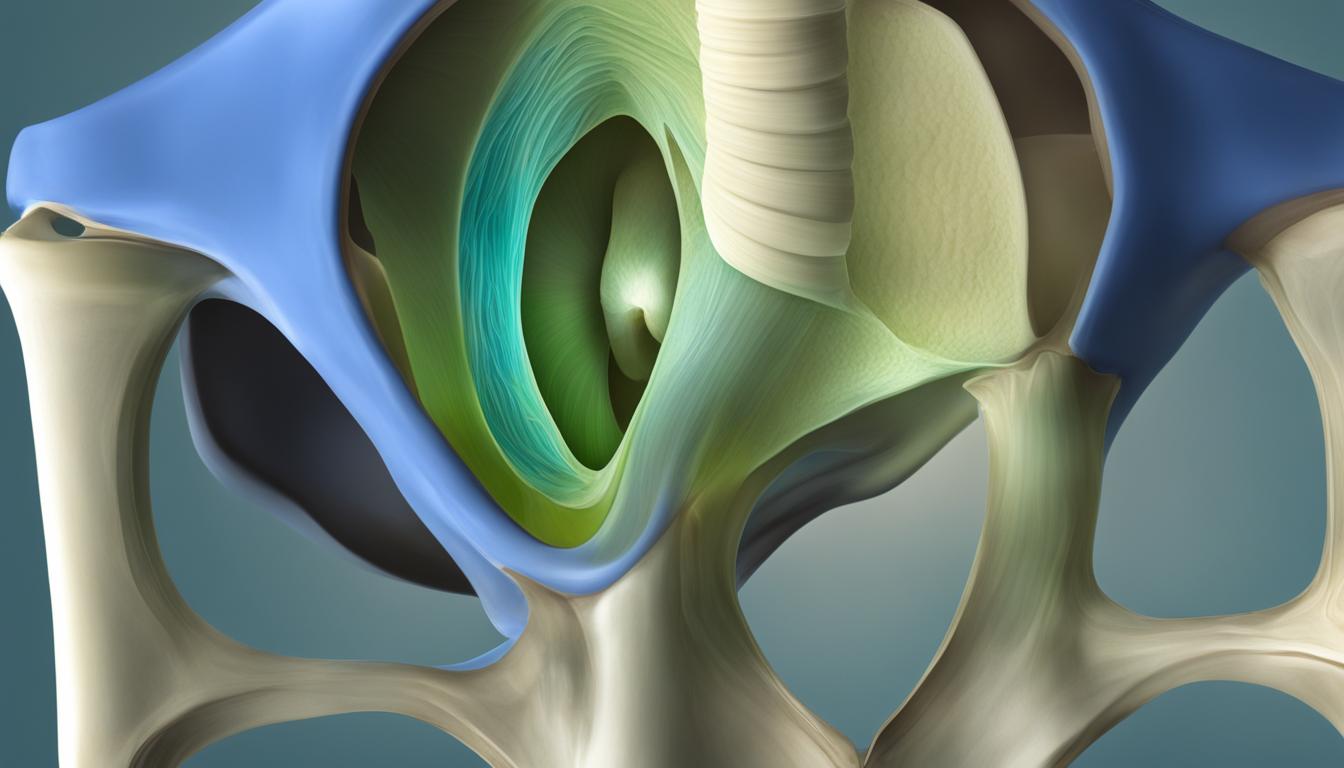
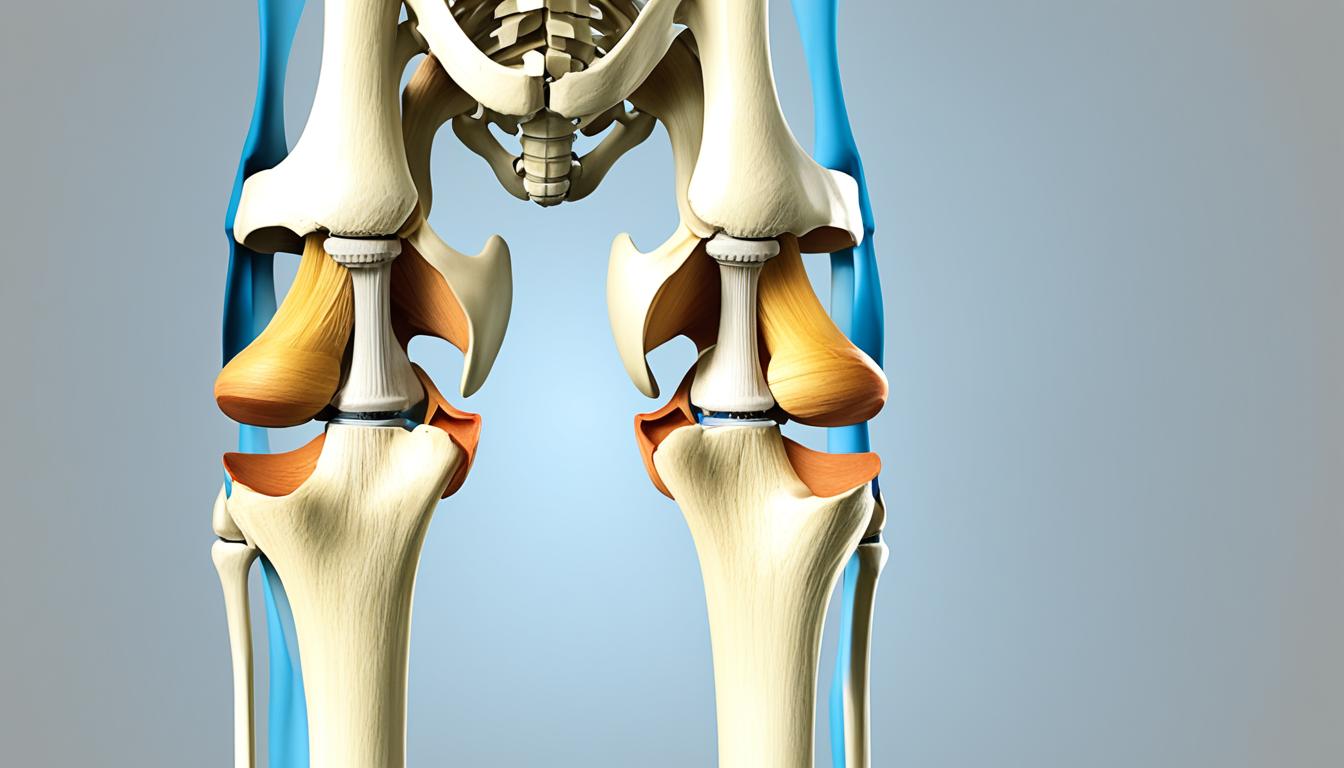
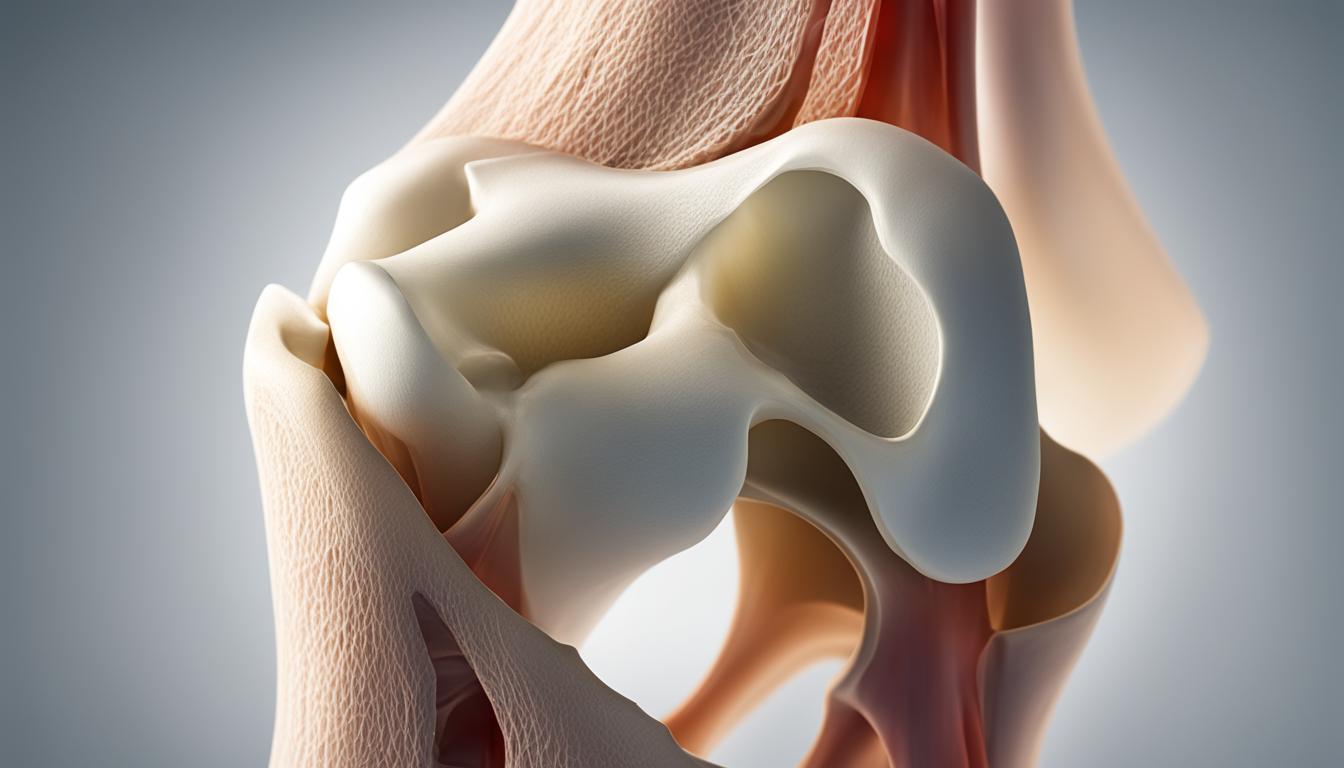
Did you know that patella alta, or a high-riding patella, can lead to patellofemoral dysfunction and cause debilitating pain in the knee? This abnormal condition, where the patella sits higher on the femur, affects a significant number of individuals worldwide. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for patella alta, as well as delve into key research on this condition. Whether you or someone you know is dealing with this condition, understanding patella alta is crucial for effective management.
Before we dive deeper, let’s define patella alta. It is characterized by an abnormally high patella in relation to the femur. Radiographic measurements, such as the Caton-Deschamps index, Insall-Salvati index, Blackburne-Peel index, and patellotrochlear index, are used to diagnose patella alta. Typically, a Caton-Deschamps index of >1.2 to >1.3 confirms the presence of patella alta.
Clinical Presentation and Symptoms of Patella Alta
When it comes to patella alta, the main clinical presentation is the instability of the patella, which often leads to patellofemoral pain and a sensation of the knee giving way. Patients with patella alta typically experience pain after direct contact or sudden changes in direction. The pain is commonly felt in the anterior aspect of the knee.
Increased physical activity can exacerbate the anterior knee pain associated with patella alta. Activities such as going up and down stairs or squatting may worsen the symptoms. Patients with patella alta may also experience difficulty with activities that require knee flexion, such as prolonged sitting or driving for long periods.
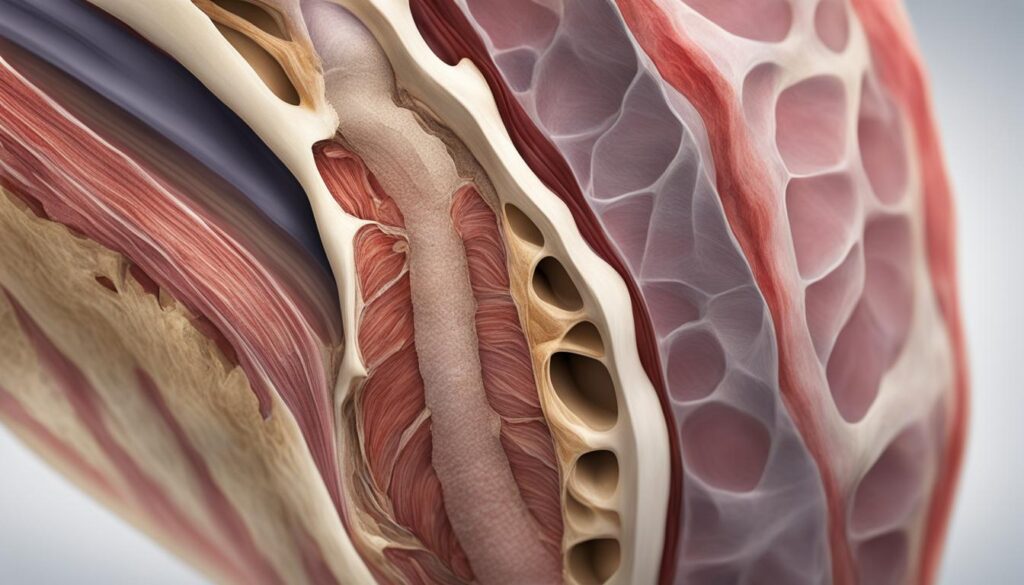
Aside from patellofemoral pain, patella alta is also associated with other knee conditions. Chondromalacia, characterized by softening and degeneration of the articular surface of the patella, is commonly observed in patients with patella alta. Additionally, individuals with patella alta have an increased risk of developing patellar osteoarthritis over time.
Quote: “Patients with patella alta often report a feeling of instability and pain in the front of the knee. It is essential to assess the patellar height and consider it as a potential cause of their symptoms.”
Presentation and Symptoms Summary:
- Main symptom: Patellar instability leading to patellofemoral pain and a sensation of the knee giving way.
- Pain worsens after direct contact or sudden changes in direction.
- Increased physical activity exacerbates anterior knee pain.
- Difficulty with activities such as going up and down stairs or squatting.
- Association with chondromalacia and increased risk of patellar osteoarthritis.

| Patella Alta Symptoms | Clinical Presentation |
|---|---|
| Instability of the patella | Patients may experience a sense of the knee “giving way” due to the patella’s abnormal position on the femur. |
| Anterior knee pain | Pain is typically felt in the front of the knee and is aggravated by physical activity or movements that stress the patellofemoral joint. |
| Chondromalacia | Softening and degeneration of the articular surface of the patella, often present in individuals with patella alta. |
| Increased risk of patellar osteoarthritis | Patella alta is associated with a higher likelihood of developing osteoarthritis in the patellar joint over time. |
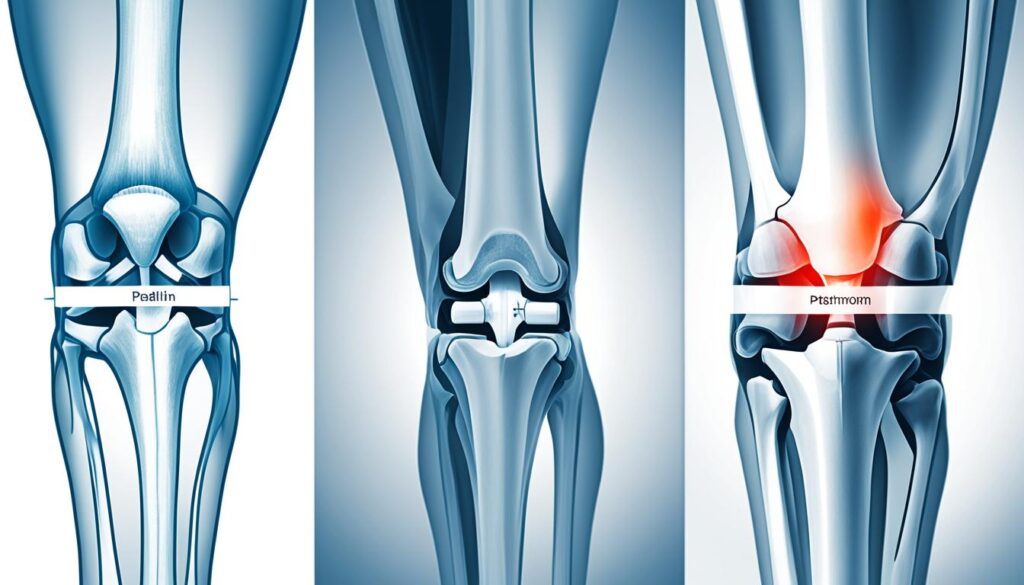
Diagnosis of Patella Alta
Patella alta, a condition characterized by an abnormally high patella, can be diagnosed through various imaging techniques and measurements of radiographic ratios. These diagnostic procedures provide valuable insights into the positioning and relationship of the patella, enabling healthcare professionals to confirm the presence of patella alta.
Imaging techniques such as lateral radiographs and MRI scans play a crucial role in the diagnosis of patella alta. These imaging modalities allow for a detailed assessment of the patellar alignment and aid in identifying any abnormalities or deviations.
Additionally, specific radiographic ratios are commonly used to determine the presence of patella alta. The Insall-Salvati ratio, Caton-Deschamps index, and Blackburne-Peel index are among the most utilized measurements. These ratios assess the length of the patellar tendon, the length of the patella, and the patella’s position relative to the tibial plateau.
An A/B ratio greater than 1.2 for the Insall-Salvati index or a ratio greater than 1.3 for the Caton-Deschamps index confirms the diagnosis of patella alta.
By employing these diagnostic procedures, healthcare professionals can accurately diagnose patella alta, facilitating the development of an appropriate treatment plan.
| Diagnostic Procedure | Description |
|---|---|
| Lateral Radiographs | Utilizes X-ray imaging to visualize the patellar alignment and identify potential abnormalities. |
| MRI Scans | Provides detailed images of the knee joint, allowing for a comprehensive assessment. |
| Insall-Salvati Ratio | Compares the length of the patellar tendon to the length of the patella to determine patella alta. |
| Caton-Deschamps Index | Evaluates the patellar position relative to the tibial plateau to confirm patella alta. |
| Blackburne-Peel Index | Measures the relationship between the patella, femoral condyles, and tibial plateau. |
Medical and Physical Therapy Management of Patella Alta
The treatment of patella alta aims to reduce pain and instability while restoring full knee function. In most cases, non-operative treatment options are recommended as the initial approach. These options include:
- Rest: Allowing the knee to recover and heal by avoiding activities that aggravate the condition.
- Strengthening exercises: Targeted exercises for the knee and surrounding muscles can help improve stability and support the patella.
- Physical therapy: A comprehensive physical therapy program can help alleviate pain, improve joint range of motion, and strengthen the muscles around the knee.
- Patellar taping: Application of specialized tape to the knee can provide additional support and stability to the patella.
- Ice packs: Cold therapy can help reduce pain and inflammation.
- Knee braces: The use of knee braces can provide external support to the knee joint and help relieve pain and instability.
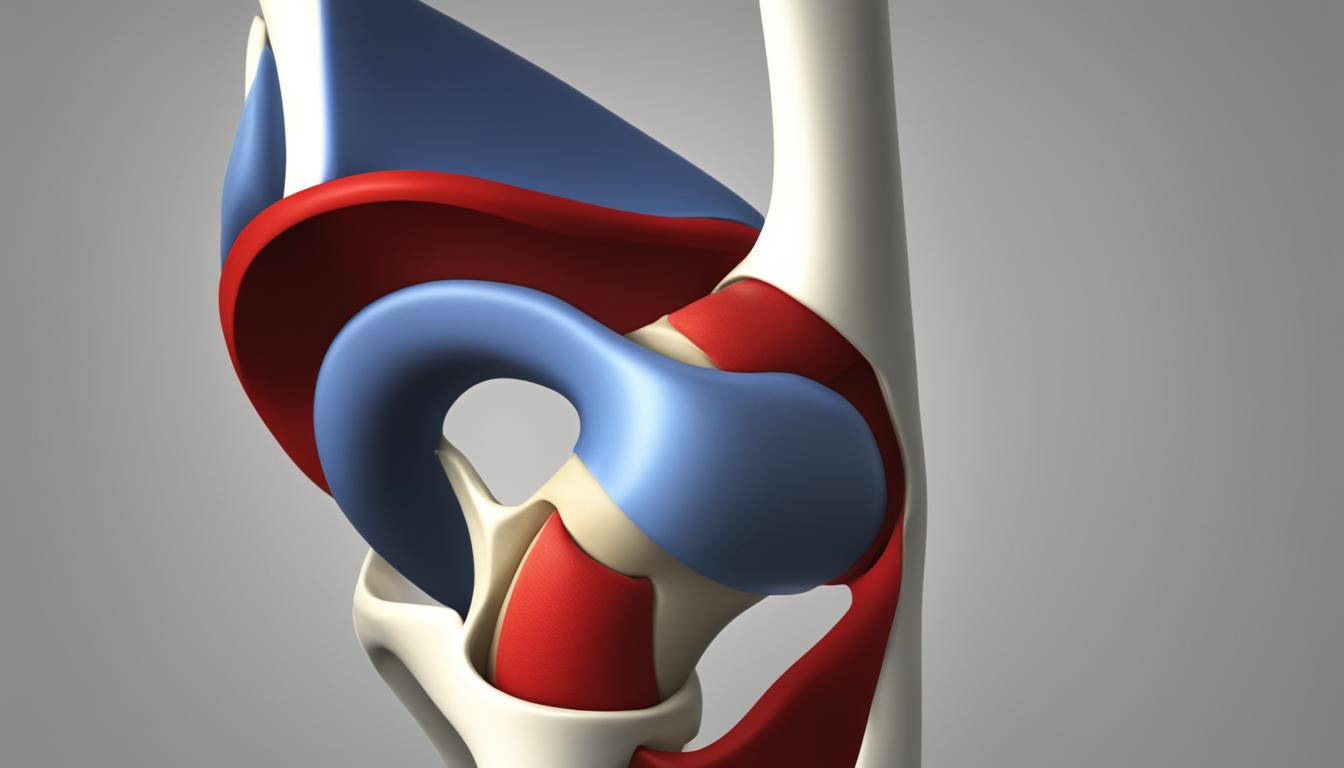
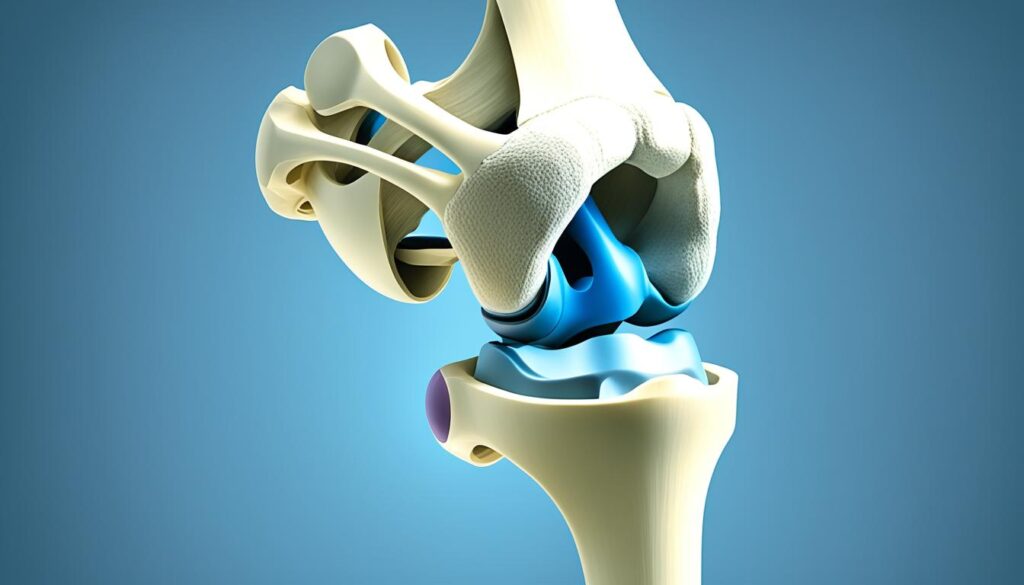
In severe cases of patella alta or when conservative treatment fails to provide relief, surgical options may be considered. These can include:
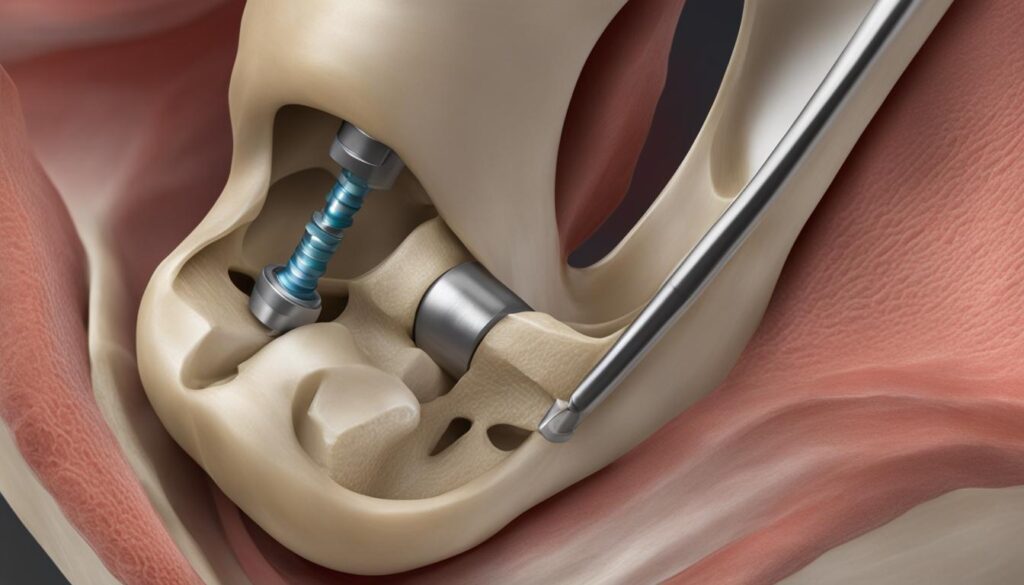
- Tibial tuberosity osteotomy: This surgical procedure involves repositioning the patellar tendon attachment to correct the high-riding patella and restore proper alignment.
- Lateral release: In this procedure, tight structures on the outside of the knee are released to help realign the patella and reduce associated symptoms.
Following surgery, the patient typically undergoes a period of recovery and rehabilitation, which may include:
- Wearing a knee brace: A brace is often worn to provide support and protect the knee during the healing process.
- Using crutches: Crutches may be used to assist with walking and mobility while weight-bearing on the affected leg is restricted.
- Participating in physical therapy: A structured physical therapy program is essential to regain strength, range of motion, and functional abilities. This includes exercises targeting the knee and surrounding musculature to restore optimal function.

Physical Therapy Management
Physical therapy plays a crucial role in managing patella alta. The goals of physical therapy management include:
- Reducing pain and inflammation
- Improving joint mobility
- Strengthening the muscles around the knee, particularly the quadriceps and the hip abductors and external rotators
- Improving lower limb alignment and patellar tracking
- Enhancing proprioception and neuromuscular control
“Physical therapy is a key component in the comprehensive management of patella alta. The focused exercises and therapeutic techniques help address muscle imbalances, improve knee control, and optimize knee function for individuals with this condition.”
Incorporating a multidisciplinary approach, physical therapists work closely with patients to develop personalized treatment plans that address their specific needs and goals. This may involve a combination of therapeutic exercises, manual therapy techniques, modalities, and patient education.
Key Research on Patella Alta
In the field of patella alta, extensive research has been conducted to explore its association with various conditions such as patellofemoral pain, chondromalacia, and knee osteoarthritis. These studies provide valuable insights into the biomechanics of patella alta and its impact on patellofemoral joint contact stress.
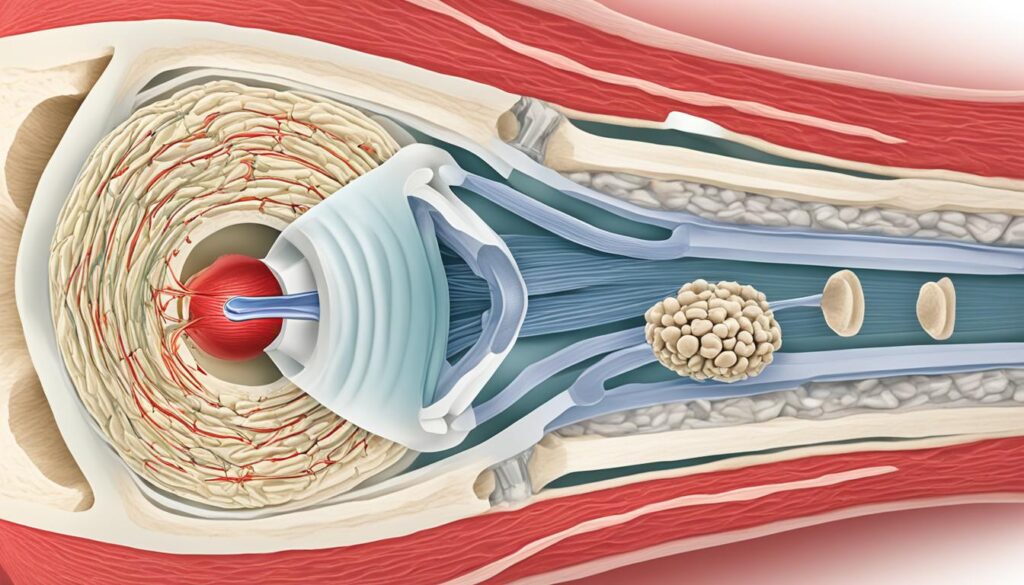
One area of research focuses on the effectiveness of taping methods and knee bracing in managing the pain associated with patella alta. Some studies have suggested that these interventions can be beneficial by increasing the contact area between the patella and the femur in the patellofemoral joint.
Research has shown that taping techniques and braces have the potential to optimize patellofemoral joint mechanics and reduce symptoms in individuals with patella alta.
However, while these initial findings are promising, further research is still necessary to establish the optimal treatment approach for patella alta. Additional studies are needed to investigate the long-term effects of taping methods and bracing, as well as to explore other potential treatment modalities.
By expanding our understanding of patella alta through ongoing research, we can continue to enhance the management and treatment strategies for individuals affected by this condition, ultimately improving their overall quality of life.
Current Research Studies on Patella Alta
Here are some recent research studies that are contributing to our knowledge and understanding of patella alta:
- A Comparative Analysis of Patella Alta and Patella Baja: A Biomechanical Study.
- Association of Patella Alta with Cartilage Lesions in the Patellofemoral Joint.
- The Effect of Taping Techniques on Patellofemoral Joint Contact Area in Patella Alta: A Randomized Controlled Trial.
- Long-Term Outcomes of Surgical Management for Patella Alta: A Retrospective Cohort Study.
| Study | Objective | Methods | Findings |
|---|---|---|---|
| A Comparative Analysis of Patella Alta and Patella Baja: A Biomechanical Study | To compare the biomechanics of patella alta and patella baja and evaluate their respective effects on patellofemoral joint contact stress. | Biomechanical modeling and simulations using computer-aided design software. | Patella alta was associated with increased patellofemoral joint contact stress compared to normal patella position (patella baja). |
| Association of Patella Alta with Cartilage Lesions in the Patellofemoral Joint | To investigate the relationship between patella alta and the presence of cartilage lesions in the patellofemoral joint. | Retrospective analysis of MRI scans and medical records of patients with patella alta. | Patella alta was significantly associated with a higher prevalence of cartilage lesions in the patellofemoral joint. |
| The Effect of Taping Techniques on Patellofemoral Joint Contact Area in Patella Alta: A Randomized Controlled Trial | To assess the impact of taping techniques on patellofemoral joint contact area in individuals with patella alta and evaluate their effects on pain and function. | Randomized controlled trial comparing different taping techniques and a control group. | Taping techniques significantly increased the patellofemoral joint contact area in the patella alta group, leading to improved pain and function. |
| Long-Term Outcomes of Surgical Management for Patella Alta: A Retrospective Cohort Study | To evaluate the long-term outcomes of surgical management options for patella alta and determine their effectiveness in improving pain, function, and patient satisfaction. | Retrospective analysis of patient data and follow-up questionnaires. | Surgical management, including tibial tuberosity osteotomy and lateral release, showed favorable long-term outcomes in terms of pain relief, functional improvement, and high patient satisfaction rates. |
Conclusion
Patella alta, characterized by a higher positioning of the patella on the femur, is an abnormal condition that can cause instability and an increased risk of patellofemoral pain. While the exact cause of patella alta is not fully understood, it is believed to be associated with abnormally long patellar tendons. Diagnosis of patella alta is based on radiographic measurements, such as the Insall-Salvati ratio and the Caton-Deschamps index.
When it comes to the management of patella alta, non-operative approaches are often the initial line of treatment. Physical therapy, taping techniques, and knee braces can help reduce pain and improve knee function. In severe cases or when conservative measures fail, surgical interventions like tibial tuberosity osteotomy or lateral release may be considered to address the underlying issue.
Although significant progress has been made in understanding patella alta, further research is crucial to enhance our knowledge and develop more effective management strategies. By delving deeper into the biomechanics and associated pathologies of patella alta, we can optimize treatment approaches and ultimately improve patient outcomes for this condition.
FAQ
What is patella alta?
Patella alta, also known as high-riding patella, refers to an abnormally high position of the patella (kneecap) in relation to the femur (thigh bone). It is defined by radiographic measurements, such as the Caton-Deschamps index, Insall-Salvati index, Blackburne-Peel index, and patellotrochlear index.
What are the causes and symptoms of patella alta?
The exact cause of patella alta is not fully understood, but it can be congenital or a result of sports injuries. Common symptoms include patellofemoral pain, instability of the patella, a sensation of the knee giving way, and pain worsened by physical activities such as squatting or going up and down stairs.
How is patella alta diagnosed?
Patella alta is diagnosed through imaging techniques, such as lateral radiographs and MRI scans. Several radiographic ratios, including the Insall-Salvati ratio, Caton-Deschamps index, and Blackburne-Peel index, are used to determine the presence of patella alta.
What are the treatment options for patella alta?
Non-operative treatment options for patella alta include rest, strengthening exercises for the knee and surrounding muscles, physical therapy, patellar taping, ice packs, and knee braces. In severe cases or when conservative treatment fails, surgical options such as tibial tuberosity osteotomy or lateral release may be considered.
What research has been done on patella alta?
Research on patella alta has focused on its association with patellofemoral pain, chondromalacia, and knee osteoarthritis. Studies have investigated the biomechanics of patella alta and its effects on patellofemoral joint contact stress. Some research suggests that taping methods and bracing can be effective in managing pain associated with patella alta.
Is there a conclusion on patella alta?
While further research is needed to determine the optimal treatment approach for patella alta, current medical and physical therapy management strategies aim to reduce pain, restore knee function, and improve knee stability. Understanding the causes, symptoms, and diagnostic methods for patella alta is crucial in providing appropriate care for individuals with this condition.