Did you know that patellar dislocation accounts for approximately 2 to 3% of knee injuries? That’s right, this common condition affects a significant number of individuals, particularly young and active ones, including adolescent females and athletes.
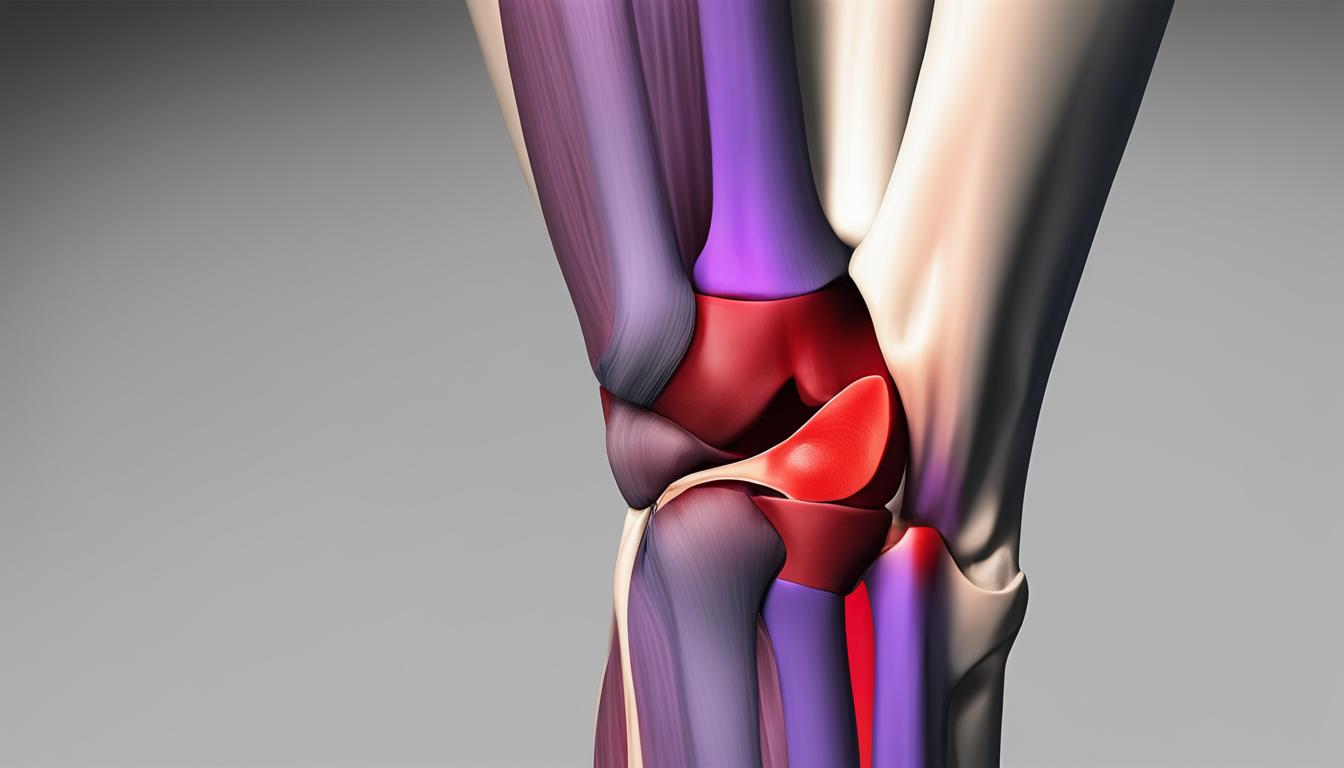
But what exactly is a lateral patella dislocation, and what are the causes and risk factors associated with it? In this article, we will delve into the world of patellar instability and explore the various factors that contribute to the occurrence of lateral patella dislocations.
Whether you’re a healthcare professional, a patient, or simply curious about knee injuries, understanding the causes and risk factors for lateral patellar dislocation is crucial for prevention, diagnosis, and effective management. Let’s dive in and discover the ins and outs of this condition and how it impacts individuals.
Risk Factors for Lateral Patellar Dislocation
Understanding the risk factors associated with lateral patellar dislocation is crucial for effective prevention and management. Several factors can increase an individual’s susceptibility to this condition.
Anatomical Risk Factors
Anatomical variations in the knee joint can predispose individuals to lateral patellar dislocation. These include:
- Patella Alta: An unusually high position of the patella, resulting in an increased risk of dislocation.
- Trochlear Dysplasia: Shallow or malformed groove in the femur, leading to poor patellar stability.
- Lateral Patella Tilt: Excessive lateral tilt of the patella, making it more prone to dislocation.
Ligamentous Laxity
Ligamentous laxity refers to increased looseness or flexibility of the ligaments in the knee joint. It is commonly seen in females and individuals with connective tissue disorders, such as Ehlers-Danlos syndrome. Ligamentous laxity can contribute to patellar instability and raise the risk of dislocation.
Muscle Imbalances
Muscle imbalances, particularly weakness of the vastus medialis oblique (VMO), can also predispose individuals to lateral patellar dislocation. The VMO plays a crucial role in stabilizing the patella, and its weakness can result in patellar instability.
Activity-Related Factors
Certain activities increase the risk of lateral patellar dislocation. These include:
- High-Impact Sports: Activities involving jumping, pivoting, or sudden changes in direction, such as basketball, soccer, and skiing.
- Dancing: Recurrent and forceful movements in dance styles that place stress on the knee joint.
Demographic Factors
Demographic factors can also influence the risk of lateral patellar dislocation:
- Teenagers: Adolescents, especially those experiencing rapid growth, may have looser joints and ligaments, making them more susceptible to patellar dislocation.
- Women: Women, with their wider hips and looser ligaments, may experience increased lateral stress on the knee, increasing the risk of dislocation.
- Big and Tall Men: Individuals with a larger body size may experience increased pressure on the knee joints, putting them at higher risk of patellar dislocation.
By understanding these risk factors, healthcare professionals can implement targeted prevention strategies and develop personalized treatment plans for individuals with lateral patellar dislocation.

| Anatomical Risk Factors | Ligamentous Laxity | Muscle Imbalances | Activity-Related Factors | Demographic Factors |
|---|---|---|---|---|
| Patella Alta | Ligamentous laxity in females and individuals with connective tissue disorders | Weakness of the vastus medialis oblique (VMO) muscle | High-impact sports | Teenagers |
| Trochlear Dysplasia | Dancing | Women | ||
| Excessive lateral patella tilt | Big and tall men |
Signs and Symptoms of Lateral Patellar Dislocation
Common signs and symptoms of lateral patellar dislocation include:
- An audible pop or snapping sound at the time of dislocation.
- Buckling or instability of the knee.
- Intense pain in the knee.
- Sudden swelling and bruising at the knee.
- Locking of the knee joint.
- Inability to walk or bear weight on the affected leg.
- Visual dislocation of the kneecap, which may be visibly out of place.
When a lateral patellar dislocation occurs, it is often accompanied by an audible pop or snapping sound. This distinct sound is indicative of the displacement of the kneecap from its normal position. In addition to the audible pop, individuals may experience a sensation of buckling or instability in the knee joint. This instability can make it difficult to maintain balance and perform regular activities.
The most prominent symptom of a lateral patellar dislocation is intense pain in the knee. The pain is often immediate and can be severe, making it challenging to bear weight on the affected leg. Swelling and bruising are also common after a patellar dislocation, as the soft tissues surrounding the knee joint may become inflamed due to the trauma.
Another sign of a lateral patellar dislocation is the locking of the knee joint. This occurs when the kneecap becomes trapped outside of its normal position and cannot be easily moved back into place. The locked knee joint can cause a significant limitation in mobility and may require medical intervention to restore proper alignment.
Visually, a lateral patellar dislocation can be identified by the visible dislocation of the kneecap. The kneecap may appear shifted or out of place, providing a clear indication of the dislocation. This visual dislocation is often accompanied by swelling and bruising, further underscoring the severity of the injury.
Recognizing these signs and symptoms is essential for prompt diagnosis and appropriate management of a lateral patellar dislocation. If any of these symptoms are experienced after a knee injury, seeking medical attention is crucial to prevent further damage and facilitate effective treatment.

Diagnosis and Evaluation of Lateral Patellar Dislocation
Diagnosing lateral patellar dislocation involves a comprehensive approach, combining the patient’s medical history, physical examination, and imaging studies. This allows healthcare professionals to accurately assess the extent of the injury and determine the most appropriate treatment plan.
History: Patients with lateral patellar dislocation often recall a specific traumatic event that triggered the injury, such as a non-contact twisting injury or a direct blow to the knee. They typically experience sudden pain, swelling, and joint instability.
Physical Examination: During a physical examination, physicians evaluate several key factors to confirm the diagnosis. This includes assessing the knee for signs of joint effusion or hemarthrosis (blood in the joint), alignment abnormalities, tenderness, and irregularities along the poles of the patella. Range of motion restrictions are also assessed, and specific tests like the patellar apprehension test and patellar tracking assessment may be performed to evaluate stability and tracking of the patella.
Imaging Studies: X-rays are commonly used to identify any associated fractures, malalignment, or anatomical risk factors that may contribute to patellar instability. Additional imaging, such as CT scans or MRI, may be necessary to evaluate the full extent of the injury, measure the tuberosity tibia-trochlear groove distance, and assess for potential osteochondral lesions.
The combination of history, physical examination, and imaging studies allows healthcare professionals to make an accurate diagnosis of lateral patellar dislocation. This comprehensive evaluation is crucial in developing an effective treatment plan that addresses the specific needs and circumstances of the individual patient.
Treatment and Management of Lateral Patellar Dislocation
When it comes to treating lateral patellar dislocation, there are several approaches that can be taken based on the severity of the condition and the individual’s specific needs. In many cases, conservative management techniques can effectively treat primary acute patellar dislocations without the need for surgery. This typically involves immobilization of the knee, physiotherapy sessions to strengthen the surrounding muscles and improve stability, and the use of bracing to prevent re-dislocation. Additionally, medications may be prescribed to manage pain and inflammation during the recovery process.
However, if the dislocations become recurrent or chronic, or if there is significant ligamentous or bony damage, surgical intervention may be necessary. There are various surgical options available, including lateral release, medial patellofemoral ligament reconstruction, and distal realignment or anteromedialisation. These procedures aim to restore proper alignment and stability to the patella, reducing the risk of future dislocations and improving overall knee function.
Physiotherapy plays a critical role in the management of lateral patellar dislocation, regardless of whether conservative or surgical treatment is pursued. An individualized physiotherapy program may include exercises to improve range of motion, strengthen the quadriceps and other surrounding muscles, enhance proprioception, and promote proper patellar tracking. These exercises and techniques are designed to support the recovery process and help patients regain full function and stability in their knee joint.
Preventing lateral patellar dislocation is also a key aspect of treatment and management. Addressing risk factors is essential, such as providing appropriate training and conditioning for athletes, focusing on muscle balance and stability, and utilizing protective bracing when necessary. By taking proactive measures to reduce the likelihood of dislocation, individuals can safeguard their knee health and minimize the need for additional treatment or surgery.
Recovering from a lateral patellar dislocation requires a comprehensive rehabilitation program that includes ongoing monitoring and follow-up care. Range of motion exercises, strength-building exercises, and stability training are essential components of this program, along with gradually reintroducing functional activities. The goal is to restore full range of motion, build strength, and ensure a stable knee joint, allowing individuals to return to their normal activities with confidence.
FAQ
Why does the patella dislocate laterally?
Acute lateral patella dislocations are typically caused by trauma, such as a non-contact twisting injury or a direct blow to the knee. Recurrent subluxation and chronic laxity of the patella can also lead to lateral patellar dislocations. Anatomic variations, ligamentous laxity, muscle imbalances, and certain activities can also contribute to patellar instability.
What are the risk factors for lateral patellar dislocation?
Risk factors for lateral patellar dislocation include anatomical variations such as patella alta and trochlear dysplasia, ligamentous laxity (more common in females and individuals with connective tissue disorders), and muscle imbalances. Certain activities, rapid growth in teenagers, wider hips and looser ligaments in women, and increased pressure on the joints in big and tall men can also increase the risk of dislocation.
What are the common signs and symptoms of lateral patellar dislocation?
Common signs and symptoms of lateral patellar dislocation include an audible pop or snapping sound at the time of dislocation, buckling or instability of the knee, intense pain, sudden swelling and bruising, locking of the knee joint, inability to walk or bear weight on the affected leg, and visual dislocation of the kneecap.
How is lateral patellar dislocation diagnosed and evaluated?
Diagnosis of lateral patellar dislocation involves a combination of history, physical examination, and imaging studies. History includes a traumatic event followed by pain, swelling, and joint instability. Physical examination assesses the knee for abnormalities, tenderness, and range of motion restrictions. Imaging studies, such as X-rays, CT scans, or MRI, are used to identify associated fractures, malalignment, anatomical risk factors, and osteochondral lesions.
What are the treatment and management options for lateral patellar dislocation?
Primary acute patellar dislocations can often be managed conservatively with immobilization, physiotherapy, bracing, and medication for pain and inflammation. Surgical intervention may be necessary for recurrent or chronic dislocations, significant ligamentous or bony damage. Surgical options include lateral release, medial patellofemoral ligament reconstruction, and distal realignment or anteromedialisation. Physiotherapy is crucial for rehabilitation and includes range of motion exercises, strengthening exercises, proprioception training, and patellar tracking exercises. Prevention involves addressing risk factors, proper training, and using protective bracing. Recovery requires a comprehensive rehabilitation program and close monitoring.
Leave a Reply