobility syndrome is a condition characterized by very flexible joints that can cause pain, stiffness, and other symptoms.”
Treatment for joint hypermobility syndrome aims to improve muscle strength and fitness, which helps protect the joints and reduce symptoms. This often involves physiotherapy or occupational therapy to target specific muscles and enhance joint stability.
Pain relief can be achieved through over-the-counter options such as paracetamol and anti-inflammatory painkillers. In some cases, a GP may refer individuals with joint hypermobility syndrome to a pain clinic for additional management.
Supportive measures at home can also be beneficial for managing joint hypermobility syndrome, such as gentle exercise, maintaining a healthy weight, wearing supportive shoes, and avoiding excessive joint movements.
When to Book a GP Appointment for Joint Hypermobility Syndrome?
If you experience symptoms of joint hypermobility syndrome, it is important to consult with a GP for evaluation and diagnosis. The following scenarios warrant a GP appointment:
- If you have persistent joint pain or stiffness
- If you frequently experience joint dislocations or sprains
- If you notice changes in your skin texture or other unusual symptoms
- If you have difficulty with balance and coordination
- If you have bladder or bowel problems
During the GP appointment, the doctor will inquire about your symptoms, perform a physical examination, and use the Beighton scoring system to assess your joint flexibility. Based on the results, they can provide a diagnosis and recommend appropriate treatment options.
It is essential to seek medical attention for joint hypermobility syndrome to ensure accurate diagnosis and effective management of symptoms. Early intervention can help prevent complications and improve your quality of life.
Hypermobile Joints: Causes and Outlook
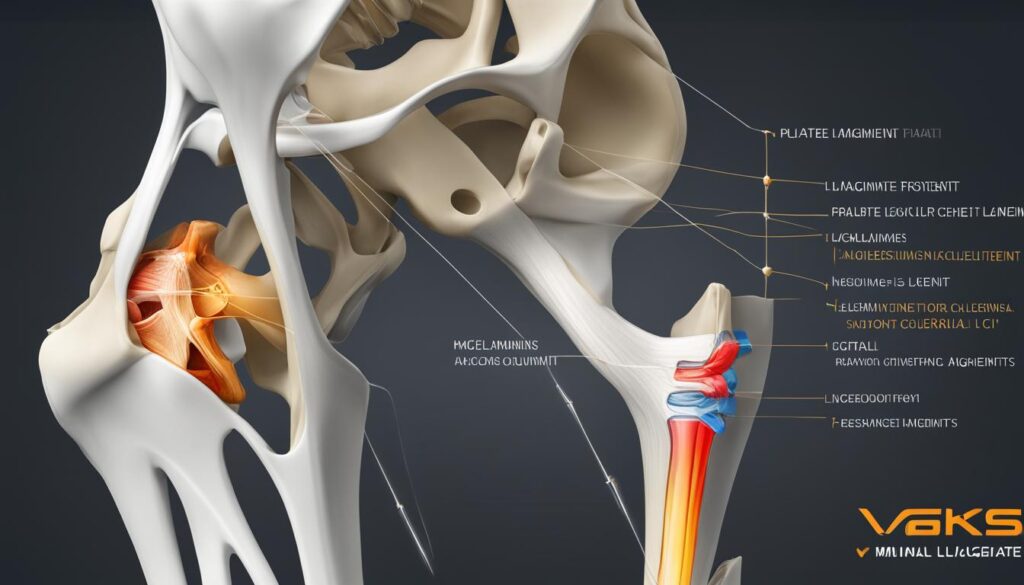
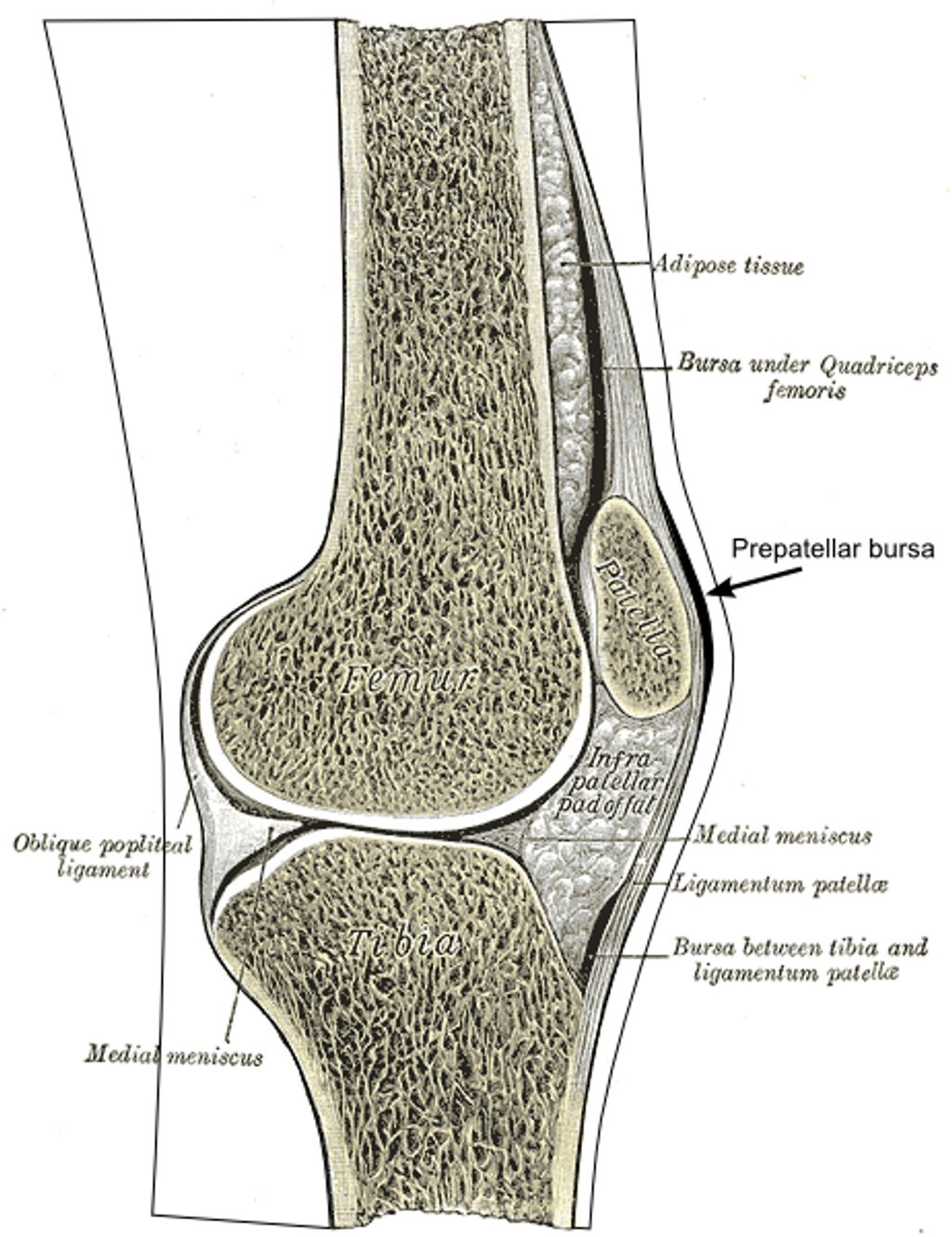
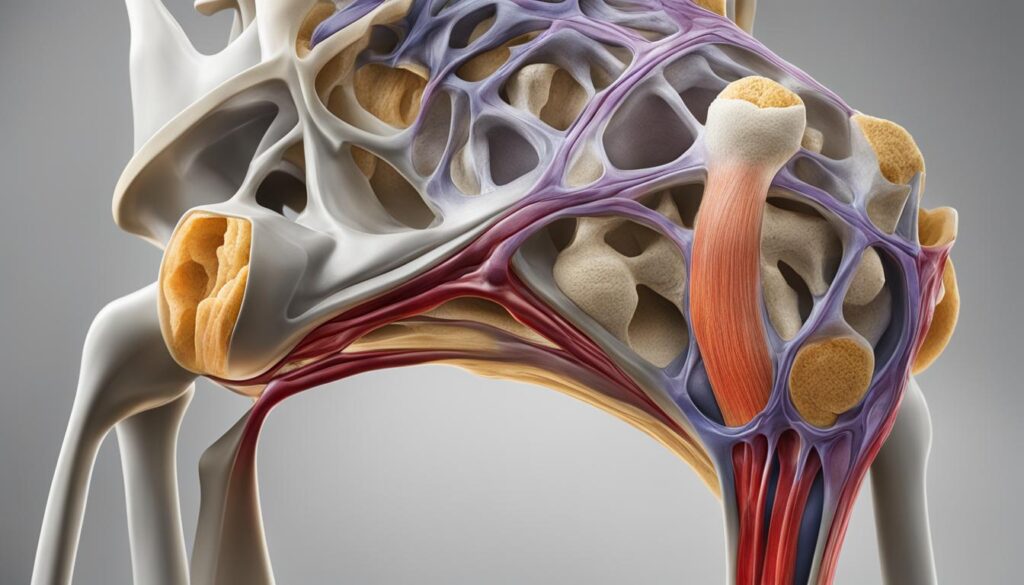
Hypermobile joints occur when the ligaments and joint capsules that hold the joints together are too loose, allowing for an extended range of motion. In most cases, hypermobile joints are benign and not accompanied by any other health conditions. The main causes of hypermobile joints include:
- Bone shape or the depth of the joint sockets
- Muscle tone or strength
- Proprioception
- A family history of hypermobility
Rarely, hypermobile joints can be a symptom of underlying conditions such as:
- Down syndrome
- Cleidocranial dysostosis
- Ehlers-Danlos syndrome
- Marfan syndrome
- Morquio syndrome
While most people with hypermobile joints do not require treatment, those experiencing pain or joint instability should seek medical attention. Treatment options may include:
- Pain relievers: Over-the-counter painkillers can help alleviate discomfort associated with hypermobile joints.
- Physical therapy: Targeted exercises and therapies can assist in strengthening the muscles around the joints, providing better stability.
- Protective measures: It is essential to protect the joints during physical activities to prevent further strain or injury.
By diligently following healthcare professionals’ advice and incorporating appropriate measures, individuals with hypermobile joints can effectively manage their symptoms and maintain a good quality of life.
Below is a table summarizing the causes and complications of hypermobile joints:
| Causes of Hypermobile Joints | Complications of Hypermobile Joints |
|---|---|
| Bone shape or joint socket depth | – |
| Muscle tone or strength | – |
| Proprioception | – |
| Family history of hypermobility | – |
| Down syndrome | – |
| Cleidocranial dysostosis | – |
| Ehlers-Danlos syndrome | – |
| Marfan syndrome | – |
| Morquio syndrome | – |

Symptoms and Diagnosis of Hypermobility Syndromes
Hypermobility can manifest in a variety of symptoms that often affect different parts of the body. These symptoms may include:
- Joint and muscle pain and stiffness
- Clicking joints
- Back and neck pain
- Fatigue
- Poor coordination
- Difficulty sensing joint position
- Joint dislocations
- Soft tissue injuries
- Easy bruising
- Stomach pain
- Bladder and bowel problems
- Dizziness
- Stretchy skin
Diagnosing hypermobility syndromes, such as Hypermobility Spectrum Disorder (HSD) or Hypermobile Ehlers-Danlos syndrome (hEDS), requires a thorough evaluation by a healthcare professional. The diagnostic process typically involves:
- A series of questions to assess symptoms and medical history
- An evaluation of family history to identify any potential genetic links
- A physical examination to assess joint mobility and stability
- Specific tests to determine pain levels and joint mobility
“Proper diagnosis is crucial for effectively managing symptoms and ruling out any underlying conditions.”
Seeking medical advice and guidance is essential for individuals experiencing symptoms of hypermobility. A healthcare professional can provide expert information and advice, as well as develop a personalized treatment plan based on individual needs.
In the next section, we will explore strategies and treatments for managing hypermobile joints effectively.
| Hypermobile Syndromes | Hypermobile Ehlers-Danlos Syndrome (hEDS) | Hypermobility Spectrum Disorder (HSD) |
|---|---|---|
| Symptoms | Pain and instability in joints, easy bruising, stretchy skin | Joint pain and instability, fatigue, muscle pain, gastrointestinal issues |
| Prevalence | Rare, affecting approximately 1 in 5,000 individuals | More common, affecting up to 10% of the population |
| Genetic Cause | Linked to gene mutations affecting collagen production | May have a genetic component but no specific gene mutations identified |
| Treatment | Physical therapy, joint protection strategies, pain management | Physical therapy, pain management, lifestyle modifications |
Managing Hypermobile Joints: Tips and Treatments
Effective management of hypermobile joints involves a combination of self-care measures and healthcare interventions. Here are some strategies to help you manage your hypermobile joints:
Exercise for Hypermobile Joints
Regular exercise plays a crucial role in strengthening the muscles around the joints and improving control. Low-impact activities like swimming and cycling are especially beneficial for hypermobile joints. Engaging in targeted exercises that focus on stability and joint support can help minimize pain and increase joint functionality.
Diet and Nutrition
Maintaining a healthy diet and weight is important for overall joint health. Consuming a balanced diet rich in antioxidants and nutrients can help reduce inflammation and promote joint health. Incorporate foods like fatty fish, leafy greens, and nuts into your diet to support joint function and minimize symptoms.
Footwear for Hypermobile Joints
Choosing supportive footwear is crucial for individuals with hypermobile joints. Opt for shoes with good arch support, cushioning, and stability. Consider using special insoles or orthotics to provide additional support and alleviate pain. Avoid high heels and unsupportive shoes that can exacerbate joint instability.
Pain Relief for Hypermobile Joints
There are various options for pain relief in hypermobile joints. Over-the-counter painkillers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate mild to moderate pain. Topical pain relief sprays or creams may provide temporary relief. If necessary, consult with a healthcare professional who can prescribe stronger pain medications.
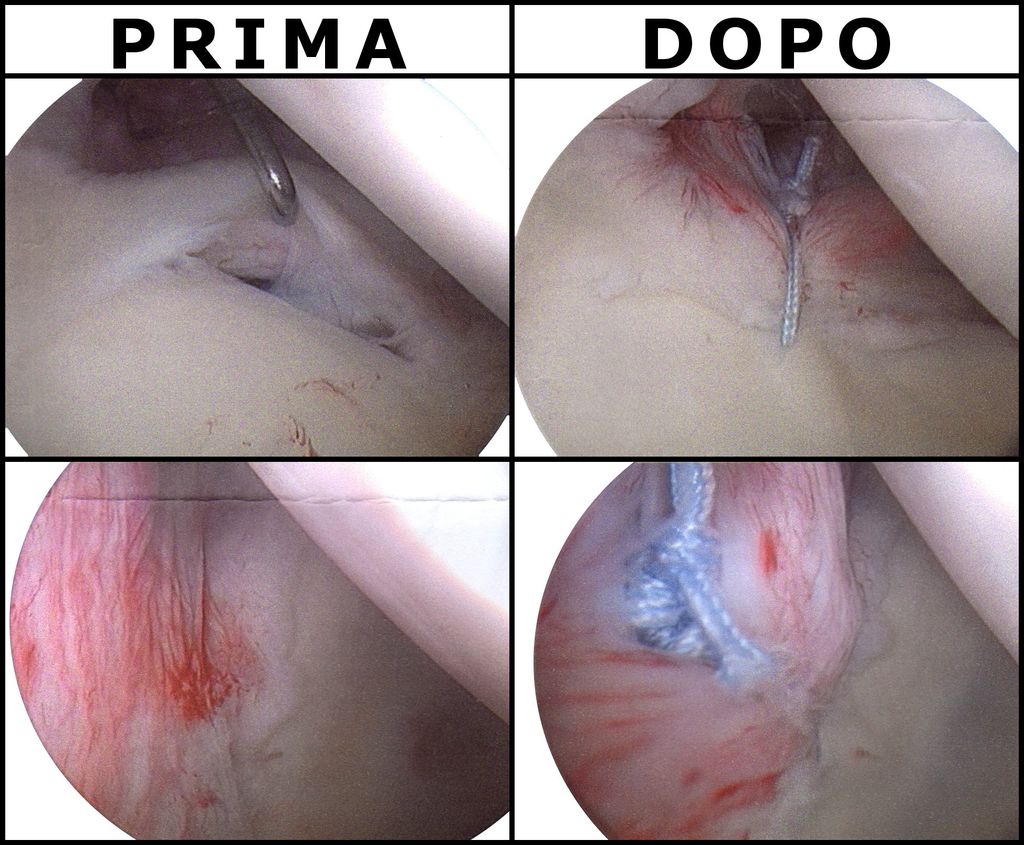
Physical Therapies for Hypermobile Joints
Physical therapies such as physiotherapy and hydrotherapy can be beneficial for individuals with hypermobile joints. These therapies focus on reducing pain, improving joint strength, and enhancing balance. A qualified therapist can create a personalized exercise program tailored to your specific needs and goals.
| Treatment | Benefits |
|---|---|
| Regular exercise | – Strengthen the muscles around the joints – Improve joint control – Reduce pain and stiffness |
| Diet and nutrition | – Support overall joint health – Reduce inflammation – Provide necessary nutrients for joint function |
| Footwear | – Provide stability and support – Alleviate pain and discomfort – Minimize joint instability |
| Pain relief | – Alleviate mild to moderate pain – Enhance daily comfort – Improve quality of life |
| Physical therapies | – Reduce pain and stiffness – Improve joint strength and stability – Enhance balance and coordination |
Working closely with healthcare professionals, including physiotherapists, occupational therapists, and orthopedic specialists, can guide you towards effective management strategies for your hypermobile joints. Prioritize joint protection during physical activities and follow the expert advice to optimize your joint health and overall well-being.

Conclusion
Managing hypermobile knees and joint hypermobility syndrome requires a comprehensive approach that focuses on protecting and strengthening the joints, reducing pain, and improving overall joint health. By implementing self-care measures such as regular exercise, maintaining a healthy weight, and wearing supportive footwear, individuals with hypermobile knees can enhance stability and reduce strain on the joints. Additionally, physical therapies, pain relief options, and occupational therapy can provide valuable support and guidance for managing symptoms and maintaining independence.
Although there is no cure for joint hypermobility syndrome, effective strategies can greatly enhance the quality of life and minimize the impact of symptoms. It is crucial to consult with healthcare professionals for proper diagnosis, personalized treatment plans, and ongoing management of hypermobile knees and joint hypermobility syndrome.
The key to successful management lies in a combination of self-care and professional intervention. Together, we can work towards minimizing pain, improving joint function, and optimizing overall well-being for individuals with hypermobile knees and joint hypermobility syndrome. By adopting a proactive approach and seeking appropriate support, those affected can achieve a higher quality of life and better manage the challenges associated with this condition.
FAQ
What is joint hypermobility syndrome?
Joint hypermobility syndrome refers to a condition characterized by very flexible joints that can cause pain, stiffness, and other symptoms. It is often diagnosed in children and young people and is usually not accompanied by any other underlying conditions.
What are the symptoms of joint hypermobility syndrome?
Common symptoms of joint hypermobility syndrome include fatigue, joint and muscle pain and stiffness, recurrent sprains and strains, joint dislocations, poor balance and coordination, thin and stretchy skin, and bladder or bowel problems.
How is joint hypermobility syndrome diagnosed?
Diagnosis is usually done by a GP who will use the Beighton scoring system to assess joint flexibility. The doctor may also examine the individual’s medical history and perform physical examinations to determine the severity of symptoms and rule out any underlying conditions.
What treatment options are available for joint hypermobility syndrome?
Treatment focuses on improving muscle strength and fitness to protect the joints. Options may include physiotherapy, occupational therapy, pain relief medications, and referrals to pain clinics for further management.
What causes hypermobile joints?
Hypermobile joints can be caused by factors such as bone shape or the depth of the joint sockets, muscle tone or strength, proprioception, and a family history of hypermobility. In rare cases, hypermobile joints can be a symptom of underlying conditions such as Down syndrome, cleidocranial dysostosis, Ehlers-Danlos syndrome, Marfan syndrome, or Morquio syndrome.
What are the complications of hypermobile joints?
While most people with hypermobile joints do not require treatment, those experiencing pain or joint instability should seek medical attention. Complications can include joint dislocations, soft tissue injuries, easy bruising, stomach pain, bladder and bowel problems, dizziness, and stretchy skin.
How are hypermobility syndromes diagnosed?
Diagnosis of hypermobility syndromes such as Hypermobility Spectrum Disorder (HSD) or Hypermobile Ehlers-Danlos syndrome (hEDS) is done by a doctor through a series of questions, family history assessment, physical examination, and tests to determine joint mobility and pain levels.
How can hypermobile joints be managed?
Managing hypermobile joints involves a combination of self-care measures and healthcare interventions. This may include regular exercise, maintaining a healthy diet and weight, wearing supportive footwear, practicing joint protection, and seeking physical therapy or occupational therapy for pain relief and strengthening of muscles around the joints.