Are you experiencing persistent knee pain that doesn’t seem to subside? The knee is a complex structure made up of various soft tissues, and issues like Synovial Plica Syndrome can be a source of discomfort.
This condition occurs when the plica, a fold in the membrane surrounding the knee joint, becomes irritated and inflamed. Understanding the symptoms is crucial for proper diagnosis and treatment, as they can be similar to those of other knee problems.
Key Takeaways
- Synovial Plica Syndrome affects the knee, causing pain and discomfort.
- The condition is characterized by irritation and inflammation of the plica.
- Symptoms can be similar to other knee issues, making diagnosis challenging.
- Understanding the symptoms is key to proper diagnosis and treatment.
- Accurate diagnosis is crucial for effective treatment.
Understanding Synovial Plica Syndrome
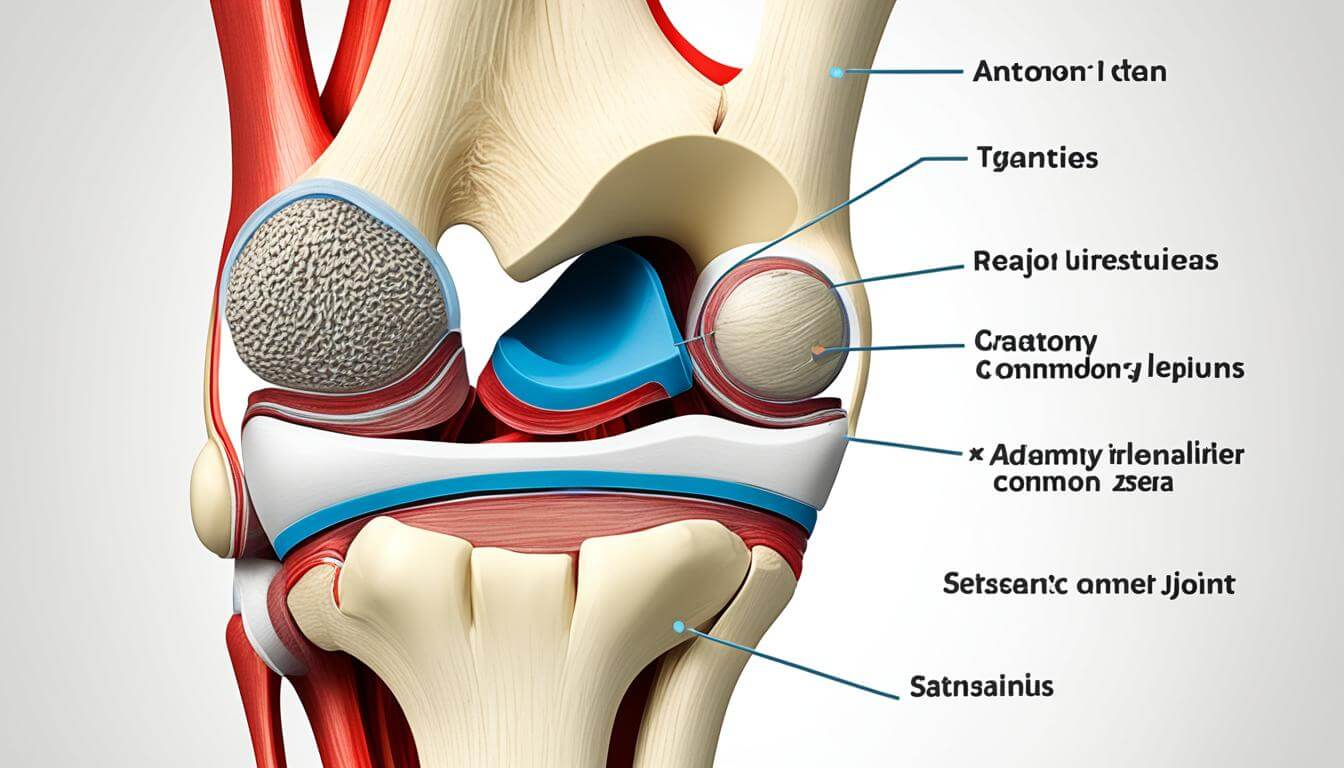
Understanding the intricacies of Synovial Plica Syndrome is crucial for diagnosing and treating knee discomfort. Synovial Plica Syndrome involves the irritation of the plica, which are folds in the synovial tissue surrounding the knee joint.
What is Synovial Plica Syndrome?
Synovial Plica Syndrome occurs when the plica becomes inflamed, typically due to overuse or direct trauma to the knee. This inflammation can lead to plica irritation, causing pain and discomfort, particularly in the center of the kneecap, known as medial patellar plica syndrome.
Research indicates that a significant percentage of patients undergoing arthroscopic surgery have remnants of their synovial plicae, highlighting the prevalence of this condition.
Causes of Synovial Plica Syndrome
The primary causes of Synovial Plica Syndrome include repetitive knee movements and direct trauma to the knee. Athletes and individuals engaged in activities that involve frequent knee bending are more susceptible to this condition.
- Overuse or repetitive strain on the knee
- Direct trauma or injury to the knee
- Poor knee alignment or tracking
Who is Affected?
Synovial Plica Syndrome commonly affects athletes and individuals who participate in sports or activities that involve repetitive knee movements. This includes runners, cyclists, and those involved in jumping sports.
Understanding who is at risk can help in prevention and early diagnosis, potentially reducing the severity of symptoms and improving treatment outcomes.
Common Symptoms
Knee problems are a hallmark of Synovial Plica Syndrome, with several symptoms being commonly reported. The condition can manifest in different ways, but there are key indicators that healthcare professionals look for when diagnosing Synovial Plica Syndrome.
Pain Location
Pain associated with Synovial Plica Syndrome is typically located around the kneecap. This pain is often described as achy rather than sharp or shooting. Activities that stress the knee, such as squatting, bending, or using stairs, can exacerbate the pain.
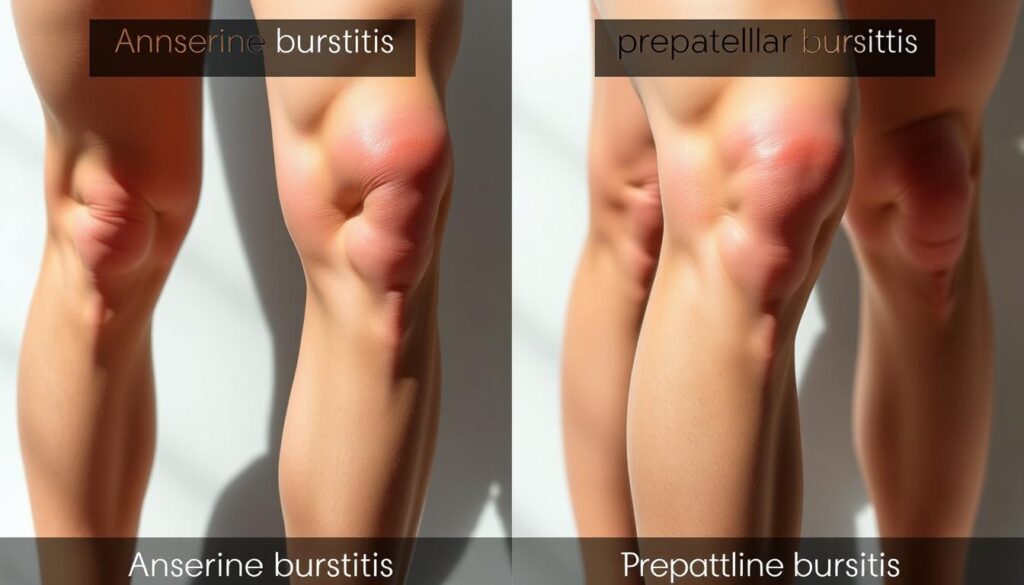
Swelling Around the Knee
Swelling is another common symptom of Synovial Plica Syndrome. The swelling occurs due to inflammation of the plica, which can be irritated by repetitive knee motions or direct trauma to the knee. This swelling can lead to discomfort and may affect the appearance of the knee.
Stiffness and Reduced Mobility
Stiffness and reduced mobility are also characteristic symptoms. The inflammation and irritation of the synovial plica can lead to a decrease in the knee’s range of motion, making it difficult to perform daily activities or engage in physical exercises without discomfort.

The symptoms of Synovial Plica Syndrome can vary in severity and impact daily life to different extents. Understanding these symptoms is crucial for seeking appropriate medical care.
| Symptom | Description | Common Triggers |
|---|---|---|
| Pain Around Kneecap | Achy pain rather than sharp | Squatting, bending, using stairs |
| Swelling | Inflammation causing knee swelling | Repetitive knee motions, direct trauma |
| Stiffness and Reduced Mobility | Decreased range of motion | Inflammation and irritation of the plica |
How Symptoms Manifest
The manifestation of Synovial Plica Syndrome symptoms can vary significantly among individuals. Symptoms can be influenced by the level of physical activity, the specific irritation of the plica, and individual tolerance to pain.
Symptoms During Physical Activity
During physical activity, symptoms of Synovial Plica Syndrome can worsen. Activities that involve bending, jumping, or repetitive knee movements can irritate the plica, leading to pain and discomfort. Some individuals may experience a catching or locking sensation in the knee, particularly when getting up from a seated position after sitting for an extended period.
Common symptoms during physical activity include:
- Pain or tenderness around the knee
- Joint clicking or cracking noises when bending or straightening the knee
- Swelling or inflammation around the affected area
- Stiffness or reduced mobility in the knee
Symptoms at Rest
Even at rest, some individuals with Synovial Plica Syndrome may experience symptoms. The condition can cause discomfort or pain when sitting for long periods or when the knee is in a bent position for an extended time.
Night-time Pain
Night-time pain is another symptom that some individuals with Synovial Plica Syndrome may experience. The pain can be severe enough to disrupt sleep, particularly if the individual sleeps with their knee bent. Understanding the pattern of night-time pain can help in diagnosing and managing the condition.
Key factors that contribute to night-time pain include:
- The severity of the plica irritation
- The individual’s overall knee health
- Sleeping position and habits
Diagnosis of Synovial Plica Syndrome
Diagnosing Synovial Plica Syndrome requires a comprehensive approach that involves evaluating the patient’s medical history, conducting a thorough physical examination, and sometimes utilizing imaging tests. This multi-faceted diagnostic strategy is crucial for accurately identifying the condition and ruling out other potential causes of knee problems.
Medical History Evaluation
The first step in diagnosing Synovial Plica Syndrome is a thorough medical history evaluation. This involves assessing the patient’s symptoms, including the onset and duration of Synovial plica syndrome symptoms, to understand the condition’s progression. Healthcare professionals will also inquire about any previous knee injuries or conditions that could be contributing to the current symptoms.
Physical Exam Details
A physical examination is a critical component of the diagnostic process. During the exam, the healthcare provider will assess the knee’s range of motion, check for tenderness, and perform specific maneuvers to reproduce the patient’s symptoms. This hands-on evaluation helps to identify the presence of a synovial plica and assess its impact on knee function. For more information on when to seek medical help for knee pain, visit https://kneehurt.com/when-to-seek-medical-help-for-knee-pain/.
Imaging Tests Utilized
While a diagnosis can often be made based on medical history and physical examination, imaging tests may be employed to confirm the diagnosis or rule out other causes of knee pain. Common imaging tests include X-rays, MRI (Magnetic Resonance Imaging), and ultrasound. These tests provide detailed images of the knee’s internal structures, helping healthcare professionals to visualize the synovial plica and assess any associated inflammation or irritation.
In conclusion, diagnosing Synovial Plica Syndrome involves a combination of medical history evaluation, physical examination, and sometimes imaging tests. By understanding the diagnostic process, patients can better appreciate the complexity of identifying this condition and the importance of seeking professional medical advice for accurate diagnosis and effective treatment.
Treatment Options
Synovial Plica Syndrome treatment encompasses a range of strategies from conservative management to surgical interventions, depending on the severity and persistence of symptoms.
Conservative Treatments
Most instances of medial patellar plica syndrome respond well to alternative treatment options. These include chiropractic care, physical therapy, or even a tailored exercise plan at home. Such conservative approaches aim to alleviate knee pain and knee discomfort by improving knee function and reducing inflammation.
Surgical Interventions
In cases where conservative treatments fail to provide relief, surgical options may be considered. Surgical interventions for Synovial Plica Syndrome typically involve arthroscopic procedures to remove or repair the problematic plica. For more information on Synovial Plica Syndrome, you can visit Healthline’s resource on the condition.
Rehabilitation Strategies
Regardless of whether the treatment involves conservative methods or surgery, rehabilitation plays a crucial role in recovery. Rehabilitation strategies often include a structured physical therapy program aimed at restoring knee strength and mobility, thereby reducing the risk of future complications.
| Treatment Approach | Description | Benefits |
|---|---|---|
| Conservative Treatments | Includes chiropractic care, physical therapy, and home exercise plans. | Non-invasive, reduces knee pain and discomfort. |
| Surgical Interventions | Arthroscopic procedures to remove or repair the plica. | Effective for severe cases not responding to conservative treatments. |
| Rehabilitation Strategies | Structured physical therapy programs. | Restores knee strength and mobility, prevents future issues. |
Managing Pain from Symptoms
Effective management of Synovial Plica Syndrome symptoms involves a multi-faceted approach to pain relief. This condition can cause significant discomfort due to plica irritation and swelling around the knee. Managing pain is crucial to improve the quality of life for individuals affected by this condition.
Over-the-Counter Medications
Over-the-counter (OTC) medications are often the first line of defense against pain associated with Synovial Plica Syndrome. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation. It’s essential to follow the recommended dosage and consult with a healthcare professional before starting any medication regimen.
Some individuals may find relief with topical creams or gels that contain NSAIDs or capsaicin. These products can be applied directly to the skin around the affected area, providing localized pain relief.
Alternative Pain Management Techniques
In addition to OTC medications, alternative pain management techniques can be beneficial. Physical therapy is a valuable approach, as it can help improve knee function and reduce pain. A physical therapist can design a personalized exercise program to strengthen the muscles around the knee and improve flexibility.
- Applying ice packs to reduce swelling and ease pain
- Using compression bandages to provide support
- Elevating the knee to minimize swelling
In some cases, healthcare professionals may recommend corticosteroid injections to reduce inflammation and relieve pain. These injections can provide significant relief, especially when the pain is severe and interferes with daily activities.
It’s crucial for individuals with Synovial Plica Syndrome to work closely with their healthcare provider to develop a comprehensive pain management plan. By combining different strategies, individuals can better manage their symptoms and improve their overall quality of life.
Lifestyle Adjustments
To manage Synovial Plica Syndrome effectively, it’s essential to make certain lifestyle adjustments. These modifications can help alleviate symptoms such as stiffness and joint clicking, improving overall knee function.
Exercises to Alleviate Symptoms
Engaging in specific exercises can help strengthen the muscles around the knee, thereby reducing the severity of symptoms. Activities such as biking, swimming, walking, or using an elliptical machine are beneficial as they promote knee mobility without excessive strain.
Strengthening the quadriceps through specific stretches and exercises is particularly helpful. This can be achieved through:
- Straight leg raises to strengthen the quadriceps
- Wall squats to improve knee stability
- Leg press exercises to enhance muscle strength around the knee
Importance of Rest and Recovery
Adequate rest and recovery are crucial for managing Synovial Plica Syndrome. Avoiding activities that exacerbate the condition and ensuring sufficient rest can help alleviate symptoms.
It’s also important to listen to your body and take regular breaks during activities to prevent overuse. By balancing activity with rest, individuals can better manage their symptoms and improve their quality of life.
When to See a Doctor
Recognizing the signs that necessitate a doctor’s visit is vital for individuals suffering from Synovial Plica Syndrome. It’s essential to be aware of the symptoms that indicate a need for immediate medical evaluation.
Warning Signs of Severe Symptoms
Severe symptoms of Synovial Plica Syndrome can manifest as significant pain or locking of the knee, which are indicative of potential complications. If you experience any of the following, seek medical attention promptly:
- Intense pain that interferes with daily activities
- Knee locking or catching sensations
- Significant swelling or redness around the knee
- Instability or feeling of the knee giving way
If chiropractic care, physical therapy, or other treatments do not alleviate knee plica syndrome symptoms, a procedure known as arthroscopic resection may be necessary. Understanding these warning signs can help prevent further knee problems.
Regular Check-Ups and Monitoring
Regular check-ups with a healthcare provider are crucial for monitoring the condition and adjusting treatment as necessary. These visits can help in early detection of any worsening of symptoms or development of new issues.
| Monitoring Aspect | Importance | Action |
|---|---|---|
| Symptom Severity | Understanding the progression of the syndrome | Adjust treatment plan |
| Treatment Effectiveness | Evaluating the success of current treatments | Modify or continue treatment |
| Knee Functionality | Assessing the impact on knee mobility and strength | Implement rehabilitation strategies |
Living with Synovial Plica Syndrome
Living with Synovial Plica Syndrome can be challenging, but there are several strategies that can help alleviate its symptoms. Effective management involves a combination of medical treatments, lifestyle adjustments, and self-care practices.
Coping Strategies
Coping with Synovial Plica Syndrome requires a multifaceted approach. Physical therapy is often recommended to improve knee function and reduce pain. Exercises tailored to strengthen the muscles around the knee can help stabilize the joint and alleviate stress on the plica.
In addition to physical therapy, lifestyle modifications play a crucial role. Avoiding activities that aggravate the condition, maintaining a healthy weight, and using proper footwear can significantly impact symptom management.
- Engage in low-impact activities such as cycling or swimming to maintain fitness without exacerbating the condition.
- Use knee supports or braces if recommended by a healthcare provider to provide additional stability.
- Practice stress-reducing techniques, such as meditation or deep breathing, to manage stress that can exacerbate pain.
Supporting Resources and Communities
Connecting with others who understand the challenges of living with Synovial Plica Syndrome can be incredibly beneficial. Support groups, either online or in-person, offer a platform to share experiences, gain insights, and find emotional support.
Furthermore, educational resources from reputable organizations can provide valuable information on managing the condition. Staying informed about the latest treatment options and management strategies is empowering.
By adopting a proactive approach to managing Synovial Plica Syndrome and leveraging available resources, individuals can lead active and fulfilling lives despite the challenges posed by the condition.
Conclusion
Understanding the symptoms and treatment options is crucial for managing Synovial Plica Syndrome. Early diagnosis and appropriate treatment can significantly alleviate knee discomfort associated with plica irritation.
Personalized Management Plans
Developing a personalized management plan with healthcare professionals is essential. This plan may include conservative treatments, lifestyle adjustments, and rehabilitation strategies to address the condition effectively.
By adopting a comprehensive approach to managing Synovial Plica Syndrome, individuals can reduce the risk of complications and improve their overall quality of life. This involves being aware of the symptoms, making necessary lifestyle changes, and adhering to the recommended treatment plan to mitigate knee discomfort and plica irritation.
FAQ
What are the common symptoms of Synovial Plica Syndrome?
The common symptoms include pain around the kneecap, swelling, stiffness, and reduced mobility. Some individuals may also experience joint clicking, locking, or knee discomfort.
What causes Synovial Plica Syndrome?
Synovial Plica Syndrome is often caused by overuse or direct trauma to the knee, leading to irritation and inflammation of the plica. Activities that involve repetitive knee movements can exacerbate the condition.
How is Synovial Plica Syndrome diagnosed?
Diagnosis involves a comprehensive approach, including medical history evaluation, physical examination, and sometimes imaging tests, to rule out other possible causes of knee pain and accurately diagnose the condition.
What are the treatment options for Synovial Plica Syndrome?
Treatment can range from conservative management, including physical therapy, chiropractic care, and activity modifications, to surgical interventions, depending on the severity and persistence of symptoms.
How can pain from Synovial Plica Syndrome be managed?
Pain management can involve over-the-counter medications, alternative pain management techniques, and in some cases, corticosteroid injections to alleviate symptoms and improve quality of life.
What lifestyle adjustments can help alleviate Synovial Plica Syndrome symptoms?
Engaging in exercises that strengthen the muscles around the knee, avoiding activities that exacerbate the condition, and ensuring adequate rest and recovery can help alleviate symptoms and improve function.
When should I seek medical attention for Synovial Plica Syndrome?
Severe symptoms, such as significant pain or locking of the knee, warrant immediate medical evaluation. Regular check-ups with a healthcare provider can also help monitor the condition and adjust treatment as necessary.
Can Synovial Plica Syndrome be managed effectively?
Yes, with proper diagnosis and treatment, Synovial Plica Syndrome is a manageable condition. By understanding the symptoms, treatment options, and lifestyle adjustments, individuals can effectively manage their condition and improve their quality of life.
What are some coping strategies for living with Synovial Plica Syndrome?
Coping strategies include making lifestyle adjustments, seeking support from resources and communities, and working closely with healthcare professionals to develop a personalized management plan.