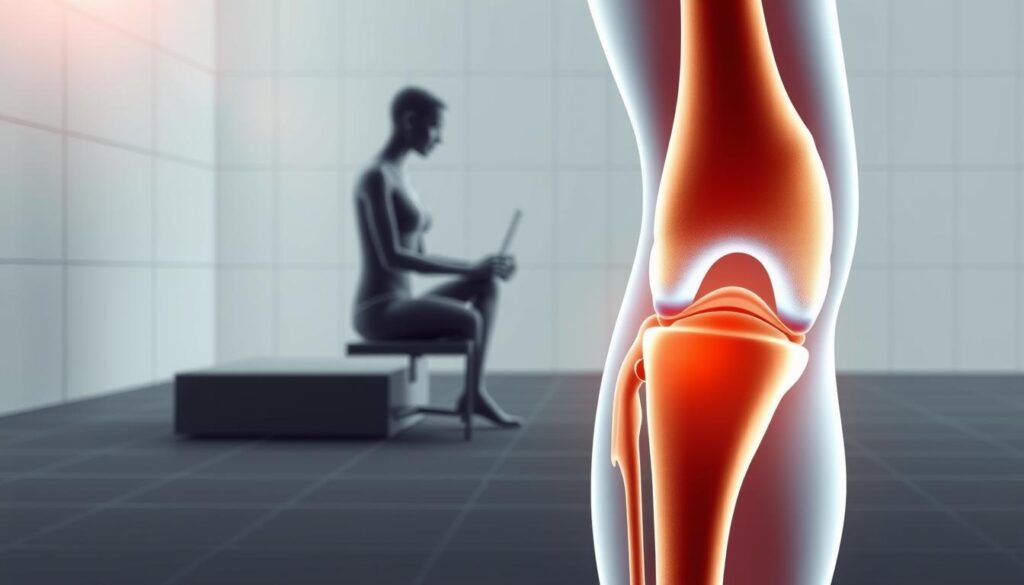
Have you ever wondered why some pain appears only during simple movements? For many, sitting feels comfortable, but rising from a chair triggers sharp stiffness or aching. This common issue often points to deeper challenges in how our joints and muscles work together.
Startup stiffness—a term linked to arthritis—is a key factor here. When standing, the body relies on proper alignment between the legs, hips, and feet. Weakness in the thigh muscles or poor chair design (like low seats or missing armrests) can strain the joints, making this motion harder over time.
Daily habits matter too. Prolonged sitting reduces blood flow to the legs, while repetitive motions wear down cartilage. Simple adjustments, such as using ice packs for 15 minutes a day or choosing supportive chairs, often provide relief. But when should these steps become a priority?
Key Takeaways
- Startup stiffness is often tied to arthritis or muscle weakness.
- Proper body alignment is critical when transitioning from sitting to standing.
- Chair design (e.g., armrests and seat height) impacts joint stress.
- Brief rest and ice therapy can reduce inflammation at home.
- Early intervention helps prevent long-term mobility issues.
Understanding Causes and Recognizing Symptoms
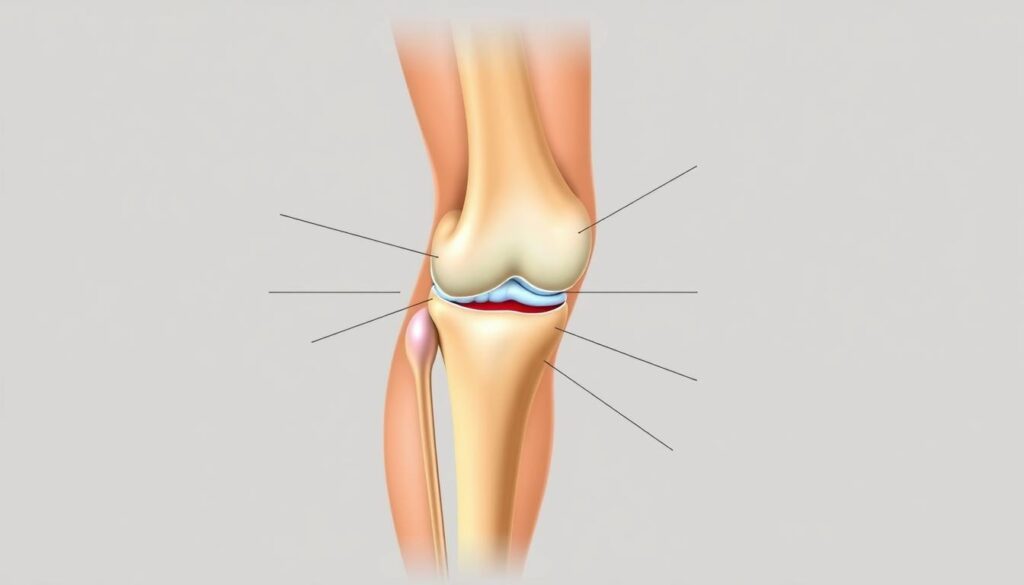
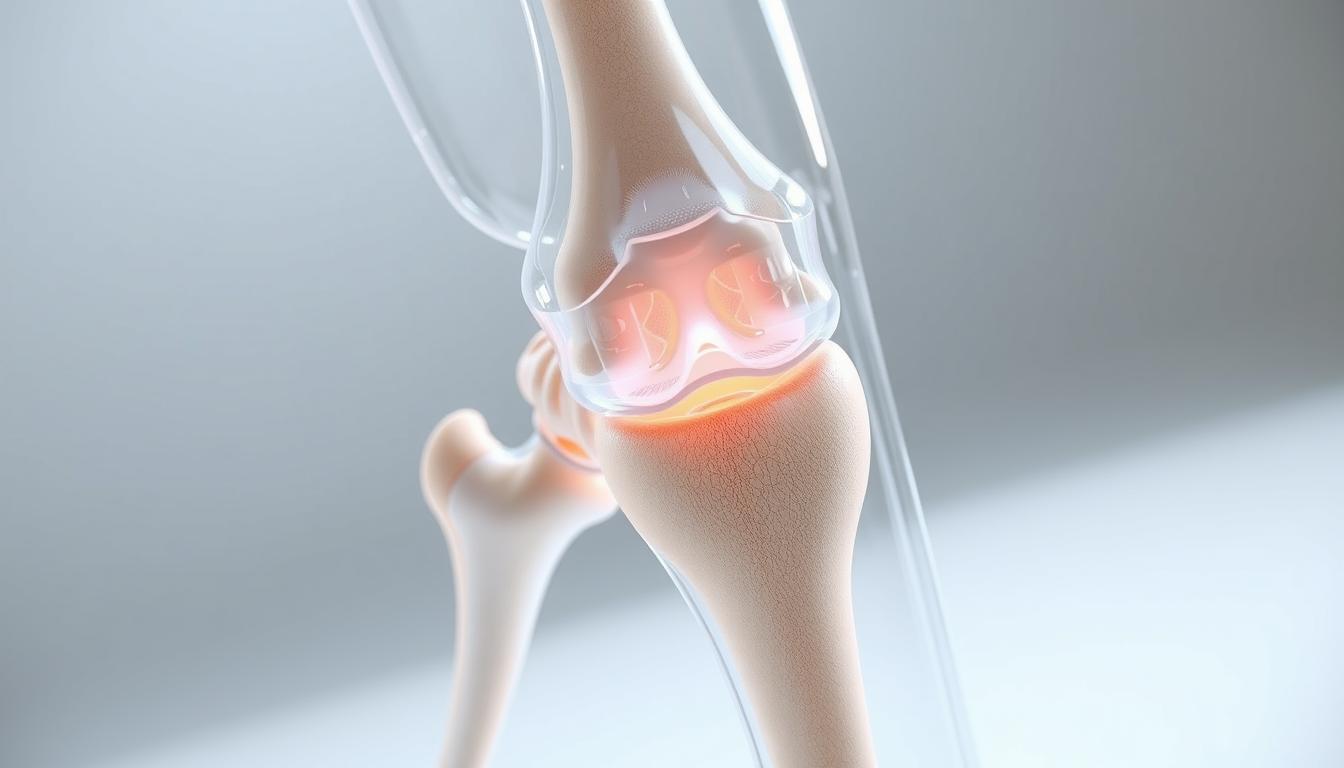
What makes certain motions trigger sharp joint sensations? For many, rising after sitting feels like a battle against stiffness or sudden aches. Two primary culprits often lie behind this struggle: arthritis and meniscal injuries.

Arthritis and Startup Stiffness
Arthritis wears down cartilage, leaving bones less protected. Morning stiffness or difficulty moving after rest—called “startup stiffness”—is common. Weak thigh muscles can’t compensate, making standing harder. Over time, this cycle reduces mobility and increases strain.
Meniscal Tears and Other Issues
Torn knee cartilage often causes locking or catching sensations. Unlike arthritis, these injuries may stem from sudden twists or prolonged sitting in awkward positions. Arthroscopic surgery repairs severe cases, but early detection through symptoms like swelling improves outcomes.
| Condition | Primary Symptoms | Common Triggers |
|---|---|---|
| Arthritis | Morning stiffness, reduced motion | Age, repetitive strain |
| Meniscal Tear | Sharp pain, joint locking | Twisting motions, deep squats |
Ignoring these signs risks long-term damage. Joint warmth or persistent swelling warrants medical evaluation. Simple changes—like avoiding low chairs—can ease pressure while addressing root causes.
Biomechanics of Standing Up and Muscle Involvement
Standing from a seated position seems simple, but it’s a complex dance between joints and muscles. Proper alignment ensures forces distribute evenly—weakness or poor mechanics shifts stress to vulnerable areas. This explains why some feel sharp sensations during routine motions.

Thigh Muscle Strength and Movement
The quadriceps and glutes act as primary engines during standing. Weak thigh muscles force the knee joint to absorb 50% more pressure, according to biomechanical research. Exercises like seated leg lifts or wall sits build endurance without straining tendons.
Patellofemoral pain syndrome—often called “runner’s knee”—worsens when these muscles fatigue. “Strength isn’t just about power; it’s about control,” notes a physical therapist. Proper engagement prevents the kneecap from grinding against bone during extension.
Chair Design and Body Mechanics
Seat height matters. Low chairs increase standing effort by 30%, while armrests reduce joint load by letting arms assist. Ideal seats align hips slightly above knees, keeping feet flat. Prolonged sitting in reclined positions tilts the pelvis, stressing ligaments.
| Chair Feature | Impact | Solution |
|---|---|---|
| Low Seat | Overworks quads | Add cushion |
| No Armrests | Shifts weight to legs | Use side table |
| Soft Cushion | Slumps posture | Firm support |
Even subtle adjustments, like foot placement shoulder-width apart, create stability. For those with arthritis, a higher seat combined with daily stretches can transform this daily challenge into a fluid motion.
Knee discomfort only when getting up from chair
Why does a simple act like standing become a source of sharp sensations? Identifying triggers requires observing patterns. Does the ache strike immediately after sitting for 20 minutes? Or does it flare when twisting slightly while rising? These clues help separate temporary strain from chronic issues.

Pressure on the kneecap often plays a central role. Activities requiring deep bends—like gardening or climbing stairs—can misalign the patella. Over time, this wears down cartilage, leading to patellofemoral pain syndrome. Early signs include clicking sounds or tenderness around the joint.
Movement Patterns Matter
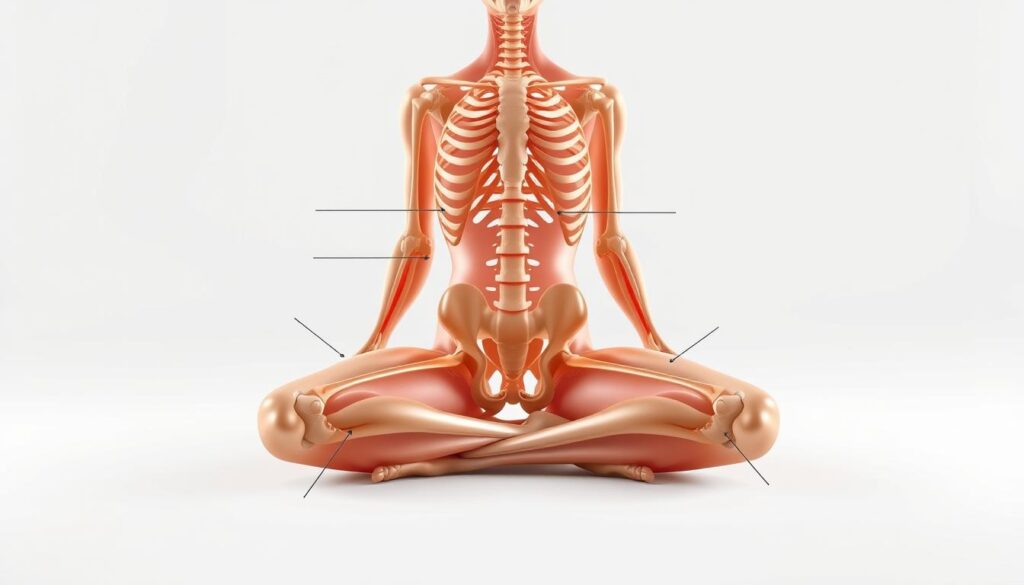
How you stand matters as much as how long you sit. Leaning too far back shifts 40% more weight onto the joints. Instead:
- Shift forward until your nose aligns with toes
- Push through heels, not toes
- Engage core muscles to stabilize hips
Immediate Actions vs. Long-Term Solutions
Applying ice for 15 minutes reduces inflammation quickly. But recurring stiffness may signal osteoarthritis or tendon weakness. Medical options like corticosteroid injections provide temporary relief, while targeted exercises rebuild strength. Severe cases might require surgery to repair damaged tissue.
| Trigger | Quick Fix | Long-Term Fix |
|---|---|---|
| Kneecap misalignment | Ice + rest | Quad-strengthening workouts |
| Arthritis flare-up | Heat therapy | Low-impact cardio |
| Muscle fatigue | Compression sleeve | Balance training |
Treatment Options, Exercises, and Prevention Strategies
Finding the right balance between self-care and medical support can transform mobility. While quick fixes ease immediate symptoms, lasting results often come from combining daily habits with professional guidance.
Everyday Adjustments for Lasting Relief
Heat therapy and ergonomic seating reduce strain during flare-ups. Chairs with firm lumbar support and armrests cut standing effort by 25%, according to ergonomic studies. For swelling, alternating ice packs with gentle stretches improves circulation.
Low-impact exercises build stability without stressing joints:
- Wall slides to strengthen quadriceps
- Water aerobics for resistance training
- Yoga poses like bridge lifts to engage glutes
When to Consider Advanced Care
Persistent symptoms may need targeted interventions. Corticosteroid injections temporarily calm inflammation, while physical therapy addresses muscle imbalances. “Surgery isn’t a first step—it’s a last resort,” explains Dr. Ellen Torres, orthopedic specialist.
| Treatment | Purpose | Best For |
|---|---|---|
| Corticosteroid Injections | Reduce swelling | Acute arthritis flares |
| Physical Therapy | Improve mobility | Post-injury recovery |
| Knee Replacement | Restore function | Severe cartilage loss |
Prevention starts with small changes. Maintaining healthy weight cuts joint pressure by 4 pounds per pound lost. Supportive footwear and avoiding prolonged sitting complete the picture—empowering you to rise with confidence.
Conclusion
Addressing joint challenges requires a blend of awareness and action. Arthritis-related stiffness and muscle imbalances often lie at the root of recurring issues. Simple daily habits—like applying ice therapy for 15 minutes or choosing chairs with proper support—can ease strain on the kneecap and surrounding tissues.
For many, combining home care with professional guidance yields the best results. Targeted exercises rebuild strength in weak areas, while corticosteroid injections manage severe swelling. In persistent cases, surgical options like knee replacement restore mobility when conservative methods fall short.
Body mechanics play a pivotal role. Adjusting seat height, engaging core muscles during standing, and avoiding prolonged sitting all reduce pressure on the knee joint. These changes, paired with early medical consultation, help prevent minor aches from becoming chronic problems.
Whether managing patellofemoral syndrome or recovering from injury, personalized plans matter. We encourage exploring solutions that align with your lifestyle and seeking expert advice to maintain long-term joint health.
FAQ
What causes sharp front-of-knee pain when rising from a seated position?
We often see this linked to patellofemoral pain syndrome (runner’s knee) or early-stage osteoarthritis. Weak thigh muscles, improper tracking of the kneecap, or cartilage wear can strain the joint during standing motions. Swelling or stiffness after long periods of sitting may also signal inflammation.
How does chair height impact knee stress during standing?
Low chairs force your hips below knee level, increasing pressure on the patellar tendon. We recommend chairs with seat heights matching your lower leg length. Armrests help redistribute weight, reducing strain on the quadriceps and joints when pushing up.
Can daily exercises prevent discomfort when getting up?
Yes. Strengthening exercises like straight-leg raises and step-ups build quadriceps endurance, while stretches for hamstrings and IT bands improve flexibility. Consistency matters—aim for 10–15 minutes of targeted movements 3–4 times weekly to support joint stability.
When should someone consider medical interventions for this issue?
If pain persists despite rest, ice, or over-the-counter anti-inflammatories, consult a specialist. Persistent swelling, grinding sensations, or difficulty bearing weight may indicate meniscal tears or advanced arthritis. Options like corticosteroid injections or arthroscopic surgery are explored if conservative treatments fail.
Are there lifestyle changes that reduce strain on knees during daily activities?
Absolutely. Maintaining a healthy weight lowers pressure on joints. Avoid sitting cross-legged or in deep sofas for extended periods. Use ergonomic furniture, and take short walks hourly if desk-bound. Supportive footwear with cushioned soles also minimizes impact during transitions from sitting to standing.
Does osteoarthritis always lead to knee replacement surgery?
No. Many manage symptoms for years with physical therapy, weight management, and anti-inflammatory medications. Surgery becomes an option only when cartilage loss severely limits mobility or causes unrelenting pain. Early diagnosis and proactive care often delay or prevent the need for joint replacement.