Knee pain can be a common issue, especially as we age or engage in physical activities. Understanding the anatomy of the knee and the causes of knee pain can help us address and manage discomfort. In this article, we will explore effective exercises and lifestyle modifications that can help soothe sore knees and promote knee health.
Key Takeaways
- Perform low-impact aerobic exercises such as swimming or cycling to strengthen the muscles around the knee without adding stress.
- Incorporate strength training exercises to improve knee stability and support.
- Engage in flexibility and range of motion exercises to maintain joint mobility and reduce stiffness.
- Maintain a healthy weight through proper nutrition and regular exercise to reduce pressure on the knees.
- Wear appropriate footwear and consider orthotics to provide proper support and alignment for the knees.
Understanding Knee Anatomy

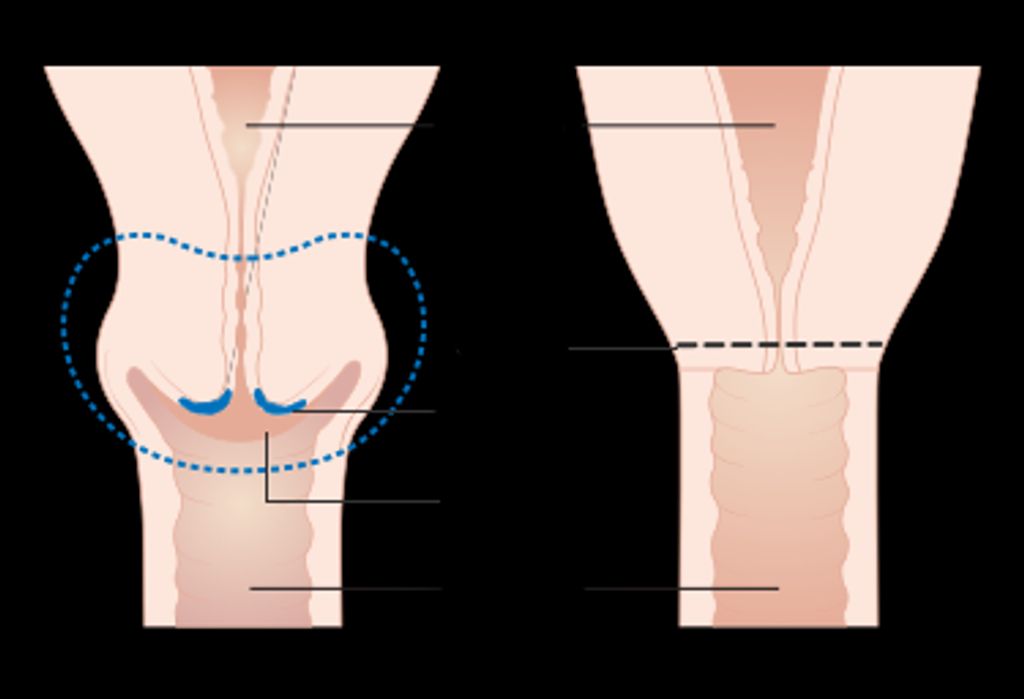
Structure of the knee joint
The knee joint is a complex structure that plays a crucial role in our mobility and stability. It consists of several components, including the femur, tibia, and patella. These bones are connected by strong ligaments that provide support and stability. Additionally, the knee joint is cushioned by a layer of cartilage that helps to reduce friction and absorb shock during movement. Understanding the intricate anatomy of the knee joint is essential for addressing and preventing knee pain and injuries.
| Component | Function |
|---|---|
| Femur | Articulates with tibia |
| Tibia | Supports body weight |
| Patella | Protects knee joint |
Functions of the knee ligaments
We often overlook the critical role that the ligaments of the knee play in our daily activities. These fibrous bands are essential for stabilizing the knee joint, enabling us to walk, run, and jump with confidence. The primary ligaments in the knee include the Anterior Cruciate Ligament (ACL), Posterior Cruciate Ligament (PCL), Medial Collateral Ligament (MCL), and Lateral Collateral Ligament (LCL).
Each ligament has a specific function:
- The ACL prevents the tibia from sliding out in front of the femur and provides rotational stability.
- The PCL prevents the tibia from sliding backward under the femur.
- The MCL resists forces that would push the knee inward.
- The LCL resists forces that would push the knee outward.
It’s crucial to maintain the strength and flexibility of these ligaments to prevent injury. A sudden twist or turn can strain or tear a ligament, leading to pain and instability. Regular exercise and proper technique during physical activities can help protect these vital structures.
Tip: Always warm up before engaging in sports or high-impact activities to prepare your knee ligaments for the stress ahead.
Importance of knee cartilage
We often overlook the critical role that cartilage plays in the overall health and function of our knees. This resilient, rubbery tissue serves as a shock absorber, reducing the impact on our joints as we move. Without the cushioning effect of cartilage, our bones would rub against each other, leading to pain and inflammation.
Cartilage also enables smooth joint movement, allowing us to perform a wide range of activities with ease. Unfortunately, once damaged, cartilage does not heal easily due to its lack of blood supply. This is why we emphasize the importance of protecting our knee cartilage through preventive measures and exercises.
Remember, maintaining healthy knee cartilage is not just about avoiding injury; it’s also about preserving mobility and quality of life as we age. Engaging in low-impact exercises and maintaining a healthy weight can significantly contribute to the longevity of our knee cartilage.
Common Causes of Knee Pain

Degenerative joint diseases
Degenerative joint diseases, such as osteoarthritis, are a common cause of knee pain. Inflammation and gradual wear and tear of the cartilage are key factors in these conditions. It’s important to understand the impact of these diseases on knee function and mobility. Here’s a brief overview of the prevalence of degenerative joint diseases in the population:
| Disease | Prevalence |
|---|---|
| Osteoarthritis | 27 million affected individuals |
| Rheumatoid Arthritis | 1.3 million affected individuals |
These numbers highlight the widespread nature of degenerative joint diseases and emphasize the need for effective management strategies. Maintaining a healthy weight and engaging in appropriate exercises can help alleviate the symptoms and slow the progression of these conditions. As a first step, it’s crucial to recognize the impact of degenerative joint diseases on knee health and take proactive measures to address them.
Injuries and trauma
Injuries and trauma are common causes of knee pain. Traumatic injuries such as fractures, dislocations, and ligament tears can result in acute knee pain. Overuse injuries from repetitive stress or strain can lead to chronic knee pain. It’s important to seek medical attention for any knee injury to prevent further damage and promote proper healing. Additionally, implementing proper rehabilitation exercises and techniques can aid in the recovery process.
Overuse and repetitive stress
Overuse and repetitive stress on the knee joint can lead to chronic pain and discomfort. This type of stress is often the result of repetitive movements or activities that put excessive strain on the knee, such as prolonged standing or frequent bending. Maintaining proper form and using supportive footwear can help reduce the impact of repetitive stress on the knees. Additionally, incorporating regular rest periods and gentle stretching into daily routines can alleviate the strain caused by overuse. It’s important to be mindful of our daily activities and make adjustments to prevent overuse and repetitive stress on the knees.
Effective Exercises for Knee Pain Relief

Low-impact aerobic exercises
After incorporating low-impact aerobic exercises into our routine, we can further enhance knee stability and strength through targeted strength training. This includes exercises that focus on the quadriceps, hamstrings, and calf muscles. Additionally, flexibility and range of motion exercises are crucial for maintaining joint mobility and preventing stiffness. Here’s a brief overview of the recommended exercises:
| Exercise Type | Description |
|---|---|
| Quadriceps Strengthening | Straight leg raises, wall sits |
| Hamstring Strengthening | Hamstring curls, bridges |
| Calf Strengthening | Calf raises, heel drops |
It’s important to start with light weights and gradually increase resistance to avoid strain and injury. Remember to consult a healthcare professional before starting any new exercise program.
Strength training for knee stability
We understand that maintaining knee stability is crucial for overall joint health. Strength training exercises specifically target the muscles surrounding the knee, such as the quadriceps, hamstrings, and calf muscles. By strengthening these key muscle groups, we can provide better support for the knee joint and potentially reduce the risk of injury.
Consistency is key when incorporating strength training into your routine. We recommend starting with exercises that do not overload the knee. For example:
- Leg presses with a light weight
- Seated or lying leg curls
- Step-ups using a low platform
As you progress, gradually increase the intensity and weight to continue challenging your muscles while still prioritizing safety.
Tip: Always listen to your body and avoid any exercises that cause pain beyond normal muscle fatigue. It’s essential to differentiate between the discomfort of a workout and the pain that can signal harm to the knee.
Remember, while strength training is beneficial, it should be balanced with other forms of exercise and lifestyle modifications for optimal knee health.
Flexibility and range of motion exercises
After completing the low-impact aerobic exercises and strength training for knee stability, flexibility and range of motion exercises are crucial for maintaining joint mobility and preventing stiffness. These exercises focus on improving the flexibility of the muscles and tendons around the knee joint, enhancing the range of motion and reducing the risk of injury.
It’s important to perform these exercises with proper form and technique to maximize their benefits. Here’s a simple table summarizing the recommended flexibility and range of motion exercises:
| Exercise Type | Description |
|---|---|
| Quadriceps Stretch | Standing or lying down, holding onto a support |
| Hamstring Stretch | Seated or standing, reaching for toes |
| Calf Stretch | Using a wall or step to stretch the calf muscles |
| Knee Flexion and Extension | Sitting or lying down, bending and straightening |
Remember to consult a healthcare professional before starting any new exercise routine, especially if you have existing knee issues or concerns about your knee health.
Lifestyle Modifications for Knee Health

Nutrition and weight management
Nutrition and weight management play a crucial role in maintaining healthy knees. Balanced nutrition supports the repair and maintenance of knee tissues, while weight management reduces the load on the knee joint, alleviating stress and strain. It’s important to focus on a diet rich in antioxidants, omega-3 fatty acids, and vitamin D to promote joint health.
When it comes to weight management, maintaining a healthy body weight can significantly reduce the risk of knee pain and injury. Here’s a simple table to illustrate the recommended body mass index (BMI) ranges for optimal knee health:
| BMI Range | Health Status |
|---|---|
| 18.5-24.9 | Normal Weight |
| 25-29.9 | Overweight |
| 30 or above | Obese |
In addition to nutrition and weight management, proper footwear and orthotics are essential for providing adequate support and alignment for the knees. Posture and body mechanics also play a significant role in knee health. Remember to maintain good posture and practice proper body mechanics to reduce the risk of knee strain and injury.
Tip: When choosing footwear, look for shoes with good arch support and cushioning to minimize impact on the knees during physical activities.
Proper footwear and orthotics
We often underestimate the impact that our footwear can have on knee health. The right shoes can provide the necessary support to alleviate stress on the knee joint, while the wrong ones can exacerbate pain and lead to further injury. Orthotics, or custom insoles, can be particularly beneficial for those with specific foot conditions that affect knee alignment and function.
When selecting footwear, consider the following points:
- Ensure the shoes offer adequate cushioning and support for the arches of your feet.
- Look for a comfortable fit that doesn’t pinch or restrict movement.
- Consider the activity you’ll be using them for; different activities require different types of support.
Tip: Regularly replace your shoes, especially if you lead an active lifestyle, to maintain optimal support and cushioning.
Orthotics should be chosen with care and, ideally, with the guidance of a healthcare professional. They can correct abnormal walking patterns, distribute weight more evenly, and reduce the strain on your knees.
Posture and body mechanics
When it comes to maintaining good posture and body mechanics, awareness and conscious effort are key. We must be mindful of our body alignment and movement patterns throughout the day. This includes sitting, standing, and walking. Additionally, incorporating ergonomic adjustments in our work and home environments can greatly benefit our knee health. For example, using a supportive chair with proper lumbar support and adjusting the height of our computer monitor to eye level can help reduce strain on the knees and promote better posture. It’s important to remember that small changes in our daily habits can have a significant impact on our knee health and overall well-being.
Conclusion
In conclusion, the exercises outlined in this article offer a comprehensive approach to soothing sore knees. By incorporating these exercises into your daily routine, you can significantly improve knee strength and flexibility, leading to reduced discomfort and enhanced mobility. Remember to consult with a healthcare professional before beginning any new exercise regimen, especially if you have pre-existing knee conditions. With dedication and consistency, you can take proactive steps to support your knee health and overall well-being.
Frequently Asked Questions
What are the best low-impact aerobic exercises for knee pain relief?
Some of the best low-impact aerobic exercises for knee pain relief include swimming, cycling, and using an elliptical machine. These exercises help improve cardiovascular health and strengthen the muscles around the knee without putting excessive stress on the joint.
Is it safe to perform strength training exercises for knee stability if I have knee pain?
It is important to consult with a healthcare professional before starting any strength training exercises for knee stability, especially if you have knee pain. Proper guidance and modifications can help ensure that the exercises are safe and beneficial for your specific condition.
How can flexibility and range of motion exercises help with knee pain relief?
Flexibility and range of motion exercises help improve the flexibility of the muscles and tendons around the knee joint, which can reduce stiffness and discomfort. These exercises also promote better joint mobility and function, contributing to overall knee pain relief.
What role does nutrition play in managing knee pain?
Nutrition plays a crucial role in managing knee pain, as a balanced diet rich in nutrients such as omega-3 fatty acids, vitamin C, and antioxidants can help reduce inflammation and support joint health. Maintaining a healthy weight through proper nutrition also reduces the load on the knee joint, alleviating pain and discomfort.
Are there specific footwear and orthotics that can help with knee pain?
Choosing supportive footwear and orthotics designed to provide cushioning and stability can help reduce knee pain by improving alignment and reducing impact during daily activities. It is important to select footwear and orthotics that are suitable for your specific foot structure and gait pattern.
How can posture and body mechanics affect knee health?
Maintaining good posture and using proper body mechanics can help reduce strain on the knees and prevent unnecessary stress on the joint. Correct posture and body alignment contribute to better weight distribution, reducing the risk of developing knee pain and related issues.