Welcome to our comprehensive guide on knee osteoarthritis. In this article, we will explore the origins of this common condition and understand where it starts. If you or someone you know is experiencing knee joint pain, it is crucial to delve into the underlying causes and mechanisms of knee osteoarthritis to better manage and treat the symptoms.
Knee osteoarthritis, also known as degenerative joint disease of the knee, is primarily a result of wear and tear and a progressive loss of articular cartilage. It can be classified into two types: primary and secondary osteoarthritis. Primary osteoarthritis refers to articular degeneration without any apparent underlying reason, while secondary osteoarthritis is caused by abnormal concentration of force across the joint or abnormal articular cartilage.
Commonly observed in the elderly, knee osteoarthritis can lead to disability and significantly impact daily life. The primary symptoms include knee pain that is gradual in onset and worsens with activity, knee stiffness and swelling, pain after prolonged sitting or resting, as well as pain that worsens over time.
Treatment for knee osteoarthritis typically starts with conservative methods and progresses to surgical options if conservative treatments fail. Unfortunately, there are currently no proven disease-modifying agents for the treatment of knee osteoarthritis.
Throughout this guide, we will explore the causes, risk factors, prevalence, pathophysiology, diagnosis, and clinical symptoms associated with knee osteoarthritis. We will also provide insights into the prevention strategies and personalized treatment plans that can help manage this condition.
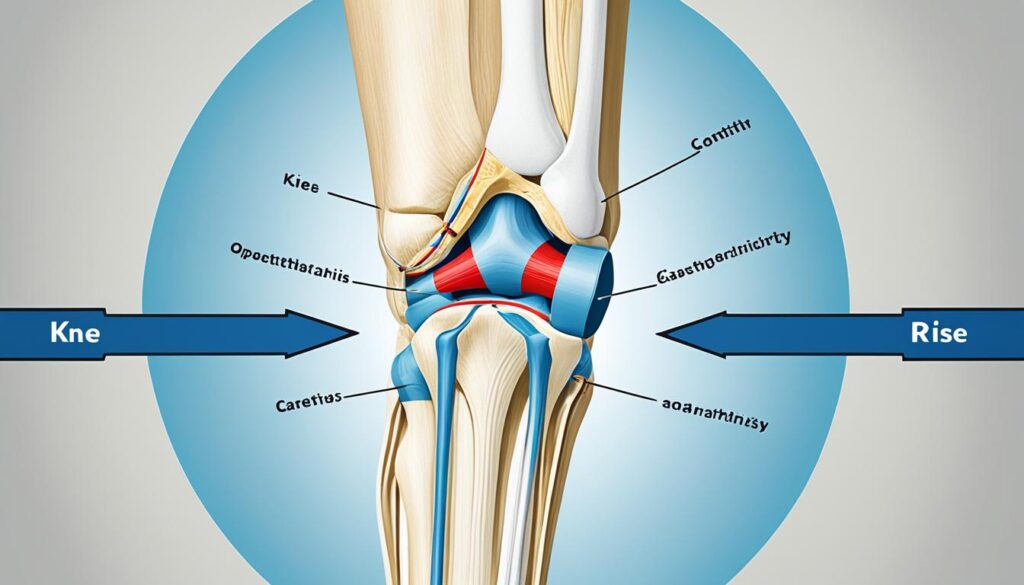
Let’s begin our exploration of knee osteoarthritis origins and gain a deeper understanding of where this condition starts. Before we dive in, take a moment to familiarize yourself with the image below, illustrating the knee joint.
Causes and Risk Factors
When it comes to knee osteoarthritis, there are various causes and risk factors that contribute to its development. Let’s take a closer look at these factors:
Primary and Secondary Osteoarthritis
Osteoarthritis can be classified into two categories: primary and secondary. Primary knee osteoarthritis occurs when the articular cartilage undergoes degeneration without any known reason. It is often associated with wear and tear on the knee joint over time.
“Primary knee osteoarthritis is typically the result of articular cartilage degeneration without any known reason, often associated with wear and tear.”
Secondary knee osteoarthritis, on the other hand, is the result of articular cartilage degeneration due to a specific cause or condition. This can include post-traumatic causes, such as a previous injury or surgery to the knee, or underlying conditions like rheumatoid arthritis.
Risk Factors
There are several risk factors that can increase the likelihood of developing knee osteoarthritis. Some of these factors are modifiable, while others are not:
| Modifiable Risk Factors | Non-Modifiable Risk Factors |
|---|---|
|
|
Modifiable risk factors can be addressed through lifestyle changes and preventative measures. For example, maintaining a healthy weight, engaging in regular exercise to strengthen the muscles around the knee joint, and avoiding activities that put excessive stress on the knee can help reduce the risk of knee osteoarthritis.
“There are several risk factors that can increase the likelihood of developing knee osteoarthritis.”
Non-modifiable risk factors, such as age, gender, genetics, and race, can’t be changed. However, being aware of these factors can help individuals and healthcare professionals identify those who may be at a higher risk and develop appropriate management plans.
With the right combination of treatment and lifestyle modifications, individuals can effectively manage knee osteoarthritis and improve their quality of life. In the next section, we will explore more about the prevalence and epidemiology of knee osteoarthritis.
Prevalence and Epidemiology
Knee osteoarthritis is the most common type of arthritis diagnosed and its prevalence is expected to increase due to the aging population and obesity epidemic.
Approximately 13% of women and 10% of men aged 60 and older have symptomatic knee osteoarthritis, with the prevalence rising to as high as 40% among those older than 70. Women are more susceptible to knee osteoarthritis compared to men, likely due to hormonal and anatomical differences.
Various factors can influence the development of knee osteoarthritis, including physical activity levels, history of knee trauma, and race. Those who engage in heavy physical activities or have experienced significant knee injuries are at a higher risk of developing knee osteoarthritis. Studies have also shown that certain races, such as African Americans, tend to have a higher prevalence of knee osteoarthritis.
It is important to note that radiographic findings of knee osteoarthritis may not always correspond with symptomatic experiences. Only 15% of patients with radiographic evidence of knee osteoarthritis report experiencing related symptoms. This indicates that the severity of radiographic findings may not always reflect the level of disability or pain experienced by individuals with knee osteoarthritis.
The incidence of symptomatic knee osteoarthritis is approximately 240 cases per 100,000 people per year. This highlights the significant impact of knee osteoarthritis on the population and the need for effective management strategies.
The image above illustrates a knee joint experiencing inflammation, a common symptom of knee osteoarthritis.
Pathophysiology
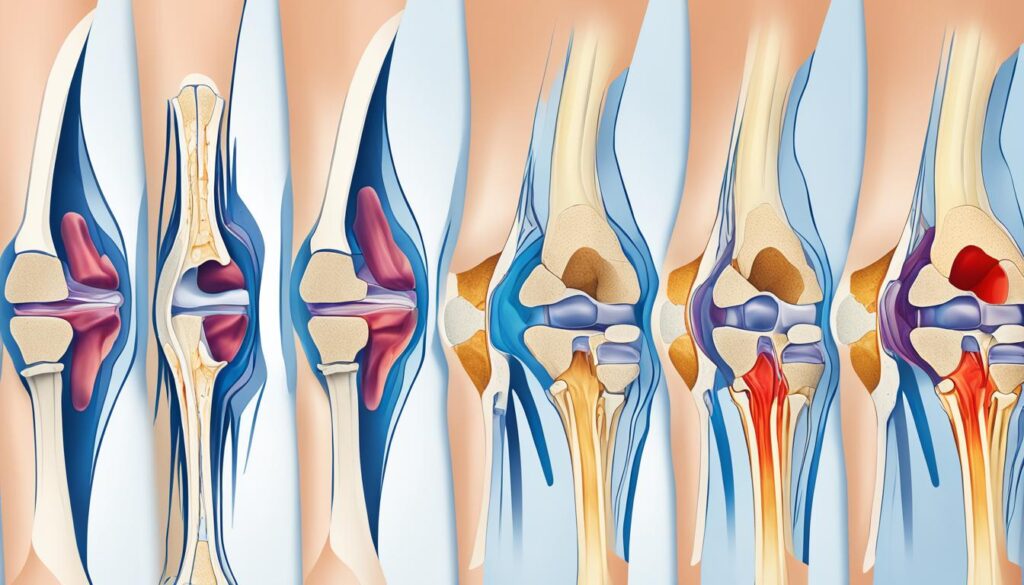
Knee osteoarthritis is a complex condition that involves the progressive degeneration of the knee cartilage, leading to wear and tear of the knee joint. Understanding the pathophysiology of knee osteoarthritis can help us comprehend the underlying mechanisms of this disease and explore potential treatment strategies.
The articular cartilage in the knee joint is primarily composed of type II collagen, proteoglycans, chondrocytes, and water. In knee osteoarthritis, the balance between cartilage degradation and synthesis is disrupted. This imbalance is caused by the overexpression of degradative enzymes called matrix metalloproteases (MMPs).
In response to cartilage damage, chondrocytes, the cells responsible for maintaining cartilage health, attempt to repair the damaged tissue by increasing the synthesis of proteoglycans. However, due to the overexpression of MMPs, the equilibrium is disturbed, leading to a decrease in proteoglycan content, an increase in water content, and the disorganization of collagen fibers. Ultimately, this results in the erosion of the articular cartilage that cushions the knee joint, causing pain and functional impairment.
Importantly, knee osteoarthritis should not be mistaken as a normal part of aging. While aging can contribute to the degeneration of cartilage, knee osteoarthritis is its own distinct disease with specific characteristics that differentiate it from normal aging cartilage.
By gaining a deeper understanding of the pathophysiology of knee osteoarthritis, we can develop targeted interventions that aim to restore the balance of cartilage degradation and synthesis, slowing down the progression of the disease and improving the quality of life for those affected.
The Difference Between Knee Osteoarthritis and Normal Aging Cartilage
While knee osteoarthritis and normal aging cartilage share some common features, there are distinct differences between the two. These differences highlight the pathological processes that occur specifically in knee osteoarthritis and emphasize the need for targeted treatments.
| Knee Osteoarthritis | Normal Aging Cartilage |
|---|---|
| Progressive loss of articular cartilage | Gradual thinning of cartilage |
| Increased expression of MMPs | Normal expression of MMPs |
| Inflammation in the joint | No inflammation |
| Disorganized collagen fibers | Organized collagen fibers |
Knee osteoarthritis is a complex disease that involves the progressive degeneration of knee cartilage. Understanding its pathophysiology and the unique characteristics that set it apart from normal aging cartilage is crucial for developing effective treatment strategies. By targeting the specific processes involved in knee osteoarthritis, we can work towards improving the lives of individuals suffering from this debilitating condition.
Diagnosis and Clinical Symptoms
The diagnosis of knee osteoarthritis is based on the patient’s history, physical examination, and sometimes imaging studies. The history should include information about the onset, location, duration, and characteristics of knee pain, as well as alleviating and aggravating factors.
During physical examination, healthcare professionals may observe periarticular erythema and swelling, quadriceps muscle atrophy, and varus or valgus deformities. They may also assess gait abnormalities and perform range of motion testing and palpation of the knee joint to gather diagnostic information.
Common clinical symptoms of knee osteoarthritis include:
- Knee pain that is gradual in onset and worsens with activity
- Stiffness and swelling in the knee
- Pain after prolonged sitting or resting
- Pain that worsens over time
These symptoms can significantly affect an individual’s mobility and quality of life, making an accurate diagnosis essential for appropriate management and treatment.
To better understand the impact of knee osteoarthritis symptoms on patients, consider the following quote:
“The pain in my knee started gradually and became worse over time. It’s especially bothersome after I’ve been sitting for a while, and I also notice stiffness and swelling. It’s frustrating because it limits my ability to enjoy the activities I used to love.”
– Patient with knee osteoarthritis
Conclusion
Knee osteoarthritis can have a significant impact on the quality of life and mobility of affected individuals. However, there are strategies that can help reduce the risk and delay the progression of the disease. Prevention is key in managing knee osteoarthritis, and it starts with maintaining a healthy weight. Excess weight puts additional stress on the knee joints, increasing the risk of cartilage damage and degeneration. By maintaining a healthy weight, individuals can lessen the burden on their knees and reduce the likelihood of developing knee osteoarthritis.
Regular exercise is another important component of prevention. Engaging in activities that strengthen the muscles around the knee joint can provide support and stability, reducing the risk of joint damage. Low-impact exercises such as swimming, cycling, and walking can be beneficial for individuals with knee osteoarthritis. It is important to consult with a healthcare professional or physical therapist to develop an exercise program that is safe and effective.
Avoiding activities that put excessive stress on the knee is also important for preventing knee osteoarthritis. This includes activities that involve repetitive movements or high-impact activities such as running or jumping. By being mindful of these activities and modifying them or finding alternatives, individuals can protect their knees and reduce the risk of osteoarthritis.
Managing other health conditions that may contribute to knee osteoarthritis is also essential. Conditions such as metabolic syndrome and diabetes can increase the risk of developing osteoarthritis. By effectively managing these conditions through lifestyle changes and medication, individuals can reduce their risk and protect their knee joints.
FAQ
What is knee osteoarthritis?
Knee osteoarthritis, also known as degenerative joint disease of the knee, is the result of wear and tear and progressive loss of articular cartilage. It is a common type of arthritis that primarily affects the elderly and can lead to disability.
What are the symptoms of knee osteoarthritis?
Common symptoms of knee osteoarthritis include gradual onset knee pain that worsens with activity, knee stiffness and swelling, pain after prolonged sitting or resting, and pain that worsens over time.
What are the causes and risk factors of knee osteoarthritis?
Knee osteoarthritis can be caused by articular cartilage degeneration without any known reason (primary osteoarthritis) or as a consequence of an underlying condition or abnormal stress on the joint (secondary osteoarthritis). Risk factors for knee osteoarthritis include factors like articular trauma, occupation involving prolonged standing and repetitive knee bending, muscle weakness or imbalance, weight, and certain health conditions.
How common is knee osteoarthritis?
Knee osteoarthritis is the most common type of diagnosed arthritis and its prevalence is expected to increase due to the aging population and obesity epidemic. Approximately 13% of women and 10% of men aged 60 and older have symptomatic knee osteoarthritis.
What is the pathophysiology of knee osteoarthritis?
Knee osteoarthritis involves the progressive loss of articular cartilage, which leads to the erosion of the joint. This degeneration is caused by an imbalance between cartilage degradation and synthesis, which is often associated with the overexpression of degradative enzymes called matrix metalloproteases (MMPs).
How is knee osteoarthritis diagnosed?
The diagnosis of knee osteoarthritis is typically based on the patient’s history, physical examination, and sometimes imaging studies. The history should include information about the onset, location, and characteristics of knee pain. Physical examination may reveal swelling, muscle atrophy, deformities, and gait abnormalities.
Can knee osteoarthritis be prevented?
While there is no cure for knee osteoarthritis, prevention strategies can help reduce the risk and delay the progression of the disease. These strategies include maintaining a healthy weight, engaging in regular exercise to strengthen the muscles around the knee joint, avoiding activities that put excessive stress on the knee, and managing other health conditions that may contribute to knee osteoarthritis.

Leave a Reply