Living with knee pain can significantly impact your daily activities, from climbing stairs to simply sitting for extended periods. If you’ve been diagnosed with Patellofemoral Pain Syndrome (PFPS) and are seeking relief without surgery, you’re in the right place. This comprehensive guide explores effective non-surgical approaches that can help you manage pain, improve function, and return to the activities you love.
Understanding Patellofemoral Pain Syndrome
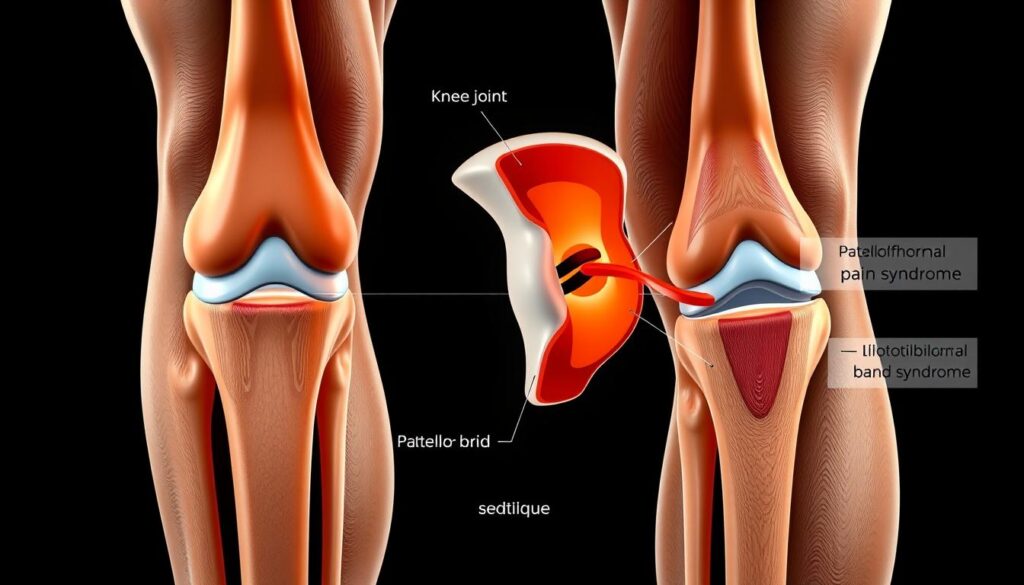
The patellofemoral joint and surrounding structures involved in PFPS
Patellofemoral pain syndrome, often called “runner’s knee,” is characterized by pain around or behind the kneecap (patella). This condition occurs when the patella doesn’t track properly in the groove of the thigh bone (femur), creating stress on the joint and surrounding tissues. PFPS affects approximately one-quarter of adults and one-third of adolescents, with a higher prevalence in women.
Common Causes of PFPS
- Overuse from repetitive activities like running or squatting
- Muscle imbalances, particularly weak quadriceps or hip muscles
- Poor flexibility in the hamstrings, quadriceps, or iliotibial band
- Anatomical factors such as a high-riding kneecap or shallow femoral groove
- Improper footwear or training techniques
- Lower extremity malalignment affecting knee mechanics
- Sudden increases in physical activity or training intensity
- Previous knee injuries or surgeries
- Tight lateral structures (lateral retinaculum and iliotibial band)
- Direct trauma to the knee
Recognizing PFPS Symptoms
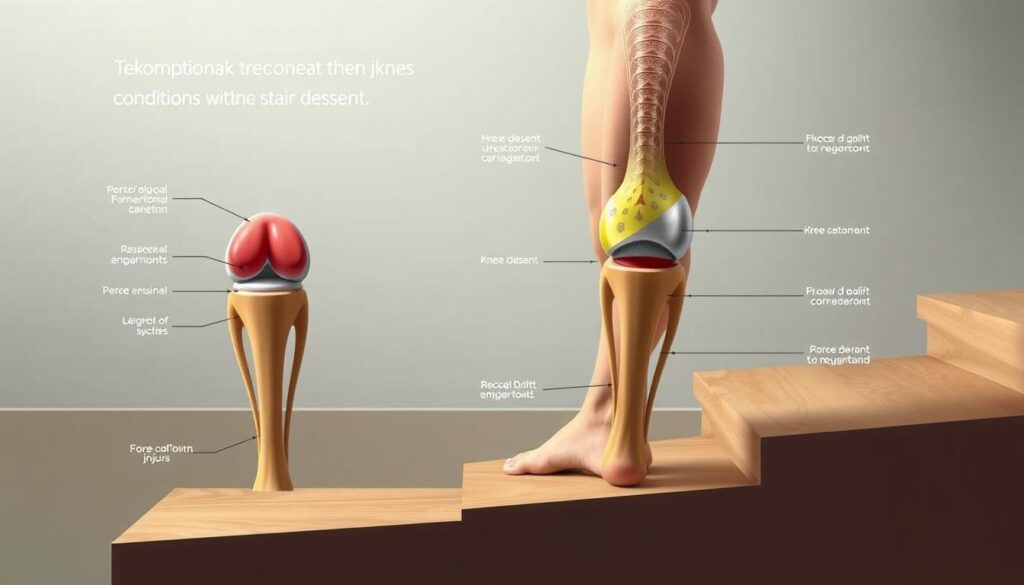
The hallmark symptom of PFPS is a dull, aching pain around or behind the kneecap. This pain typically worsens with activities that increase pressure on the patellofemoral joint, such as:
- Climbing or descending stairs
- Squatting or kneeling
- Running, especially downhill
- Sitting with knees bent for extended periods (the “theater sign”)
- Standing up after prolonged sitting
You may also experience a sensation of your knee “giving way,” popping or cracking sounds, or stiffness after periods of inactivity. Unlike some other knee conditions, PFPS rarely causes significant swelling.
Diagnosing Patellofemoral Pain Syndrome
Before exploring treatment options, it’s important to understand how PFPS is diagnosed. Most cases can be identified through a thorough clinical examination without the need for extensive imaging.
Clinical Examination
Your healthcare provider will likely perform several tests to assess your knee function and identify the source of your pain:
- Patellar tracking assessment: Observing how your kneecap moves during knee flexion and extension
- Patellar glide test: Evaluating the mobility of your kneecap
- Patellar tilt test: Checking for tightness in lateral structures
- Patellar grind test: Applying pressure to the kneecap while moving the knee
- Muscle strength and flexibility testing: Assessing quadriceps, hamstrings, and hip muscles
When Imaging Is Necessary
While most PFPS cases don’t require imaging, your doctor may recommend X-rays, MRI, or CT scans in certain situations:
- History of trauma or previous knee surgery
- Presence of joint effusion (swelling)
- Symptoms that don’t improve with standard treatment
- To rule out other conditions like osteoarthritis or loose bodies
Effective Non-Surgical Treatment Approaches
The good news is that most cases of patellofemoral pain syndrome respond well to non-surgical interventions. A comprehensive treatment plan typically includes several components working together to reduce pain and improve function.
The RICE Method: First-Line Treatment

The RICE method is an effective initial approach for managing PFPS symptoms
For acute pain flare-ups, the RICE method is often recommended as an initial approach:
- Rest: Temporarily reduce activities that aggravate your symptoms
- Ice: Apply cold packs to your knee for 15-20 minutes every 2-3 hours
- Compression: Use a knee sleeve or wrap to provide support
- Elevation: Keep your knee elevated above heart level when possible
Pro Tip: When applying ice, always use a thin towel between the ice pack and your skin to prevent tissue damage. Never apply ice directly to your skin.
Physical Therapy: The Cornerstone of PFPS Treatment
Physical therapy is considered the most effective non-surgical treatment for patellofemoral pain syndrome. A well-designed rehabilitation program focuses on correcting muscle imbalances, improving flexibility, and optimizing patellar tracking.
Key Physical Therapy Exercises for PFPS
Quadriceps Strengthening

Straight Leg Raises: Lie on your back with one leg bent and the other straight. Tighten the quadriceps of your straight leg and slowly raise it to the height of your opposite knee. Hold for 5 seconds, then lower. Perform 3 sets of 10-15 repetitions daily.
Hip Stabilizer Strengthening

Clamshells: Lie on your side with knees bent and feet together. Keep your feet touching while raising your top knee. Hold for 2 seconds, then lower. Perform 3 sets of 15-20 repetitions on each side daily to strengthen hip external rotators.
VMO Activation
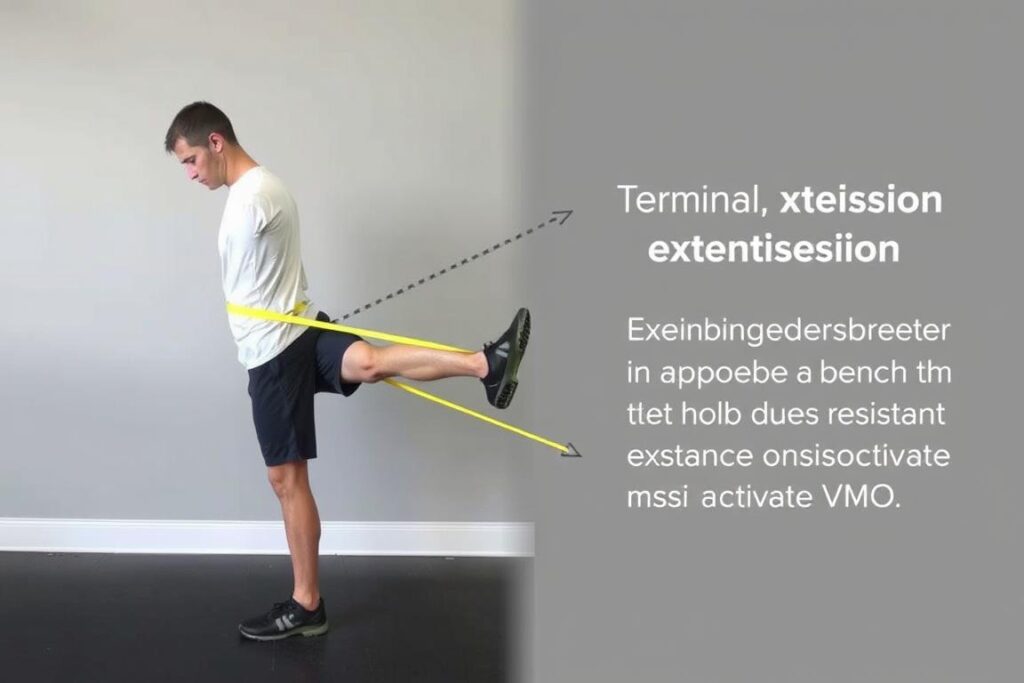
Terminal Knee Extensions: Attach a resistance band to a fixed object and loop around your knee. Stand facing away from the anchor point with slight knee bend. Straighten your knee against the resistance, focusing on the last 30 degrees of extension. Perform 3 sets of 15 repetitions daily.
Stretching Exercises for PFPS
Quadriceps Stretch

Stand holding onto a support with one hand. Grasp your ankle with the other hand and gently pull your heel toward your buttocks. Keep your knees close together and maintain an upright posture. Hold for 30 seconds and repeat 3 times on each leg.
IT Band Stretch

Stand with your right leg crossed behind your left. Extend your right arm overhead and lean to the left, feeling a stretch along the outside of your right hip and thigh. Hold for 30 seconds and repeat 3 times on each side to reduce tension on the lateral knee structures.
Orthotic Interventions for PFPS
Orthotic devices can play a supportive role in managing patellofemoral pain syndrome by improving alignment and reducing stress on the knee joint.

Knee Braces and Sleeves
Knee braces and sleeves provide external support to help stabilize the patella and reduce pain during activity. Options include:
- Patellar stabilizing braces: Feature a hole or buttress around the kneecap to help maintain proper tracking
- Knee sleeves: Provide compression and warmth that may help reduce pain
- Patellar straps: Apply pressure on the patellar tendon to alter forces across the joint
Research suggests that while bracing alone may provide symptomatic relief, it’s most effective when used as part of a comprehensive treatment program that includes physical therapy.
Foot Orthotics
Custom or over-the-counter foot orthotics can help correct biomechanical issues that contribute to PFPS:
- Provide arch support to reduce excessive pronation
- Improve lower limb alignment during walking and running
- Reduce stress on the knee joint by optimizing foot mechanics
Patellar Taping
Kinesiology tape or specialized patellar taping techniques may help:
- Guide proper patellar tracking during movement
- Provide sensory feedback to improve muscle activation
- Reduce pain during activities
While evidence for taping is mixed, many patients report symptomatic improvement, particularly during the early phases of rehabilitation.
Pain Management Techniques
Managing pain effectively is an important component of PFPS treatment, allowing you to participate more comfortably in rehabilitation exercises and daily activities.
Medication Options

Over-the-counter medications can help manage pain and inflammation:
- NSAIDs (Nonsteroidal anti-inflammatory drugs): Medications like ibuprofen and naproxen can reduce both pain and inflammation
- Acetaminophen: Helps with pain relief but doesn’t address inflammation
Always follow dosage instructions and consult with your healthcare provider before starting any medication regimen, especially if you have other health conditions or take other medications.
Topical Treatments
Topical pain relievers can be applied directly to the knee area:
- Menthol or capsaicin creams: Create cooling or warming sensations that can help mask pain
- Topical NSAIDs: Provide localized anti-inflammatory effects with fewer systemic side effects
- CBD-infused topicals: Some patients report benefits, though research is still emerging
Cold and Heat Therapy
Alternating between cold and heat can help manage symptoms:
- Cold therapy: Best for acute pain and after activity to reduce inflammation
- Heat therapy: Helpful before exercise to increase blood flow and tissue elasticity
- Contrast therapy: Alternating between cold and heat can stimulate circulation and pain relief
Activity Modification Strategies
Adjusting your activities is crucial for allowing healing while maintaining fitness and function.

Temporary Activity Adjustments
During the acute phase of PFPS, consider these modifications:
- Reduce activities that aggravate symptoms (deep squats, lunges, stair climbing)
- Decrease running mileage or intensity if running is a trigger
- Avoid sitting with knees bent for prolonged periods
- Use stairs one at a time if necessary
Low-Impact Alternatives
Maintain fitness with activities that place less stress on the patellofemoral joint:
- Swimming: Provides excellent cardiovascular exercise with minimal joint loading
- Stationary cycling: Low-impact exercise that can strengthen quadriceps (adjust seat height to avoid deep knee flexion)
- Elliptical training: Offers a running-like motion without the impact
- Water aerobics: Utilizes water resistance while reducing joint stress
Gradual Return to Activities
As symptoms improve, follow these guidelines for returning to regular activities:
- Increase activity duration and intensity by no more than 10% per week
- Monitor symptoms during and after activity
- Incorporate proper warm-up and cool-down routines
- Continue maintenance exercises even after symptoms resolve
Comparing Treatment Effectiveness
Research has evaluated various non-surgical approaches for PFPS. The following table summarizes the evidence for different treatment options:
| Treatment Approach | Evidence Level | Effectiveness | Time to Results | Best For |
| Physical Therapy (Quadriceps Strengthening) | Strong | High | 4-8 weeks | Most PFPS cases |
| Hip Strengthening Exercises | Strong | High | 6-12 weeks | Cases with hip weakness |
| Patellar Taping | Moderate | Moderate | Immediate (temporary) | Short-term pain relief |
| Knee Bracing | Moderate | Moderate | Immediate | Activity-specific support |
| Foot Orthotics | Moderate | Moderate | 2-4 weeks | Cases with foot pronation |
| NSAIDs | Moderate | Moderate (for pain) | Hours to days | Short-term pain management |
| Activity Modification | Moderate | High | 1-2 weeks | Acute pain reduction |
Expert Insights on PFPS Management
“The most successful non-surgical treatment for patellofemoral pain syndrome is a comprehensive approach that addresses all contributing factors. Physical therapy focusing on both quadriceps and hip strengthening has shown the best long-term outcomes in clinical studies.”
“Many patients expect immediate results, but patience is key with PFPS treatment. Consistent adherence to a rehabilitation program typically shows significant improvement within 6-12 weeks, though some cases may take longer. The good news is that most patients can avoid surgery with proper conservative management.”
“I emphasize to my patients that addressing biomechanical issues is crucial for long-term success. This means not just treating the symptoms but correcting movement patterns, strengthening weak muscles, and improving flexibility in tight structures. This comprehensive approach prevents recurrence, which is common with PFPS.”
Case Study: Successful Non-Surgical Recovery
Sarah’s Journey: From Sidelined Runner to Marathon Finisher

Patient Profile: Sarah, 34-year-old recreational runner training for her first half marathon
Symptoms: Developed anterior knee pain after increasing weekly mileage by 50%. Pain worsened when running downhill and climbing stairs. Experienced the “theater sign” with pain after sitting through a movie.
Diagnosis: Clinical examination revealed patellofemoral pain syndrome with weak hip abductors and tight iliotibial band.
Treatment Approach:
- Weeks 1-2: RICE protocol, activity modification (reduced running by 50%, avoided hills), and began basic physical therapy
- Weeks 3-6: Progressive strengthening of quadriceps and hip muscles, flexibility work, and gait analysis with running form correction
- Weeks 7-10: Gradual return to running with proper footwear and custom orthotics, continued strengthening exercises
- Weeks 11-16: Progressive increase in running distance with maintenance exercises
Outcome: Sarah completed her half marathon six months after beginning treatment, with no return of symptoms. She continues maintenance exercises twice weekly and uses proper warm-up techniques before runs.
Key Takeaway: A comprehensive, patient-specific approach addressing all contributing factors led to complete recovery without surgical intervention.
Frequently Asked Questions
How long does recovery from patellofemoral pain syndrome typically take?
Recovery time varies depending on the severity of symptoms, adherence to treatment, and individual factors. Most patients see significant improvement within 4-12 weeks of consistent treatment. Complete resolution may take 3-6 months in some cases. Continuing maintenance exercises even after symptoms resolve is important for preventing recurrence.
When is surgery considered for patellofemoral pain syndrome?
Surgery is rarely necessary for PFPS and is typically only considered when:
- Conservative treatment has been consistently applied for at least 6-12 months without improvement
- There is clear structural damage or anatomical abnormality contributing to symptoms
- Pain significantly limits daily activities despite comprehensive non-surgical management
- Diagnostic imaging confirms a specific issue that would benefit from surgical correction
Less than 15% of PFPS cases ultimately require surgical intervention. Always exhaust all non-surgical options first.
Can I continue exercising with patellofemoral pain syndrome?
Yes, but modifications are usually necessary. The key principle is to stay active without aggravating symptoms. This typically means:
- Switching to lower-impact activities temporarily (swimming, cycling)
- Reducing intensity and duration of problematic activities
- Ensuring proper form during exercise
- Incorporating appropriate warm-up and cool-down routines
Work with your healthcare provider or physical therapist to develop an appropriate exercise plan that allows for continued activity while promoting healing.
Will my patellofemoral pain syndrome come back after treatment?
Recurrence is possible, especially if underlying contributing factors aren’t fully addressed or if maintenance exercises are discontinued. Studies show that approximately 25-30% of patients experience some recurrence of symptoms. To minimize this risk:
- Continue maintenance exercises even after symptoms resolve
- Gradually increase activity levels when returning to sports
- Maintain proper biomechanics during activities
- Use appropriate footwear and replace shoes when worn
- Address any new pain promptly rather than pushing through it
Moving Forward: Your Path to Recovery
Patellofemoral pain syndrome can be frustrating, but with the right approach, most people achieve significant improvement without surgery. The key to success lies in a comprehensive treatment plan that addresses all contributing factors, from muscle imbalances to activity modifications.
Remember that consistency is crucial—stick with your exercises, follow your healthcare provider’s recommendations, and be patient with the recovery process. By taking a proactive approach to managing your PFPS, you can return to the activities you love with less pain and better function.
Key Takeaways:
- Physical therapy focusing on quadriceps and hip strengthening is the cornerstone of effective PFPS treatment
- A multi-faceted approach including activity modification, proper footwear, and possibly orthotics yields the best results
- Patience and consistency with your treatment plan are essential for long-term success
- Most people with PFPS can achieve significant improvement without surgical intervention
Experiencing Knee Pain?
Don’t let patellofemoral pain limit your activities. Our specialists can help determine the exact cause of your symptoms and create a personalized treatment plan.
Need Expert Guidance for Your PFPS Exercises?
Our physical therapists specialize in creating customized exercise programs for patellofemoral pain syndrome. Get a personalized plan designed for your specific needs.
Ready to Start Your Recovery Journey?
Our team of specialists can help you develop a comprehensive plan to address your patellofemoral pain syndrome without surgery.
Take the First Step Toward Pain-Free Movement
Our team specializes in non-surgical treatment of patellofemoral pain syndrome. Contact us today to schedule a comprehensive evaluation and start your personalized recovery plan.