What if the hours you spend sitting in traffic aren’t just draining your energy—they’re quietly sabotaging your mobility? For millions of Americans, extended time behind the wheel leads to stiffness, aching joints, and reduced flexibility. The good news: small adjustments to your routine can make a big difference.
We’ve developed targeted movements that work within tight spaces, whether you’re stuck in gridlock or cruising cross-country. These techniques focus on improving circulation while maintaining proper alignment—critical for preventing discomfort during long drives. Our methods are backed by physical therapy principles, adapted specifically for vehicle environments.
Regular movement isn’t just about comfort—it’s about safety. Stagnant blood flow during prolonged sitting increases health risks many drivers overlook. Through simple stretches and isometric holds, you can maintain joint health without leaving your seat.
Key Takeaways
- Combat stiffness with seated stretches designed for limited space
- Improve circulation through subtle muscle engagement techniques
- Reduce pressure on joints with proper sitting alignment tips
- Prevent travel-related discomfort with timed movement breaks
- Enhance mobility without compromising driving safety
Understanding Knee Pain on the Road
Joint discomfort during travel isn’t inevitable—it’s a warning sign. Hours spent in fixed positions compress sensitive tissues and slow blood flow. Dr. Harbinder Chadha from Sharp Chula Vista Medical Center warns:
“When blood moves too slowly through your veins, it can be the source of a stroke or heart attack.”
Common Causes and Triggers
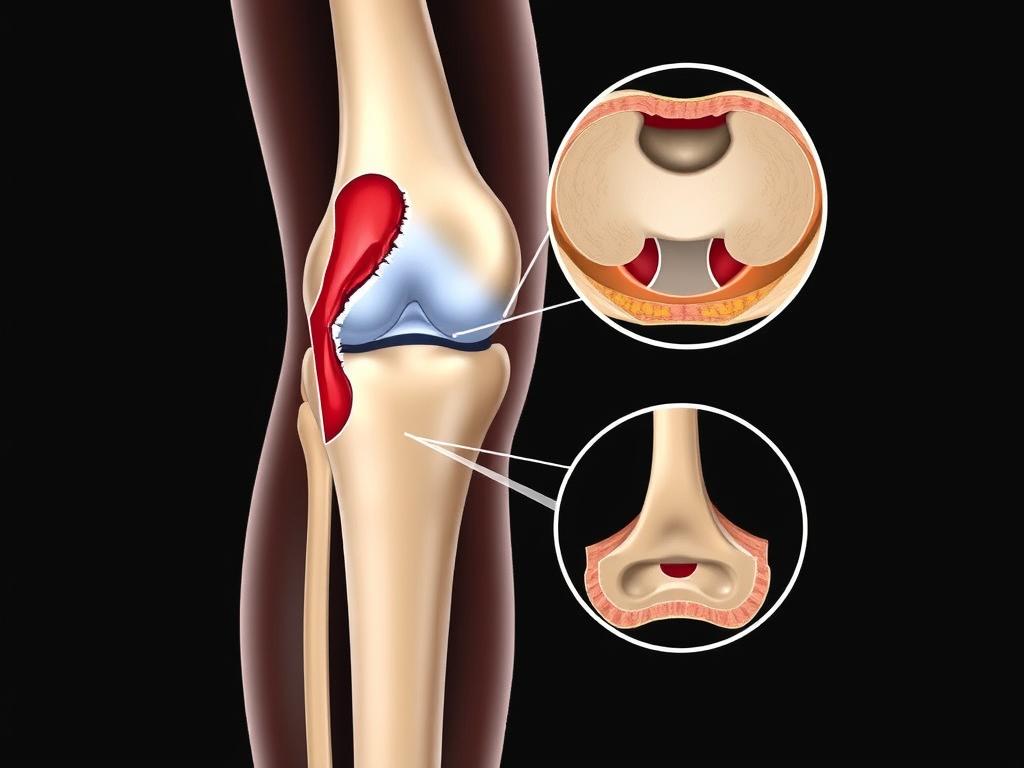
Limited legroom forces joints into unnatural angles. Seat cushions that slope backward increase pressure on the kneecap area. Without regular position changes, synovial fluid—our joints’ natural lubricant—can’t circulate properly.
Three factors worsen travel-related discomfort:
- Dashboard heights that limit leg extension
- Frequent accelerator movements straining quadriceps
- Air conditioning drying joint fluid
How Prolonged Sitting Affects Joint Health
Bent knees for extended periods starve cartilage of nutrients. This rubbery tissue relies on motion to absorb synovial fluid. Stagnation leads to stiffness and eventual injury risks.
Compensatory movements develop when drivers adjust posture to ease discomfort. These shifts transfer strain to hip muscles and lower back. Over time, this cascade effect can create chronic issues beyond initial knee pain.
Benefits of Car Exercises for Knee Pain

Your vehicle could become an unexpected ally in maintaining joint health. Research confirms that gentle motion acts like natural lubrication for stiff joints—critical for drivers managing discomfort. Therapeutic movements stimulate synovial fluid production, which nourishes cartilage lacking direct blood supply.
Reducing Stiffness and Enhancing Mobility
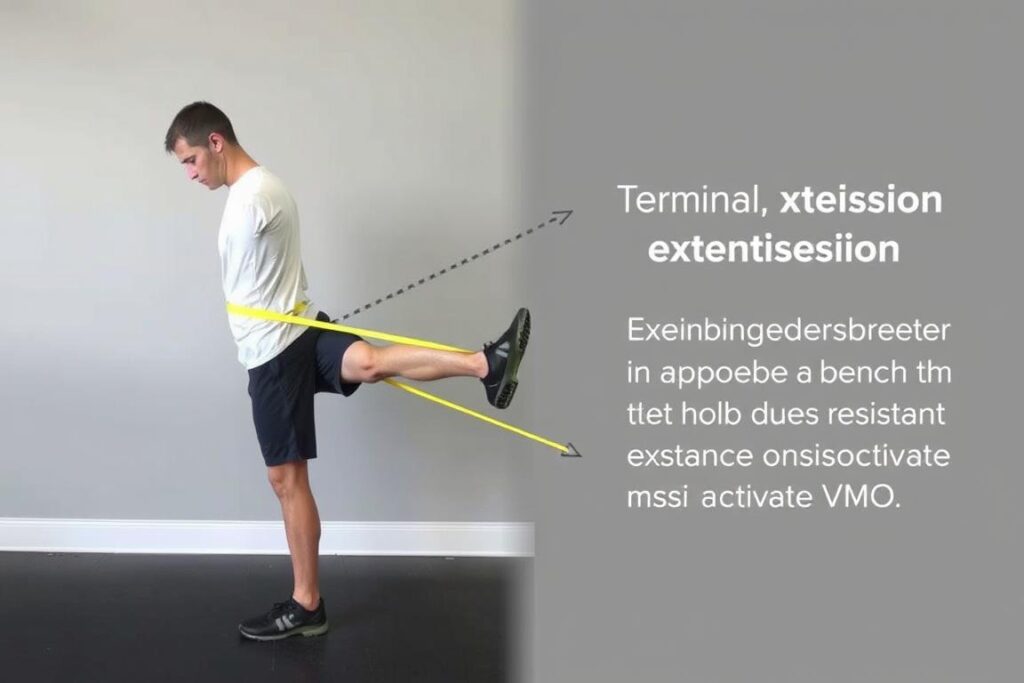
Strategic movements during rest stops or traffic delays combat two major issues. First, they pump nutrient-rich fluids into connective tissues. Second, they prevent muscle atrophy caused by prolonged sitting. Quadriceps and hamstrings stay engaged, reducing strain on vulnerable joints.
Regular motion breaks deliver three key advantages:
- Improved circulation flushes out inflammatory waste products
- Controlled stretches maintain functional range of motion
- Active muscle groups stabilize knees during position changes
Psychological benefits are equally significant. Taking charge of discomfort reduces travel anxiety. A 2021 Journal of Orthopedic Research study found drivers who performed seated movements reported 34% less stiffness during long trips.
Consistency breaks the stiffness cycle. Brief activity every 45 minutes prevents joints from locking into fixed positions. This approach keeps tissues responsive, making exit-and-enter movements safer when resuming travel.
Best car exercises for knee pain
Navigating joint care during road trips requires smart spatial awareness. Limited cabin space demands precise movements to protect sensitive areas while maintaining blood flow. Always begin by adjusting your seat to allow fist-sized gaps between knees and dashboard surfaces.
Movement Safety in Tight Quarters
Stop immediately if you feel sharp discomfort. Our approach focuses on micro-movements that work with your vehicle’s layout rather than against it. Use this comparison table to optimize your setup:
| Safe Position | Risky Position | Why It Matters |
|---|---|---|
| Hips higher than knees | Slouched seating | Reduces patellar pressure |
| Feet flat on floor mats | Legs fully extended | Maintains circulation |
| Hands on steering wheel | Arms stretched forward | Supports upper body stability |
Three essential rules for confined spaces:
- Park completely before attempting leg movements
- Use door handles for upper body support during stretches
- Limit motion range to 50% of normal capacity
Cold joints need gradual activation. Start with ankle circles before progressing to knee-friendly motions. Those recovering from injuries should consult specialists before trying new techniques. Remember: discomfort during travel often signals the need for professional guidance, not just temporary fixes.
Practical Car Stretches and Movements
Drivers can actively combat stiffness with strategic stretches designed for vehicle interiors. These movements focus on gentle engagement without compromising posture or safety. Let’s explore three adaptable techniques that work within seatbelt confines.
Recumbent Leg Lifts
Adjust your seat to a 45-degree angle. Slowly raise one straightened leg until it hovers 6 inches above the floor. Hold for 5 seconds while engaging thigh muscles, then lower with control. Alternate legs for 8 repetitions. This targets quadriceps without stressing joints.
Knee-to-Chest Technique
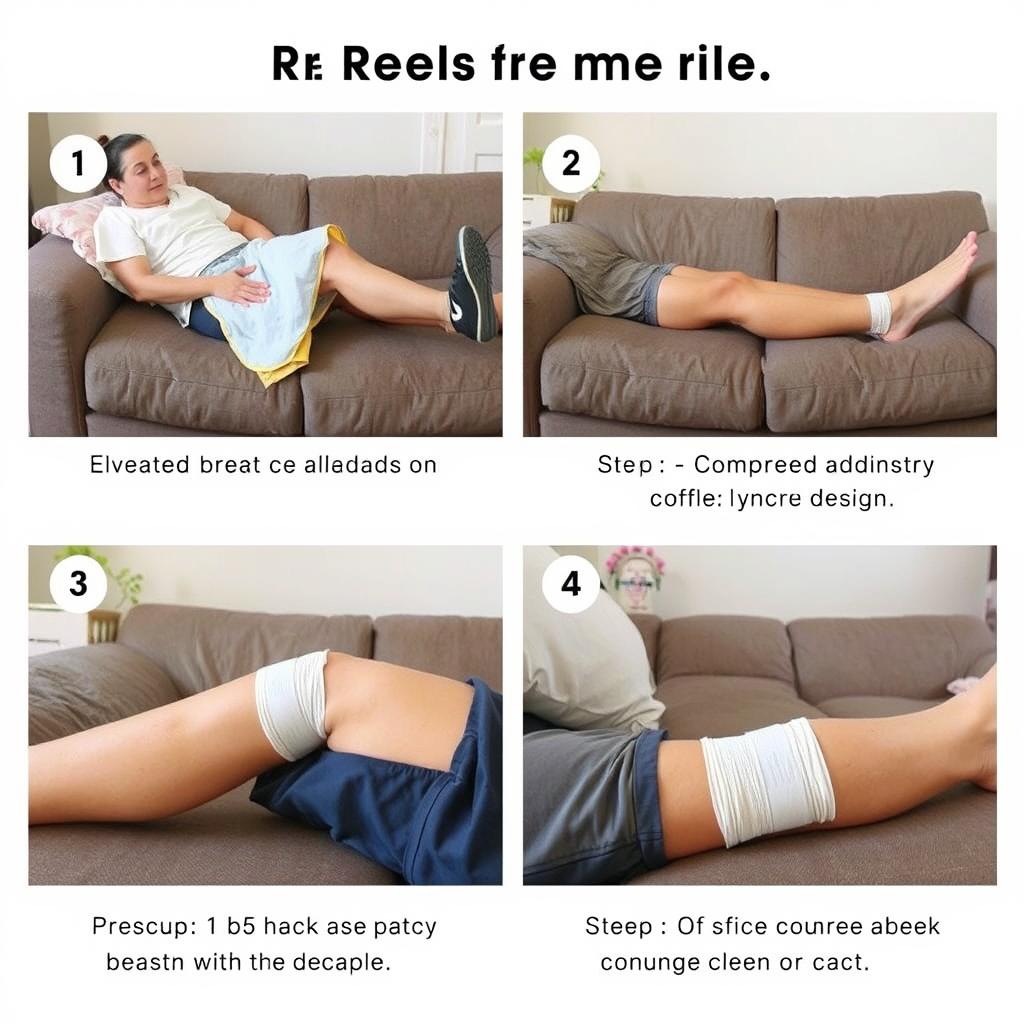
While parked, recline slightly and grasp one leg below the kneecap. Gently pull toward your torso until you feel a stretch in the hip area. Maintain this position for 10 seconds before releasing. Repeat 3 times per side to improve circulation.
Seated Cycling Motion
With feet flat on floor mats, lift one foot and make small circular motions. Aim for 15 rotations clockwise, then reverse direction. Keep movements controlled to enhance joint flexibility. This mimics natural synovial fluid distribution.
| Proper Form | Common Errors | Impact |
|---|---|---|
| Shoulders relaxed | Hunched posture | Reduces neck strain |
| Core engaged | Arching lower back | Protects spinal discs |
| Breathing steady | Holding breath | Improves oxygen flow |
For compact vehicles, modify stretches by using the steering wheel for upper body support. Always complete movements within your comfortable range – forcing extensions risks injury. Those with existing conditions should consult a physical therapist before starting new routines.
Expert Tips for Safe and Effective Exercises
Orthopedic specialists agree: smart movement strategies transform travel discomfort into opportunities for joint care. Regular activity breaks combat stagnation while keeping drivers alert and responsive. Let’s explore proven methods endorsed by medical professionals.
Actionable Recommendations from Medical Authorities
Dr. Harbinder Chadha emphasizes timed interventions during long trips: “Perform gentle movements every 45-60 minutes to maintain circulation.” His research-backed approach includes two key techniques:
- Ankle pumps: Alternate pointing toes downward and upward 20 times per foot. This simple motion reduces clot risks by 58% according to vascular studies
- Seated knee lifts: Engage core muscles while pulling knees toward chest. Hold for 10 seconds to activate hip flexors without straining joints
| Technique | Common Mistakes | Optimal Approach |
|---|---|---|
| Ankle rotations | Rushing through motions | 3-second holds per direction |
| Knee extensions | Overarching lower back | Support with seat cushion |
| Hip stretches | Twisting torso | Use headrest for alignment |
Timing matters more than intensity. Brief sessions every hour prove more effective than hour-long stretches. For those recovering from injury, modified versions using steering wheel support prevent excessive strain.
Orthopedic teams stress consistency over perfection. Even imperfect movements boost blood flow better than complete stillness. Pair these exercises with proper hydration to maintain joint lubrication throughout your journey.
Integrating Car Exercises into Your Routine
Consistent movement transforms commuting from joint-stiffening chore to active recovery time. We’ve designed adaptable methods that sync with common driving patterns, ensuring joint care becomes second nature behind the wheel.
Timing matters more than duration. Brief 2-3 minute sessions every hour maintain circulation better than occasional long stretches. Link movements to natural driving pauses—red lights become opportunities for foot pumps, while rest stops invite full-body stretches.
Phased Approach for Lasting Results
Tailor activities to your journey’s stages:
| Pre-Drive Prep | Mid-Journey Relief | Post-Drive Recovery |
|---|---|---|
| Ankle alphabet tracing | Seated leg extensions | Standing calf raises |
| Toe towel scrunches | Foot arch presses | Step-back lunges |
| Knee-cap glides | Heel slides | Hip hinge stretches |
Urban drivers can use traffic signals as movement reminders. Try lifting alternate heels during stoplights or rotating ankles while idling. Highway travelers benefit from shoulder-check stretches—turn your head fully while gently pressing corresponding foot into floor mat.
“Two-minute movement breaks every hour reduce clot risks by 40% compared to stationary sitting,” notes Dr. Harbinder Chadha. “It’s about working with your travel rhythm, not against it.”
Position adjustments enhance effectiveness. Slide seat backward slightly for leg extensions. Use lumbar support to maintain neutral spine during foot movements. Those with automatic transmissions can practice toe spreads during gear changes.
Using Physical Therapy for Long-Term Knee Health
Contrary to old beliefs, your knees grow stronger through strategic challenges rather than avoidance. A landmark study of 115,000 adults revealed recreational runners develop knee osteoarthritis at one-third the rate of sedentary individuals. This proves movement serves as natural medicine for joint preservation.
“Your body adapts to stresses when given gradual, systematic challenges. The ‘sweet spot’ exists where movement nourishes without overwhelming.”
This principle transforms how we approach travel-related discomfort.
Building Strength Gradually Over Time
Three foundational strategies create lasting results:
- Progressive loading: Start with 5-minute seated leg lifts, increasing duration weekly
- Response tracking: Use a 1-10 scale to monitor stiffness 2 hours post-exercise
- Functional integration: Apply car-based techniques to desk work or household tasks
Create personalized benchmarks using this progression guide:
| Week | Focus | Success Marker |
|---|---|---|
| 1-2 | Pain-free motion | 20% reduction in travel stiffness |
| 3-4 | Muscle endurance | Tripled repetition capacity |
| 5+ | Weight management | Easier car entry/exit motions |
Those managing injuries should pair car exercises with aquatic therapy. Water’s buoyancy reduces joint impact while building supportive muscles. Remember: improved health stems from consistency, not perfection. Even minimal daily efforts compound into significant mobility gains.
Conclusion
Your daily commute holds hidden potential for maintaining joint wellness. Through strategic movements tailored to confined spaces, drivers can transform travel time into active recovery sessions. Consistent effort with these techniques helps maintain fluid circulation while reducing pressure on sensitive areas.
Focus on gentle stretches that work with your vehicle’s layout. Adjustments like proper hip alignment and mindful feet placement make movements safer and more effective. Remember: brief sessions every hour yield better results than occasional intense efforts.
These methods adapt to any seating position or vehicle type. Compact cars become mobility studios through creative ankle rotations and seated leg lifts. Larger SUVs allow modified side stretches using door handles for support.
While these strategies help manage discomfort, they complement—not replace—professional care. Persistent issues require medical evaluation. Pair your travel routine with balanced nutrition and regular activity for lasting joint health.
Every journey becomes an opportunity when you prioritize movement. Start small, stay consistent, and let your vehicle support your wellness goals—one mindful stretch at a time.
FAQ
How does prolonged sitting during drives impact knee health?
Remaining seated for extended periods limits blood flow and reduces joint lubrication, leading to stiffness. Tight leg muscles and restricted motion can strain ligaments, worsening discomfort over time. We recommend shifting positions regularly and incorporating stretches.
What movements are safe to perform in a car seat without causing injury?
Focus on low-impact motions like ankle pumps, gentle leg extensions, and seated marches. Keep movements controlled, avoid sudden twists, and use the steering wheel or seat for balance if needed. Always prioritize comfort over intensity.
Can these activities actually prevent stiffness during long trips?
Yes! Consistent micro-movements – like heel slides or knee-to-chest stretches – maintain circulation and flexibility. Pair them with brief stops to walk every 1-2 hours for optimal results. Hydration also supports joint lubrication.
Which stretches target thigh muscles effectively in confined spaces?
Recumbent leg lifts engage quadriceps without requiring standing space. For hamstrings, lean forward slightly while seated and extend one leg with toes pointed upward. Hold each stretch for 15-20 seconds, repeating 3-5 times per side.
Do orthopedic specialists endorse in-car exercises for chronic discomfort?
Many recommend them as supplementary practices. Dr. Sarah Thompson from the Mayo Clinic notes, “Gentle motion breaks counteract sedentary strain. However, consult a professional if pain persists beyond driving sessions.”
How can commuters consistently integrate these routines?
Link exercises to routine triggers – perform ankle circles at red lights or do seated calf raises during phone calls. Set reminders on navigation apps to prompt hourly movement sessions.
Can physical therapy techniques complement car-based workouts?
Absolutely. Resistance bands stored in glove compartments allow isometric strengthening. Post-drive routines using PT-prescribed exercises build endurance, addressing root causes like weak hip stabilizers or tight IT bands.