Prevention Strategies for Knee Ligament Injuries: Professional Tips
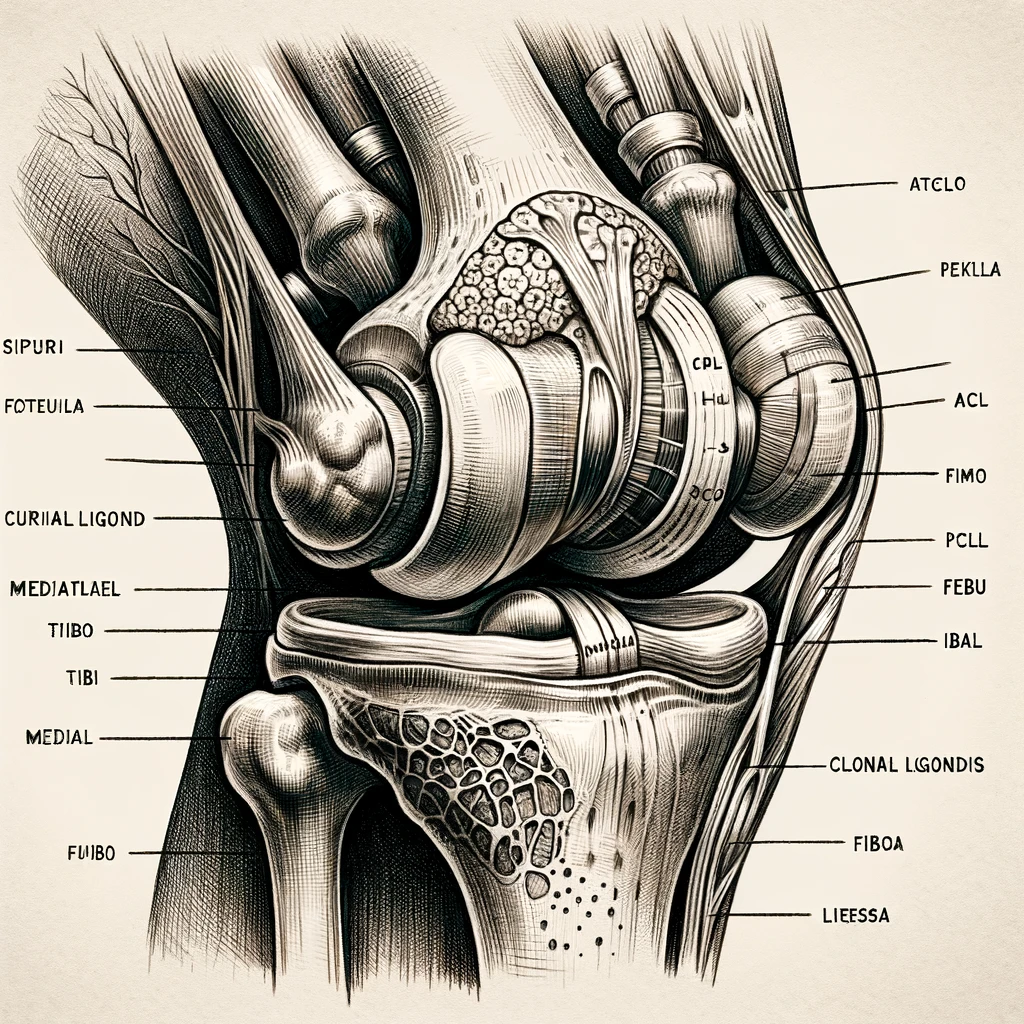
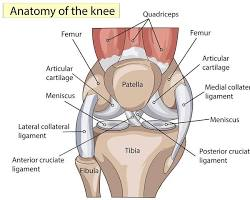
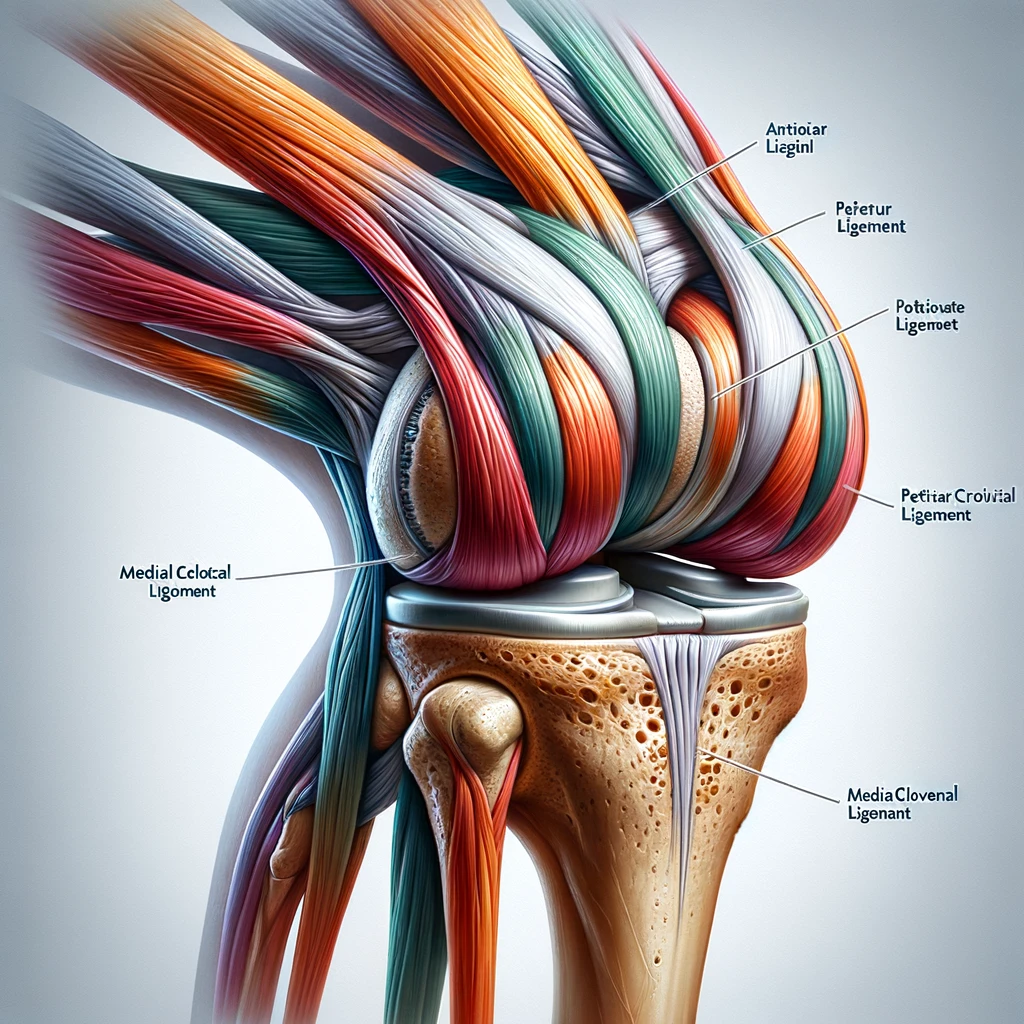
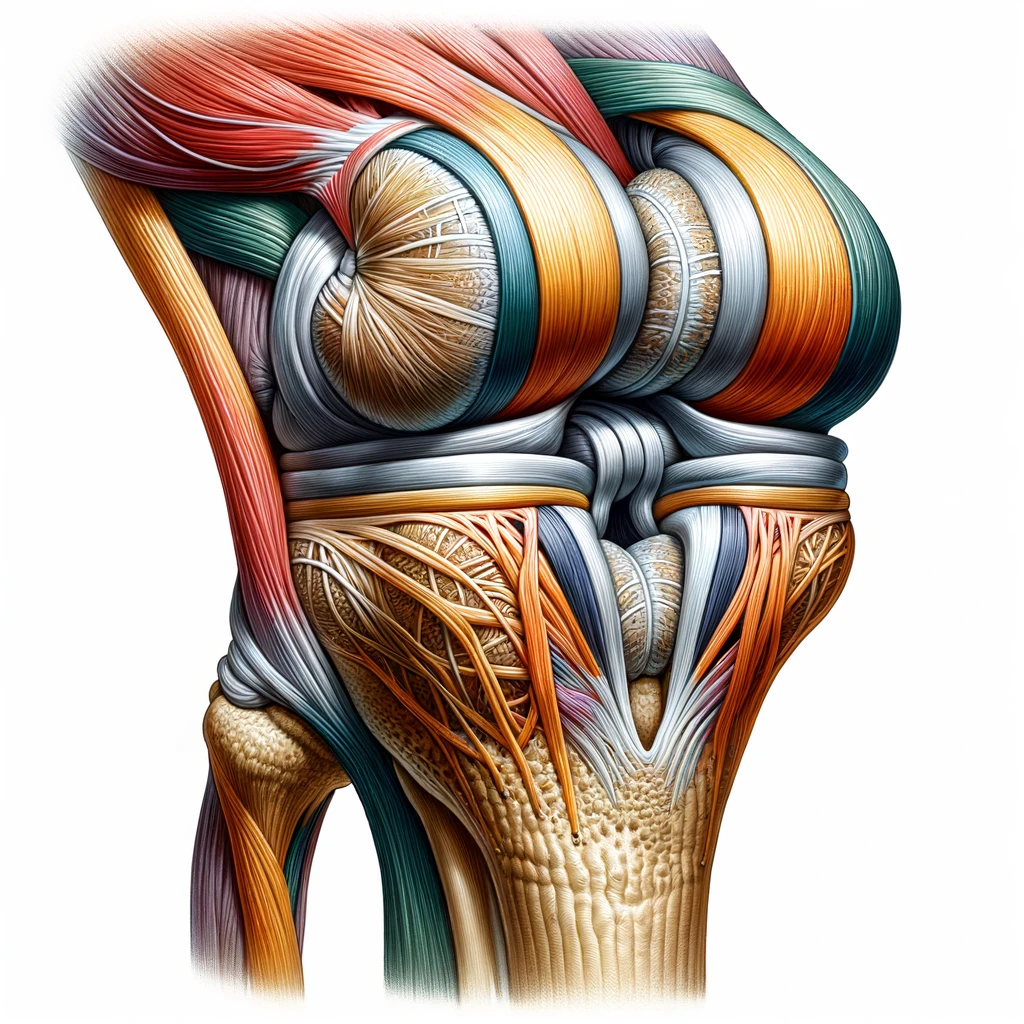
Knee ligament injuries are common among athletes and can be a frustrating setback for anyone who enjoys an active lifestyle. The knee joint is one of the largest and most complex joints in the body, making it vulnerable to various types of injuries. Understanding and identifying knee ligament injuries is crucial to prevent further damage and promote quick recovery.

The most common knee ligament injuries are the anterior cruciate ligament (ACL), medial collateral ligament (MCL), posterior cruciate ligament (PCL), and lateral collateral ligament (LCL). These injuries can occur due to direct trauma, such as contusions and strains, or from indirect trauma, such as sudden changes in direction. Symptoms of knee ligament injuries include pain, swelling, inflammation, and joint laxity. In this article, we will discuss five prevention strategies for knee ligament injuries to help maintain knee stability and prevent knee instability.
professional tips for prevention strategies to help avoid knee ligament injuries:
| Category | Tips |
|---|---|
| Strength & Flexibility Training | – Emphasize hamstring, glute, quad, hip & core exercises<br>- Ensure muscle imbalances are addressed<br>- Use proper form/technique to prevent overstress |
| Movement Control & Balance | – Practice proper landing mechanics when jumping <br>- Enhance proprioception & body control<br>- Integrate deceleration drills |
| Equipment & Environment | – Wear supportive & appropriate footwear <br>- Tape or brace vulnerable knees if needed <br>- Ensure safe, even playing surfaces |
| Loading & Recovery | – Follow loading guidelines for ramping up intensity<br>- Avoid aggressive pivoting until tissues adapted<br>- Schedule adequate rest periods between sessions |
| Body Composition & Nutrition | – Prevent muscle loss during injury layoffs<br>- Maintain healthy BMI year-round<br>- Support exercise recovery nutritionally |
| Mindset & Motivation | – Foster positive, confident mentality<br>- Set smaller achievable goal steps <br>- Enlist social support structure |
The most effective ACL/knee ligament injury prevention programs take a comprehensive approach. Optimizing strength, movement mechanics, loading, and nutrition helps create resilience. Confidence in knee stability paired with caution towards unsafe mechanics allows for safer progression. Expert guidance tailoring programs is key for best injury deterrence.

Key Takeaways
- Understanding the anatomy of the knee joint and identifying knee ligament injuries can promote quick recovery.
- Direct and indirect trauma can cause knee ligament injuries, leading to pain, swelling, inflammation, and joint laxity.
- Five prevention strategies can help maintain knee stability and prevent knee instability, reducing the risk of knee ligament injuries.
Understanding and Identifying Knee Ligament Injuries
Knee ligament injuries are common among athletes and individuals who engage in physical activities that require jumping, pivoting, or sudden changes in direction. In this section, we will discuss the common types and causes of knee ligament injuries, how to identify symptoms and diagnose the injury, treatment and rehabilitation options, and the role of sex and age in knee ligament injuries.
Common Types and Causes
The most common types of knee ligament injuries are the anterior cruciate ligament (ACL) and medial collateral ligament (MCL) injuries. The ACL is usually injured during non-contact activities such as landing after a jump or sudden stops and changes in direction. On the other hand, the MCL is usually injured from a direct blow to the outer side of the knee, such as when playing football or hockey.
Symptoms and Diagnosis
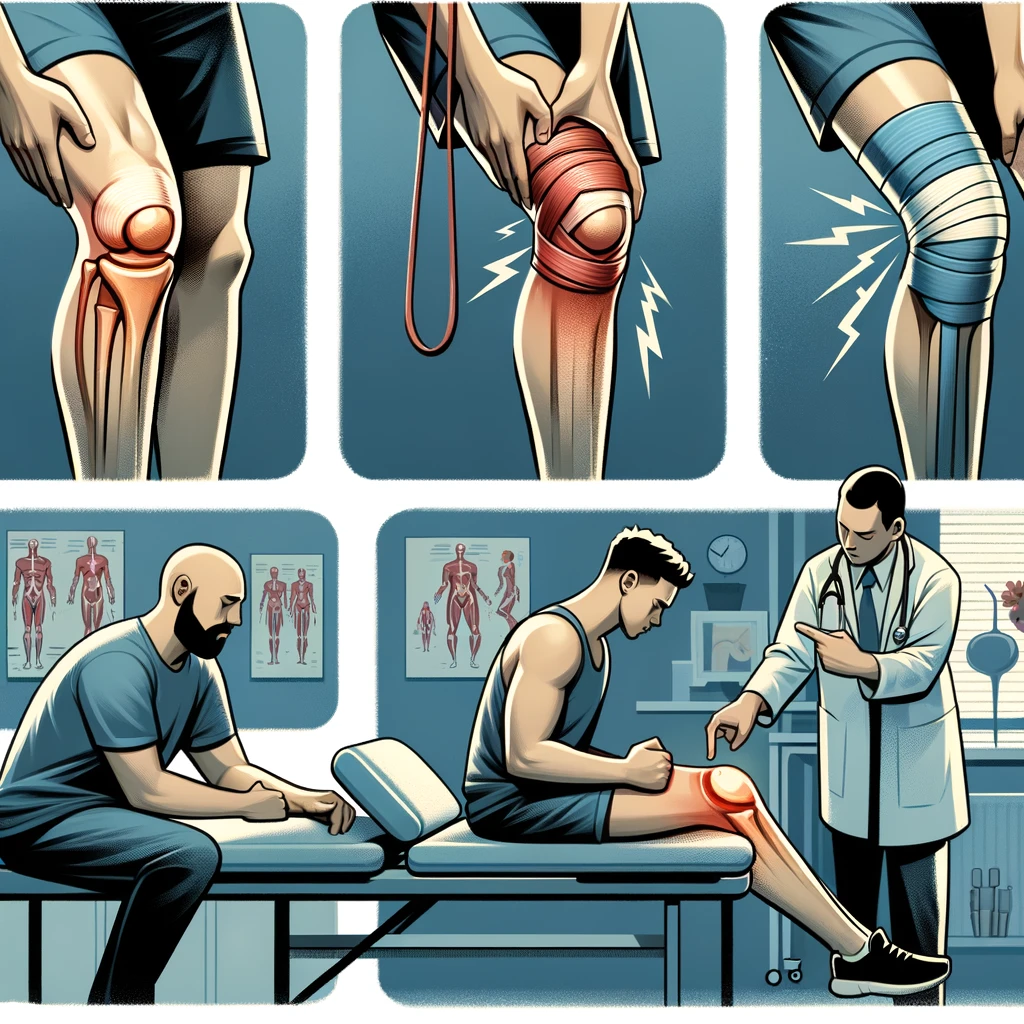
The symptoms of knee ligament injuries include pain, swelling, bruising, and instability. The diagnosis of knee ligament injuries is usually made through a physical exam and imaging tests such as MRI or X-rays. It is important to seek medical attention if you experience any of these symptoms.
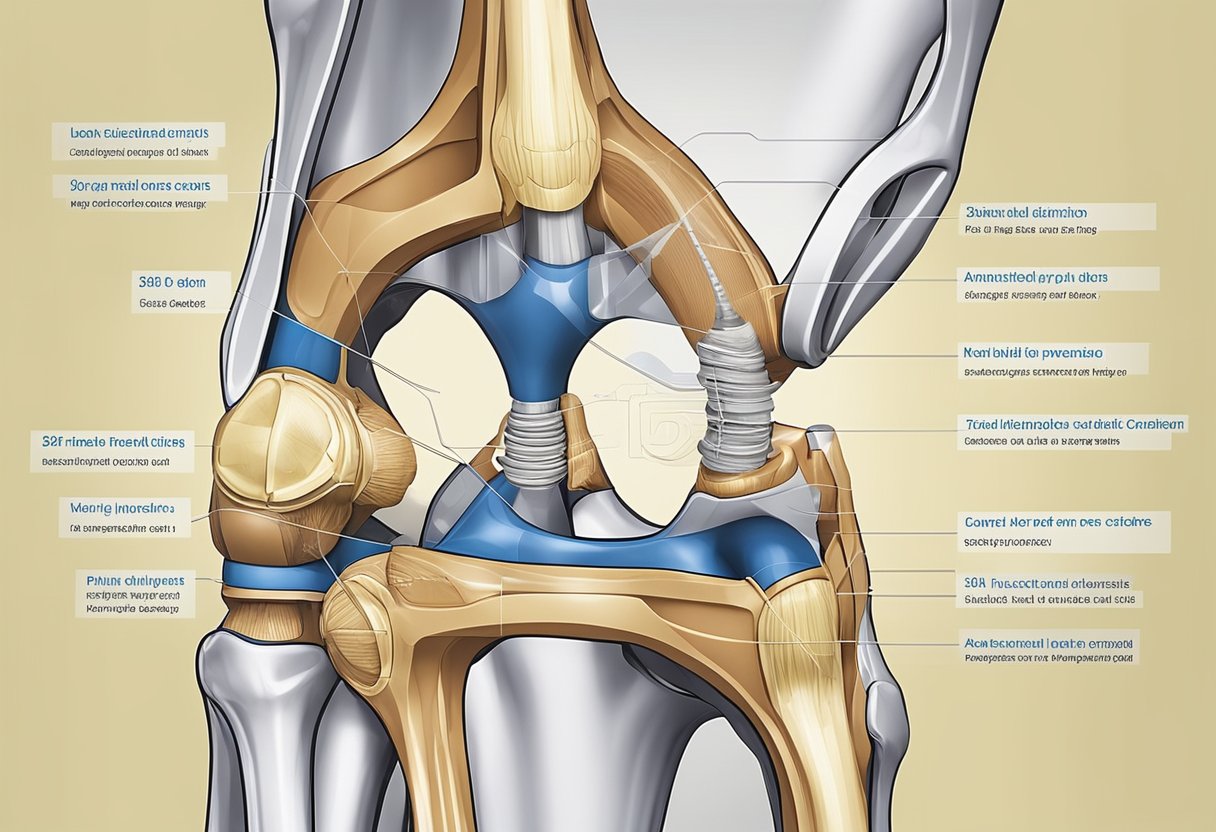
Treatment and Rehabilitation
The treatment and rehabilitation of knee ligament injuries depend on the severity of the injury. Treatment options include rest, ice, compression, and elevation (RICE), physical therapy, and surgery. Rehabilitation includes exercises to improve range of motion, strength, and mobility. It is important to follow the guidance of a physical therapist or orthopedic surgeon to ensure proper recovery.
Role of Sex and Age
Research shows that females are more prone to knee ligament injuries than males due to differences in anatomy, form, and hormones such as estrogen and relaxin. Additionally, age plays a role in knee ligament injuries, with individuals over 50 years old being at a higher risk due to decreased muscle strength and flexibility.
Sports and Injuries
Knee ligament injuries are common in sports that require sudden stops and changes in direction such as soccer, basketball, and football (soccer). Injury prevention programs that include warm-up, neuromuscular training, and proprioception exercises can reduce the frequency of knee ligament injuries by up to 50%. Coaches and athletes should also prioritize proper technique, posture, and fatigue management to prevent knee ligament injuries.
In conclusion, knee ligament injuries are common among athletes and individuals who engage in physical activities. Understanding the common types and causes of knee ligament injuries, identifying symptoms and diagnosing the injury, and following proper treatment and rehabilitation options can help prevent long-term damage. Coaches, athletes, and individuals should prioritize injury prevention programs and proper technique to reduce the frequency of knee ligament injuries.
Prevention Strategies for Knee Ligament Injuries
When it comes to knee ligament injuries, prevention is key. Here are some effective strategies that we recommend:
Strengthening and Conditioning
Strengthening and conditioning exercises can help improve muscle strength and endurance, which can help reduce the risk of knee ligament injuries. Exercises that target the hips, ankles, and core can be particularly effective in improving stability and reducing the risk of injury.
Injury Prevention Programs
Injury prevention programs can be an effective way to reduce the risk of knee ligament injuries. These programs typically include a combination of warm-up exercises, neuromuscular training, and strength and conditioning exercises. They can be particularly effective for athletes who participate in high-risk sports, such as soccer, basketball, and football.
Importance of Compliance and Frequency
Injury prevention strategies are only effective if they are followed consistently and frequently. Compliance with injury prevention programs is essential for reducing the risk of knee ligament injuries. It is important to follow the program as prescribed and to make sure that exercises are performed correctly and with good form.
In conclusion, preventing knee ligament injuries requires a combination of strategies that target strength, stability, and flexibility. Injury prevention programs that incorporate warm-up exercises, neuromuscular training, and strength and conditioning exercises can be particularly effective. However, compliance with these programs is essential for success. By following these strategies, we can help reduce the risk of knee ligament injuries and keep athletes healthy and active.