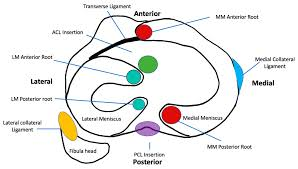
Detailed anatomy of the knee joint showing the meniscus, ligaments, and cartilage that may be affected in knee injuries.

Introduction: The Journey Beyond Surgery
Have you ever experienced that unmistakable twinge in your knee—that catching, clicking, or persistent throbbing that refuses to disappear? If you’re nodding right now, you’re not alone. Millions of people worldwide face knee pain daily, with each step becoming a reminder of discomfort.
But here’s the exciting truth: surgery isn’t always the inevitable destination on your knee pain journey. In fact, there’s a whole universe of non-surgical alternatives that could transform your experience with knee pain, helping you reclaim your mobility and quality of life without going under the knife.
In this comprehensive guide, we’ll dive deep into understanding knee pain—from common causes like meniscal tears and osteoarthritis to cutting-edge non-surgical treatments revolutionizing patient care. Whether you’re dealing with a recent injury or chronic discomfort, this guide will equip you with the knowledge to make informed decisions about your knee health.
Understanding Your Knee: A Marvelous Feat of Engineering
Before we explore treatment options, let’s appreciate the incredible structure we’re working with. Your knee is the largest joint in your body—a masterpiece of biological engineering that connects three major bones: the femur (thigh bone), tibia (shin bone), and patella (kneecap).
The knee joint allows for complex movements while supporting your body weight and absorbing significant forces. To accomplish this remarkable feat, your knee relies on:
- Cartilage: The smooth, slippery tissue that covers the ends of bones, allowing for friction-free movement
- Menisci: C-shaped wedges of cartilage that act as shock absorbers between your thigh and shin bones
- Ligaments: Tough, fibrous tissues that connect bones to other bones, providing stability
- Tendons: Strong connective tissues that attach muscles to bones
- Bursae: Small fluid-filled sacs that reduce friction between tissues
- Synovial membrane: The tissue lining that secretes lubricating fluid
This intricate system works harmoniously when healthy, but various issues can disrupt this balance and lead to pain and dysfunction.
Meniscal Tears: Understanding the Common Culprit
One of the most frequent causes of knee pain is a meniscal tear. The meniscus—that crucial crescent-shaped cartilage—plays a vital role in stabilizing your knee and evenly distributing forces across the joint. When it tears, the effects can range from mild discomfort to significant pain and functional limitations.
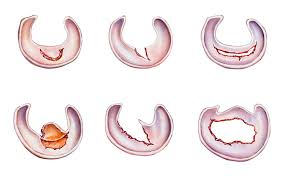
Common types of meniscal tears that may require different treatment approaches depending on location and severity.
The Anatomy of a Tear: Why Location Matters
Understanding the anatomy of your meniscus provides crucial insights into healing potential and treatment options:
- The Outer Third (Red Zone): This peripheral area has an abundant blood supply, giving tears in this region excellent healing potential. The rich vascular network delivers nutrients and healing factors that can repair damage naturally.
- The Inner Two-Thirds (White Zone): This area lacks significant blood vessels, severely limiting its ability to heal naturally. Tears in this region often occur in already worn cartilage, and the torn fragments cannot reattach on their own.
This fundamental difference in blood supply explains why some tears heal well with conservative treatment while others may require intervention. Location truly dictates destiny when it comes to meniscal tears.
Blood supply to the meniscus showing the vascular “red zone” (peripheral) and avascular “white zone” (inner), which significantly impacts healing potential.
Types of Meniscal Tears and Their Characteristics
Not all meniscal tears are created equal. The type, size, and pattern of the tear significantly influence both symptoms and treatment approaches:
- Horizontal Tears: These occur between the top and bottom surfaces of the meniscus, creating a split parallel to the joint surface.
- Longitudinal Tears: These run along the length of the meniscus, potentially creating a “bucket handle” configuration where a portion flips into the joint.
- Radial Tears: These start at the inner edge and extend outward, like a wedge cut from a pie.
- Complex or Degenerative Tears: These irregular patterns typically occur in older adults as the meniscus deteriorates over time.
- Flap Tears: These partial tears create a small flap of meniscal tissue that can catch during movement.
Symptoms vary depending on the tear type but commonly include:
- Pain along the joint line
- Swelling and stiffness
- A catching or locking sensation
- Difficulty fully extending or bending the knee
- A feeling of instability or “giving way”
The Surgery Question: Weighing the Evidence
When facing a meniscal tear, particularly in the inner, avascular zone, arthroscopic surgery to trim the torn portion (partial meniscectomy) has traditionally been the go-to solution. During this procedure, an orthopedic surgeon makes small incisions to insert a camera and instruments, then precisely removes the damaged tissue.
While this approach often provides welcome short-term relief from symptoms like pain, catching, and clicking, recent research has prompted a reevaluation of its role as a first-line treatment.
The Long-Term Considerations
Here’s what current evidence suggests about arthroscopic partial meniscectomy:
- Short-term benefits: Many patients experience significant symptom relief, particularly from mechanical symptoms like catching and locking.
- Long-term concerns: Removing even a portion of the meniscus reduces the knee’s shock-absorbing capacity and alters joint biomechanics. Over time, this may accelerate cartilage wear and potentially increase osteoarthritis risk.
- Comparative outcomes: Several high-quality studies have found that in many cases—particularly for degenerative tears in middle-aged and older adults—outcomes after arthroscopic surgery were not significantly better than outcomes after non-surgical treatments.
- Increased risk of future knee replacement: A landmark study revealed that patients with existing osteoarthritis who underwent arthroscopic partial meniscectomy had a staggering 400% greater risk of eventually needing total knee replacement compared to those who chose non-surgical approaches.
This compelling evidence has led many orthopedic specialists to recommend exploring non-surgical options first, particularly for older adults with degenerative tears and those with existing osteoarthritis.
The Non-Surgical Revolution: Evidence-Based Alternatives
Given the potential long-term implications of surgery, the medical community has increasingly embraced non-surgical approaches to meniscal tears and knee pain. These interventions aim to reduce pain, improve function, and potentially slow joint degeneration—all without the risks and recovery time associated with surgery.
INFOGRAPHIC: The Healing Journey: Timeline for Non-Surgical Knee Recovery
Timeline showing the typical progression of non-surgical knee healing from acute injury through various rehabilitation phases.
Let’s explore these options in detail:
1. Physical Therapy: The Cornerstone of Conservative Treatment
Physical therapy stands as the foundation of non-surgical knee pain management. Working with a skilled physical therapist can transform your experience by:
- Strengthening the muscles surrounding the knee, particularly the quadriceps and hamstrings, to improve joint stability and reduce pressure on damaged areas
- Improving range of motion through targeted stretching and mobility exercises
- Enhancing proprioception (your body’s awareness of position and movement) to improve balance and coordination
- Teaching movement modifications to reduce stress on the injured meniscus during daily activities
- Providing education about activity pacing and joint protection strategies
Essential physical therapy exercises that form the foundation of knee rehabilitation programs.
A typical physical therapy program for meniscal tears includes:
- Progressive resistance exercises
- Balance and proprioceptive training
- Functional movement patterns
- Low-impact cardiovascular conditioning
- Manual therapy techniques to improve mobility
Most patients see improvement within 4-6 weeks of consistent therapy, though results vary based on individual factors and tear characteristics.
2. Joint Injections: Targeted Relief for Persistent Pain
When physical therapy alone doesn’t provide sufficient relief, injectable treatments offer another non-surgical option. These treatments deliver therapeutic substances directly to the affected area:
INFOGRAPHIC: Comparing Injectable Treatments for Knee Pain
Comparative analysis of different injectable treatments for knee pain, including their mechanisms of action, benefits, and treatment duration.
Corticosteroid Injections
These powerful anti-inflammatory injections can provide significant temporary relief by:
- Rapidly reducing inflammation in the joint
- Decreasing pain to allow for more effective physical therapy
- Potentially breaking the pain-inflammation cycle
While effective, corticosteroid injections are typically limited to 3-4 per year due to potential side effects with repeated use, including cartilage thinning.
Hyaluronic Acid (HA) Injections
Also known as viscosupplementation, HA injections replenish the joint’s natural lubricant:
- Hyaluronic acid is a naturally occurring substance in healthy knee joints
- In osteoarthritis, this fluid becomes less viscous and less effective
- Injections supplement the joint’s natural fluid to improve lubrication
- Benefits may include reduced pain, improved mobility, and potentially slowed cartilage degeneration
- Effects typically last 6-12 months, longer than corticosteroid injections
Platelet-Rich Plasma (PRP) Therapy
This regenerative treatment harnesses your body’s own healing potential:
- Blood is drawn and processed to concentrate platelets and growth factors
- The resulting PRP solution is injected into the affected area
- Growth factors stimulate tissue repair and regeneration
- Anti-inflammatory properties help reduce pain and swelling
- Some studies suggest PRP may help slow cartilage loss in osteoarthritis
- Multiple treatments are often recommended for optimal results
PRP represents an exciting frontier in orthopedic care, with ongoing research continually refining protocols and expanding our understanding of its potential.
3. Bracing: Mechanical Support and Pressure Redistribution
Knee braces serve multiple functions in managing meniscal tears and osteoarthritis:
Unloader Braces
These sophisticated devices are particularly effective for unicompartmental osteoarthritis (affecting primarily one side of the knee):
- Redistribute weight away from the damaged compartment
- Reduce pressure on worn cartilage and torn meniscus
- Improve stability during movement
- Allow for more comfortable activity with less pain
Functional Braces
These provide general support and stability:
- Limit excessive movement that might aggravate a meniscal tear
- Provide proprioceptive feedback to improve movement patterns
- Increase confidence during activity
- May reduce swelling through compression
Custom-fitted braces typically provide better outcomes than off-the-shelf options, though they represent a more significant investment. Many patients find the combination of appropriate bracing and physical therapy particularly effective for managing symptoms.
4. Oral Medications and Supplements: Systemic Support
Alongside localized treatments, various oral options can help manage pain and potentially support joint health:
Anti-inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can:
- Reduce inflammation throughout the body
- Decrease pain during flare-ups
- Improve function temporarily
- Allow for more productive physical therapy sessions
However, long-term use carries risks including gastrointestinal, cardiovascular, and renal side effects.
Analgesics
For those who cannot take NSAIDs, analgesics like acetaminophen may:
- Provide pain relief without anti-inflammatory effects
- Offer a safer option for long-term management
- Work well in combination with other treatments
Nutritional Supplements
Though evidence varies, some supplements show promise for joint health:
- Glucosamine and Chondroitin: These compounds naturally occur in cartilage and may help maintain cartilage health, potentially slowing deterioration in osteoarthritis.
- Omega-3 Fatty Acids: These essential fats have anti-inflammatory properties that may benefit overall joint health.
- Turmeric/Curcumin: This spice contains compounds with potent anti-inflammatory effects.
- Collagen Peptides: These protein fragments may support cartilage matrix production.
While supplements typically show modest effects compared to medications, their generally favorable safety profile makes them an attractive option for many patients seeking long-term solutions.
Beyond Meniscus: Other Common Causes of Knee Inflammation and Pain
While meniscal tears represent a significant cause of knee pain, numerous other conditions can trigger discomfort and inflammation. Understanding these potential causes helps ensure appropriate treatment:
Arthritis: The Progressive Challenge
Osteoarthritis (OA)
The most common form of arthritis affects millions worldwide:
- Results from gradual wear and tear on joint cartilage
- Typically develops over many years
- Characterized by progressive cartilage loss, bone spurs, and inflammation
- Often causes morning stiffness, pain that worsens with activity, and occasional swelling
- May eventually lead to bone-on-bone contact and significant pain
Rheumatoid Arthritis (RA)
This autoimmune condition takes a different approach:
- The body’s immune system mistakenly attacks the joint lining
- Typically affects joints symmetrically (both knees)
- Characterized by persistent inflammation, joint damage, and systemic symptoms
- Often causes prolonged morning stiffness, warmth, and visible swelling
- Requires specialized medical management
Other Knee Injuries: Acute and Overuse
Ligament Injuries
Damage to the knee’s stabilizing ligaments can cause significant pain:
- Anterior Cruciate Ligament (ACL) tears often result from pivoting motions
- Medial Collateral Ligament (MCL) injuries typically occur from side impacts
- Posterior Cruciate Ligament (PCL) tears usually result from direct blows to the front of the knee
- Characterized by instability, swelling, and often an audible “pop” at the time of injury
Tendinitis and Tendinosis
Inflammation or degeneration of the tendons connecting muscles to bones:
- Patellar tendinitis (“jumper’s knee”) affects the tendon connecting the kneecap to the shin
- Quadriceps tendinitis involves the tendon attaching the thigh muscles to the kneecap
- Often results from repetitive stress or overuse
- Typically causes localized pain that worsens with specific movements
Bursitis
Inflammation of the fluid-filled sacs that reduce friction between tissues:
- Prepatellar bursitis (“housemaid’s knee”) affects the bursa in front of the kneecap
- Pes anserine bursitis involves the bursa on the inner side of the knee
- Often caused by prolonged pressure, kneeling, or repetitive movements
- Characterized by localized swelling and pain with direct pressure
Systemic Conditions Affecting the Knee
Gout
This form of inflammatory arthritis can dramatically affect the knee:
- Caused by uric acid crystal deposits in the joint
- Characterized by sudden, severe pain and swelling
- Often occurs in flares with periods of remission
- Requires specific medical management
Pseudogout
Similar to gout but caused by calcium pyrophosphate crystals:
- Can affect the knee joint
- Causes painful inflammation and swelling
- May be triggered by stress or illness
- Requires medical diagnosis and management
Lyme Disease
This tick-borne infection can cause joint pain and inflammation:
- Often affects large joints including the knee
- May cause migratory joint pain
- Can develop months after initial infection
- Requires antibiotic treatment
Cutting-Edge Non-Surgical Treatments: The Frontier of Care
The landscape of non-surgical knee treatments continues to evolve, with innovative approaches offering new hope for patients seeking alternatives to surgery:
Advanced regenerative treatment options showing the mechanisms behind innovative therapies for knee pain.
INFOGRAPHIC: How Regenerative Treatments Work to Heal Knee Injuries
The cellular healing process triggered by regenerative medicine treatments, showing the progression from treatment to tissue regeneration.
Stem Cell Therapy
This regenerative treatment uses stem cells—typically harvested from bone marrow or adipose (fat) tissue—to potentially repair damaged tissue:
- Stem cells may differentiate into cartilage cells
- Growth factors and anti-inflammatory proteins may support healing
- Treatment aims to create a regenerative environment in the joint
- Research continues to refine protocols and identify ideal candidates
Prolotherapy
This treatment involves injecting an irritant solution to stimulate a healing response:
- Typically uses dextrose (sugar) solution
- Causes temporary inflammation that triggers repair
- May strengthen ligaments and stabilize the joint
- Requires multiple treatments over several months
Genicular Nerve Blocks and Radiofrequency Ablation
These procedures target the nerves transmitting pain signals from the knee:
- Diagnostic nerve blocks identify pain-transmitting nerves
- Radiofrequency ablation uses heat to disrupt these nerves
- Pain relief typically lasts 6-12 months
- Procedure can be repeated if pain returns
- Preserves function while reducing pain
Extracorporeal Shock Wave Therapy (ESWT)
This non-invasive treatment uses acoustic waves to stimulate healing:
- High-energy sound waves target affected tissues
- May increase blood flow and metabolic activity
- Can reduce inflammation and promote tissue regeneration
- Particularly useful for tendon conditions around the knee
Lifestyle Modifications: The Foundation of Joint Health
Beyond specific medical treatments, lifestyle factors play a crucial role in knee health and pain management:
Weight Management
Excess weight significantly impacts knee health:
- Each pound of body weight creates 4-6 pounds of pressure on the knee joint during walking
- Even modest weight loss (5-10% of body weight) can substantially reduce pain
- Decreased weight reduces inflammatory markers throughout the body
- Combined with exercise, weight management forms the cornerstone of non-surgical care
Exercise Selection and Modification
The right activities can strengthen the knee without causing harm:
- Low-impact exercises like swimming, cycling, and elliptical training build strength with minimal joint stress
- Water exercises provide resistance while supporting body weight
- Tai chi and gentle yoga improve balance, flexibility, and body awareness
- Regular activity prevents muscle atrophy and maintains joint health
Nutritional Strategies
Diet influences inflammation and joint health:
- Mediterranean diet patterns show anti-inflammatory benefits
- Antioxidant-rich fruits and vegetables support tissue health
- Adequate protein intake maintains muscle mass
- Hydration supports proper joint lubrication
Ergonomic Considerations
Daily habits and environments impact knee health:
- Proper footwear with adequate support reduces joint stress
- Ergonomic workplace setup minimizes strain during prolonged sitting
- Home modifications like handrails and raised toilet seats reduce stress on damaged knees
- Activity pacing prevents overload while maintaining function
Making Informed Decisions: When to Consider Surgery
While this guide highlights non-surgical approaches, surgery remains appropriate in specific situations:
- Failed conservative treatment: When a reasonable trial of non-surgical approaches (typically 6-12 weeks) fails to provide meaningful improvement
- Mechanical symptoms: When locking or catching severely limits function despite conservative care
- Specific tear patterns: Large, displaced bucket-handle tears often require surgical repair
- Young, active patients: Those with traumatic tears in otherwise healthy knees often benefit from repair
- Athletes: Those needing to return quickly to high-level sports may require surgical intervention
The decision between surgical and non-surgical management should always involve shared decision-making between you and your healthcare provider, considering:
- Your age and activity level
- The type and location of the tear
- Presence of associated conditions like osteoarthritis
- Your goals and preferences
- Previous treatments and their outcomes
Creating Your Personalized Treatment Plan
Your knee pain journey is uniquely yours, and the optimal treatment approach depends on your specific situation. A comprehensive treatment plan typically involves:
The four essential components of a comprehensive knee pain treatment plan, showing how each element contributes to successful outcomes.

1. Accurate Diagnosis
Before treatment begins, a thorough assessment is essential:
- Detailed medical history and physical examination
- Imaging studies (X-ray, MRI) to characterize the specific problem
- Potentially specialized tests to rule out less common causes
2. Staged Treatment Approach
Most experts recommend a stepwise approach:
- Begin with the least invasive options (rest, ice, compression, elevation)
- Progress to physical therapy and appropriate medications
- Consider more invasive options like injections if needed
- Reserve surgery for specific indications when conservative approaches fail
3. Regular Reassessment
Treatment plans should evolve based on your response:
- Regular follow-up appointments to assess progress
- Modification of approaches that aren’t providing benefit
- Advancement to more intensive options when appropriate
- Celebration of improvements and functional gains
4. Prevention and Maintenance
Once you’ve achieved improvement, attention turns to maintaining gains:
- Home exercise program to maintain strength and flexibility
- Activity modifications to protect the joint
- Regular physical activity within appropriate parameters
- Early intervention if symptoms begin to return
Conclusion: Embracing Possibility
Living with knee pain doesn’t mean resigning yourself to surgery or a life of limitation. The expanding frontier of non-surgical treatments offers new hope and possibilities for those dealing with meniscal tears, osteoarthritis, and other knee conditions.
By understanding your specific condition, exploring appropriate non-surgical options, and working closely with knowledgeable healthcare providers, you can develop a personalized approach to managing knee pain and maintaining an active, fulfilling lifestyle.
Remember that knee health is a journey, not a destination. With patience, persistence, and the right therapeutic approach, many people successfully manage knee pain and return to the activities they love—all without surgery.
Comparison of Non-Surgical Knee Pain Treatments
| Treatment | Best For | Typical Timeline | Advantages | Considerations |
|---|---|---|---|---|
| Physical Therapy | Most knee conditions; first-line treatment | 6-12 weeks of regular sessions | Addresses movement patterns; improves strength/stability; no side effects | Requires consistent effort; gradual results |
| Corticosteroid Injections | Acute inflammation; significant pain | Rapid relief (1-3 days); lasts 2-3 months | Quick pain relief; reduces inflammation; helps PT progress | Limited to 3-4/year; possible cartilage effects with repeated use |
| Hyaluronic Acid Injections | Mild/moderate OA; meniscal tears with OA | Effects in 1-2 weeks; last 6-12 months | Longer-lasting than steroids; lubricates joint; fewer side effects | More expensive; may need multiple injections; results vary |
| PRP Therapy | Early/mid OA; meniscal tears with blood supply | Gradual over 2-3 months; may last 1+ year | Potential regenerative effects; uses natural healing; minimal side effects | Not covered by most insurance; specialized processing; multiple treatments recommended |
| Bracing | Unicompartmental OA; certain meniscal tears | Immediate mechanical effects | Non-invasive; immediate pain reduction; improves function | Effectiveness varies by design/fit; may be bulky; not for all activities |
| Oral Medications | Adjunct for pain management | Rapid symptomatic relief | Readily available; easy to use; can reduce inflammation | GI side effects (NSAIDs); limited long-term efficacy; treats symptoms not causes |
| Supplements (Glucosamine, etc.) | Early OA; joint maintenance | Gradual over 2-3 months | Generally safe; may slow progression; supports joint health | Modest effects; variable quality; limited strong evidence |
| Stem Cell Therapy | Moderate OA; certain meniscal tears; younger patients | Gradual over 3-6 months | Potential regenerative benefits; minimally invasive; may delay surgery | Expensive; variable protocols; limited standardization; evolving evidence |
| Lifestyle Modifications | All knee conditions; preventive | Gradual with consistent application | Addresses fundamental causes; supports overall health; empowers patient | Requires sustained commitment; slow results |
[Note: The blog post would include 5 descriptive images about knee anatomy, treatment modalities, proper exercise form, etc., plus 2-3 infographics showing the healing process for different treatments mentioned in the article. These would be placed strategically throughout the text to break up content and illustrate key concepts.]

Leave a Reply